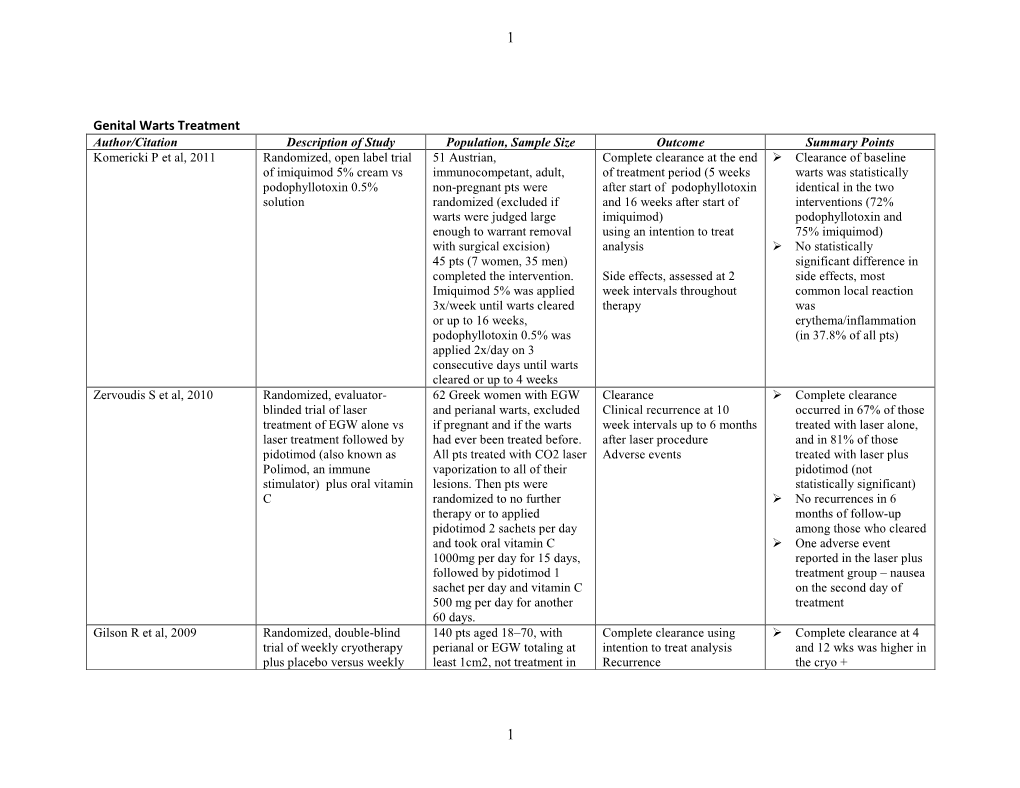
HPV Genital Warts Treatment Tables of Evidence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
(12) United States Patent (10) Patent No.: US 8,993,581 B2 Perrine Et Al
US00899.3581B2 (12) United States Patent (10) Patent No.: US 8,993,581 B2 Perrine et al. (45) Date of Patent: Mar. 31, 2015 (54) METHODS FOR TREATINGVIRAL (58) Field of Classification Search DSORDERS CPC ... A61K 31/00; A61K 31/166; A61K 31/185: A61K 31/233; A61K 31/522: A61K 38/12: (71) Applicant: Trustees of Boston University, Boston, A61K 38/15: A61K 45/06 MA (US) USPC ........... 514/263.38, 21.1, 557, 565, 575, 617; 424/2011 (72) Inventors: Susan Perrine, Weston, MA (US); Douglas Faller, Weston, MA (US) See application file for complete search history. (73) Assignee: Trustees of Boston University, Boston, (56) References Cited MA (US) U.S. PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this 3,471,513 A 10, 1969 Chinn et al. patent is extended or adjusted under 35 3,904,612 A 9/1975 Nagasawa et al. U.S.C. 154(b) by 0 days. (Continued) (21) Appl. No.: 13/915,092 FOREIGN PATENT DOCUMENTS (22) Filed: Jun. 11, 2013 CA 1209037 A 8, 1986 CA 2303268 A1 4f1995 (65) Prior Publication Data (Continued) US 2014/OO45774 A1 Feb. 13, 2014 OTHER PUBLICATIONS Related U.S. Application Data (63) Continuation of application No. 12/890,042, filed on PCT/US 10/59584 Search Report and Written Opinion mailed Feb. Sep. 24, 2010, now abandoned. 11, 2011. (Continued) (60) Provisional application No. 61/245,529, filed on Sep. 24, 2009, provisional application No. 61/295,663, filed on Jan. 15, 2010. Primary Examiner — Savitha Rao (74) Attorney, Agent, or Firm — Nixon Peabody LLP (51) Int. -

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

Review of Sezary Syndrome
REVIEWS Sezary syndrome: Immunopathogenesis, literature review of therapeutic options, and recommendations for therapy by the United States Cutaneous Lymphoma Consortium (USCLC) EliseA.Olsen,MD,a Alain H. Rook, MD,b John Zic, MD,c Youn Kim, MD,d PierluigiPorcu,MD,e Christiane Querfeld, MD,f Gary Wood, MD,g Marie-France Demierre, MD,h Mark Pittelkow, MD,i Lynn D. Wilson, MD, MPH,j Lauren Pinter-Brown, MD,k Ranjana Advani, MD,d Sareeta Parker, MD,l Ellen J. Kim, MD,b Jacqueline M. Junkins-Hopkins, MD,m Francine Foss, MD,j Patrick Cacchio, BS,a and Madeleine Duvic, MDn Durham, North Carolina; Philadelphia, Pennsylvania; Nashville, Tennessee; Palo Alto and Los Angeles, California; Columbus, Ohio; Chicago, Illinois;Madison,Wisconsin;Boston,Massachusetts; Rochester, Minnesota; New Haven, Connecticut; Atlanta, Georgia; Baltimore, Maryland; and Houston, Texas Sezary syndrome (SS) has a poor prognosis and few guidelines for optimizing therapy. The US Cutaneous Lymphoma Consortium, to improve clinical care of patients with SS and encourage controlled clinical trials of promising treatments, undertook a review of the published literature on therapeutic options for SS. An overview of the immunopathogenesis and standardized review of potential current treatment options for SS including metabolism, mechanism of action, overall efficacy in mycosis fungoides and SS, and common or concerning adverse effects is first discussed. The specific efficacy of each treatment for SS, both as monotherapy and combination therapy, is then reported using standardized criteria for both SS and response to therapy with the type of study defined by a modification of the US Preventive Services guidelines for evidence-based medicine. -

Condylomata Acuminata of the Penis and Scrotum Case Report and Literature Review
World Journal of Research and Review (WJRR) ISSN:2455-3956, Volume-8, Issue-1, January 2019 Pages 07-09 Condylomata Acuminata of the Penis and Scrotum Case Report and Literature Review Otei Otei O. O, Ozinko M, Ekpo R, Egiehiokhin Isiwere, Nabie N.F same Hospital with a histological diagnosis of Abstract— The case of an affected 36-year old male and Condylomata Acuminata following a history of multiple review of relevant literature which utilize to highlight the scrotal and penile swellings of 10 year duration and the diagnostic and management challenges of this case. The patient challenges faced in the management of the condition. was initially received medical treatment at the Dermatology CASE REPORT Clinic of the University Calabar. The latter was not successful and the patient was referred to the Burns and Plastic Surgery A 36 year old married Driver was referred from Unit of the same hospital where scrotal sac excision, flap cover dermatology clinic to the Surgical outpatient Department of and electrocautery were done. This treatment was successful the University of Calabar Teaching Hospital, Calabar with a but there was mild penile contracture and we intend to follow histological diagnosis of Condylomata Acuminata of the up patient closely for early detection and treatment of Penis and Scrotum following a history of multiple recurrence. peno-scrotal swellings of 10 years duration. BACKGROUND A swelling was first noticed as a hard painful boil on his Condylomata Acuminata or genital wart refers to the epidermal manifestation attributed to the epidermotropic left inguinal region . Multiple swellings appeared in the same Human Papiloma Virus (HPV) particularly types 6 and 11 . -

Efficacy and Safety of Imiquimod for Verruca Planae: a Systematic Review
Global Dermatology Research Article ISSN: 2056-7863 Efficacy and safety of imiquimod for verruca planae: A systematic review Xin-rui Zhang#, Bi-huan Xiao#, Rui-qun Qi*, and Xing-hua Gao* Department of Dermatology, No 1 Hospital of China Medical University, Shenyang 110001, PR China #These authors contributed equally to this work Abstract Objective: To assess the efficacy and safety of imiquimod for treating verruca planae. Methods: We searched the Pubmed, Cochrane Register of Controlled Trials, EMbase, CBM, CNKI and Wanfang databases (Chinese) to collect randomized controlled trials (RCTs). We screened the retrieved studies according to the predefined inclusion and exclusion criteria, evaluated the quality of include studies, and performed meta-analyses using the Cochrane Collaboration’s RevMan 5.1. Software. Results: Twenty-six RCTs involving 2169 patients with verruca planae were included and assessed. At the end of the 6th and ≥8th week, the effective rate of topical imiquimod was obviously higher than that of control [ RR=1.42, 95%CI (1.27, 1.60), P <0.00001; RR=1.43, 95%CI (1.22,1.67), P<0.00001]. The effective rate of imiquimod cream was higher than tretinoin cream, tazarotene gel and other antiviral drugs. [RR=1.41, 95%CI (1.25, 1.59), P <0.00001; RR=1.76, 95%CI (1.48, 2.10), P<0.00001; RR=1.71, 95%CI (1.29, 2.26), P =0.0002]. However, the effectiverate of imiquimod cream was lower than 5-ALA-PDT (RR=0.6, 95%CI (0.5, 0.71), P<0.00001). Conclusions: The limited evidence demonstrates that topical imiquimod is safe and efficient. -

Treating the Oral Creeper: Herpes
ISSN: 2574-1241 Volume 5- Issue 4: 2018 DOI: 10.26717/BJSTR.2018.08.001639 Karthik D Yadav. Biomed J Sci & Tech Res Short Communication Open Access Treating the Oral Creeper: Herpes Yadav Karthik D1*, Pai Anuradha2, R Shesha Prasad3, Yaji Anisha4 1M.D.S - Master of Dental surgery, Department of oral medicine and radiology, Bangalore 2HOD & Professor, Department of oral medicine and radiology, The oxford dental college and research center, Bangalore 3M.D.S - Master of Dental surgery, Department of oral medicine and radiology, Senior lecturer, The oxford dental college and research center, Bangalore 4M.D.S – Master of Dental surgery, Department of oral medicine and radiology, Bangalore Received: August 19, 2018; Published: August 24, 2018 *Corresponding author: Karthik D Yadav, 10th Milestone, Bommanahalli, Hosur Road, Bangalore-560 102, India Short Communication combination of all these drugs is more effective in treating HSV The term “herpes” creates panic among the general population. infections than the anesthetic preparations alone. They are also Oral herpes simplex virus is most commonly seen affecting the oral soft tissue region the perioral area [1,2]. They have been categorized treating HSV. Further, ice can be used and lip materials containing into HSV -1 and HSV -2, wherein HSV-1 affects the orofacial region, used with systemic antiviral agents for increased efficacy while cocoa, lanolin and petroleum products have been recommended to most commonly above the waist region and HSV-2 affects the treat recurrent herpes [6]. genital region below the waist. However, change in sexual practices have been the basis for the variations of the virus, affecting the While the use of topical drugs has few adverse effects and are non-conventional regions of the body [3,4]. -

The Phytochemistry of Cherokee Aromatic Medicinal Plants
medicines Review The Phytochemistry of Cherokee Aromatic Medicinal Plants William N. Setzer 1,2 1 Department of Chemistry, University of Alabama in Huntsville, Huntsville, AL 35899, USA; [email protected]; Tel.: +1-256-824-6519 2 Aromatic Plant Research Center, 230 N 1200 E, Suite 102, Lehi, UT 84043, USA Received: 25 October 2018; Accepted: 8 November 2018; Published: 12 November 2018 Abstract: Background: Native Americans have had a rich ethnobotanical heritage for treating diseases, ailments, and injuries. Cherokee traditional medicine has provided numerous aromatic and medicinal plants that not only were used by the Cherokee people, but were also adopted for use by European settlers in North America. Methods: The aim of this review was to examine the Cherokee ethnobotanical literature and the published phytochemical investigations on Cherokee medicinal plants and to correlate phytochemical constituents with traditional uses and biological activities. Results: Several Cherokee medicinal plants are still in use today as herbal medicines, including, for example, yarrow (Achillea millefolium), black cohosh (Cimicifuga racemosa), American ginseng (Panax quinquefolius), and blue skullcap (Scutellaria lateriflora). This review presents a summary of the traditional uses, phytochemical constituents, and biological activities of Cherokee aromatic and medicinal plants. Conclusions: The list is not complete, however, as there is still much work needed in phytochemical investigation and pharmacological evaluation of many traditional herbal medicines. Keywords: Cherokee; Native American; traditional herbal medicine; chemical constituents; pharmacology 1. Introduction Natural products have been an important source of medicinal agents throughout history and modern medicine continues to rely on traditional knowledge for treatment of human maladies [1]. Traditional medicines such as Traditional Chinese Medicine [2], Ayurvedic [3], and medicinal plants from Latin America [4] have proven to be rich resources of biologically active compounds and potential new drugs. -

Herpes Simplex Virus
HSV Herpes simplex virus HSV (Herpes simplex virus) can be spread when an infected person is producing and shedding the virus. Herpes simplex can be spread through contact with saliva, such as sharing drinks. Symptoms of herpes simplex virus infection include watery blisters in the skin or mucous membranes of the mouth, lips or genitals. Lesions heal with ascab characteristic of herpetic disease. As neurotropic and neuroinvasive viruses, HSV-1 and -2 persist in the body by becoming latent and hiding from the immune system in the cell bodies of neurons. After the initial or primary infection, some infected people experience sporadic episodes of viral reactivation or outbreaks. www.MedChemExpress.com 1 HSV Inhibitors (Z)-Capsaicin 1-Docosanol (Zucapsaicin; Civamide; cis-Capsaicin) Cat. No.: HY-B1583 (Behenyl alcohol) Cat. No.: HY-B0222 (Z)-Capsaicin is the cis isomer of capsaicin, acts 1-Docosanol is a saturated fatty alcohol used as an orally active TRPV1 agonist, and is used in traditionally as an emollient, emulsifier, and the research of neuropathic pain. thickener in cosmetics, and nutritional supplement; inhibitor of lipid-enveloped viruses including herpes simplex. Purity: 99.96% Purity: ≥98.0% Clinical Data: Launched Clinical Data: Launched Size: 10 mM × 1 mL, 10 mg, 50 mg Size: 500 mg 2-Deoxy-D-glucose 20(R)-Ginsenoside Rh2 (2-DG; 2-Deoxy-D-arabino-hexose; D-Arabino-2-deoxyhexose) Cat. No.: HY-13966 Cat. No.: HY-N1401 2-Deoxy-D-glucose is a glucose analog that acts as 20(R)-Ginsenoside Rh2, a matrix a competitive inhibitor of glucose metabolism, metalloproteinase (MMP) inhibitor, acts as a inhibiting glycolysis via its actions on hexokinase. -

View/Download
Research Article Research Article Dermatology Research Therapy with Pegylated Interferon or Combined with Cryosurgery in Condyloma Acuminata. Phase III Clinical Trial Israel Alfonso Trujillo*, Tomás Tabilo Bocic, Ángela Rosa Gutiérrez Rojas, Hugo Nodarse Cuní, María Elena Flores Andrade, and María del Carmen Toledo García *Correspondence: Israel Alfonso-Trujillo, Calzada of Managua # 1133 e/Caimán and Quemados. Las Guásimas. Arroyo Naranjo, Havana, Cuba, E-mail: Surgical Clinical Hospital: "Hermanos Ameijeiras", Cuba. [email protected] Received: 04 January 2019; Accepted: 18 February 2019 Citation: Israel Alfonso Trujillo, Tomás Tabilo Bocic, Ángela Rosa Gutiérrez Rojas, et al. Therapy with Pegylated Interferon or Combined with Cryosurgery in Condyloma Acuminata. Phase III Clinical Trial. Dermatol Res. 2019; 1(1); 1-8. ABSTRACT Background: The continuous recurrence of condyloma acuminata makes the constant search for necessary therapeutic alternatives. Patients and method: To evaluate the therapeutic efficacy and safety of pegylated interferon, alone or adjuvant for cryosurgery, in the condyloma acuminata an open clinical trial was carried out on 30 patients of the "Hermanos Ameijeiras" hospital, who were randomized to receive for 6 weeks (group A) only fortnightly cryosurgery, (group B) subcutaneous pegylated interferon, once a week, associated with fortnightly cryosurgery application or (group C) only subcutaneous pegylated interferon, once a week. The main variable was the percentage of recurrence at one year of follow-up, evaluated quarterly. There was also a rigorous control of adverse events. Results: At the end of the treatment 8/10 (80%) patients from group A, 10/10 (100%) from group B and 9/10 (90%) from group C were left without injuries. -

Belayachi Et Al., Afr J Tradit Complement Altern Med. (2017) 14(2):356-373 Doi:10.21010/Ajtcam.V14i2.37
Belayachi et al., Afr J Tradit Complement Altern Med. (2017) 14(2):356-373 doi:10.21010/ajtcam.v14i2.37 INDUCTION OF CELL CYCLE ARREST AND APOPTOSIS BY ORMENIS ERIOLEPIS A MORROCAN ENDEMIC PLANT IN VARIOUS HUMAN CANCER CELL LINES Lamiae Belayachia,b*, Clara Aceves-Luquerob, Nawel Merghoubd, Silvia Fernández de Mattosb,c, Saaïd a b,c a Amzazi , Priam Villalonga ,Youssef Bakri a Biochemistry-Immunology Laboratory, Faculty of Sciences, Mohammed V-Agdal University, Rabat, Morocco, b Cancer Cell Biology Group, Institut Universitari d’Investigació en Ciències de la Salut (IUNICS), c Departament de Biologia Fonamental, Universitat de les Illes Balears, Illes Balears, Spain, Green Biotechnology Center. MAScIR (Moroccan Foundation for Advanced Science, Innovation & Research)- Rabat Design Center, Rabat - Morocco. *Corresponding author E-mail: [email protected] Abstract Background: Ormenis eriolepis Coss (Asteraceae) is an endemic Moroccan subspecies, traditionally named “Hellala” or “Fergoga”. It’s usually used for its hypoglycemic effect as well as for the treatment of stomacal pain. As far as we know, there is no scientific exploration of anti tumoral activity of Ormenis eriolepis extracts. Materials and Methods: In this regard, we performed a screening of organic extracts and fractions in a panel of both hematological and solid cancer cell lines, to evaluate the potential in vitro anti tumoral activity and to elucidate the respective mechanisms that may be responsible for growth arrest and cell death induction. The plant was extracted using organic solvents, and four different extracts were screened on Jurkat, Jeko-1, TK-6, LN229, SW620, U2OS, PC-3 and NIH3T3 cells. Results: Cell viability assays revealed that, the IC50 values were (11,63±5,37µg/ml) for Jurkat, (13,33±1,67µg/ml) for Jeko-1, (41,67±1,98µg/ml) for LN229 and (19,31±4,88µg/ml) for PC-3 cells upon treatment with Oe-DF and Oe-HE respectively. -

Designing and Evaluating a Health Belief Model Based Intervention to Increase Intent of HPV Vaccination Among College Men: Use of Qualitative and Quantitative Methodology
Designing and evaluating a health belief model based intervention to increase intent of HPV vaccination among college men: Use of qualitative and quantitative methodology A dissertation submitted to the Graduate School of the University of Cincinnati In partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY In the School of Human Services of the College of Education, Criminal Justice, and Human Services 2012 by Purvi Mehta MS, University of Cincinnati Committee Chair: Manoj Sharma, M.B.; B.S., MCHES, Ph.D Abstract Humanpapilloma virus (HPV) is a common sexually transmitted disease/infection (STD/STI), leading to cervical and anal cancers. Annually, 6.2 million people are newly diagnosed with HPV and 20 million currently are diagnosed. According to the Centers for Disease Control and Prevention, 51.1% of men carry multiple strains of HPV. Recently, HPV vaccine was approved for use in boys and young men to help reduce the number of HPV cases. Currently limited research is available on HPV and HPV vaccination in men. The purpose of the study was to determine predictors of HPV vaccine acceptability among college men through the qualitative approach of focus groups and to develop an intervention to increase intent to seek vaccination in the target population The study took place in two phases. During Phase I, six focus groups were conducted with 50 participants. In Phase II using a randomized controlled trial a HBM based intervention was compared with a traditional knowledge based intervention in 90 college men. In Phase I lack of perceived susceptibility, perceived severity of HPV and barriers towards taking the HPV vaccine were major themes identified from the focus groups. -

Breast Cancer Treatment with Imiquimod: Applying an Old Lotion to a New Disease
Author Manuscript Published OnlineFirst on November 21, 2012; DOI: 10.1158/1078-0432.CCR-12-3138 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Breast cancer treatment with imiquimod: Applying an old lotion to a new disease Holbrook Kohrt, MD PhD Stanford University Cancer Institute Department of Medicine, Division of Oncology Stanford, CA 94305 Title: 79 characters Abstract: 49 words Text: 1200 words References: 12 references The author has no conflicts of interest. Running Title: Applying an old lotion to a new disease Downloaded from clincancerres.aacrjournals.org on September 25, 2021. © 2012 American Association for Cancer Research. Author Manuscript Published OnlineFirst on November 21, 2012; DOI: 10.1158/1078-0432.CCR-12-3138 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract Over the prior two decades, imiquimod, a toll-like receptor 7 agonist, has been applied to nearly fifty clinical settings. Due to its immunomodulatory role, the topical cream today for the first time, is being applied to cutaneous breast cancer in pre-clinical models and in a Phase 2 clinical trial. Manuscript In this issue of Clinical Cancer Research, two sets of authors from Demaria’s group, Dewan et al. (1) and Adams et al. (2) detail in companion papers the anti-tumor efficacy of imiquimod in first, a preclinical breast cancer model in combination with radiation (1), and second, a Phase 2, breast cancer clinical trial assessing safety and immunologic activity (2). Fifteen years after first approval by the Food and Drug Administration (FDA), imiquimod remains the only approved, active toll-like receptor (TLR) agonist (3).