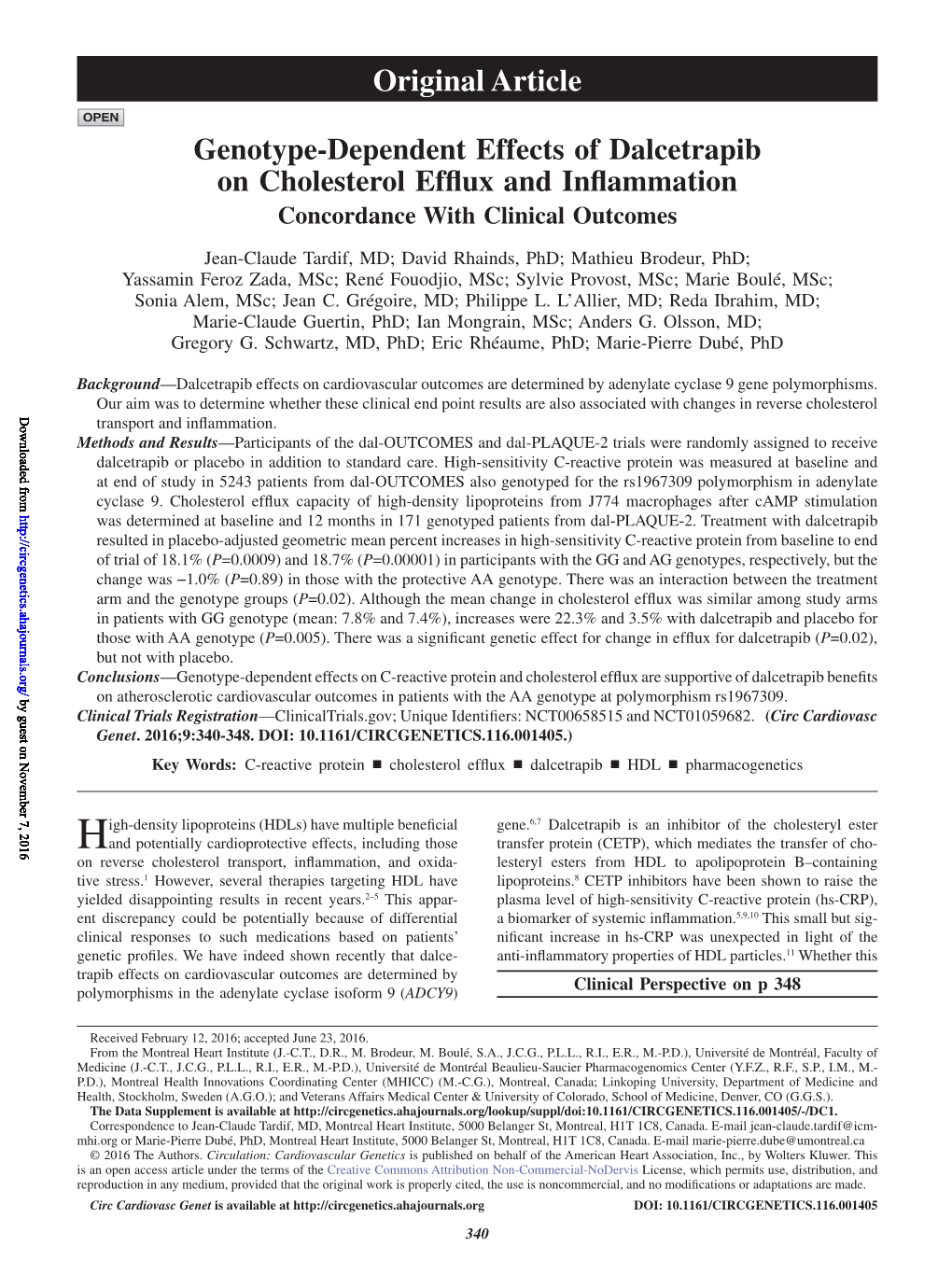
Genotype-Dependent Effects of Dalcetrapib on Cholesterol Efflux and Inflammation Concordance with Clinical Outcomes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cholesteryl Ester-Transfer Protein Inhibitors Stimulate Aldosterone Biosynthesis in Adipocytes Through Nox-Dependent Processes S
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2015/01/23/jpet.114.221002.DC1 1521-0103/353/1/27–34$25.00 http://dx.doi.org/10.1124/jpet.114.221002 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 353:27–34, April 2015 Copyright ª 2015 by The American Society for Pharmacology and Experimental Therapeutics Cholesteryl Ester-Transfer Protein Inhibitors Stimulate Aldosterone Biosynthesis in Adipocytes through Nox-Dependent Processes s Francisco J. Rios, Karla B. Neves, Aurelie Nguyen Dinh Cat, Sarah Even, Roberto Palacios, Augusto C. Montezano, and Rhian M. Touyz Institute of Cardiovascular and Medical Sciences, British Heart Foundation Glasgow Cardiovascular Research Centre, University of Glasgow, Glasgow, Scotland, United Kingdom (F.J.R., A.N.D.C., S.E., A.C.M., R.M.T.); Faculty of Pharmaceutical Sciences of Ribeirao Preto, University of Sao Paulo, Ribeirao Preto, Brazil (K.B.N.); and Departamento de Bioquímica, Fisiología y Genética Molecular Facultad de CC. de la Salud, Universidad Rey Juan Carlos, Madrid, Spain (R.P.) Downloaded from Received October 29, 2014; accepted January 22, 2015 ABSTRACT Hyperaldosteronism and hypertension were unexpected side whereby CETP inhibitors mediate effects, cells were pretreated effects observed in trials of torcetrapib, a cholesteryl ester-transfer with inhibitors of Nox1/Nox4 [GKT137831; 2-(2-chlorophenyl)-4-[3- jpet.aspetjournals.org protein (CETP) inhibitor that increases high-density lipoprotein. (dimethylamino)phenyl]-5-methyl-1H-pyrazolo[4,3-c]pyridine- Given that CETP inhibitors are lipid soluble, accumulate in adipose 3,6(2H,5H)-dione], Nox1 (ML171 [2-acetylphenothiazine]), mitochondria tissue, and have binding sites for proteins involved in adipogenesis, (rotenone), and STAT3 (S3I-201 [2-hydroxy-4-(((4-methylphenyl) and that adipocytes are a source of aldosterone, we questioned sulfonyloxy)acetyl)amino)-benzoic acid]). -
Next-Generation Sequencing Transforms Today's Biology
Evolving new therapies for the prevention of atherosclerosis: a glimpse of the near future G.K. Hovingh MD PhD ([email protected]) Department of Vascular Medicine AMC Amsterdam The Netherlands Today BMJ 2013;347:f544 www.chinadaily.com.cn/life/2009- 04/21/content_7698500.htm What we know - CVD major burden - LDL-C causally related with CVD - LDL-C goals: the lower the better - Statins : corner stone in therapy How well do we do? Reduction in MACE statin vs placebo (%) 0 -30 Potential for further risk reduction -100 Where do we go? Reduction in MACE statin vs placebo (%) 0 Potential for further -30 risk reduction -50 = further LDL-C lowering? and or Additional Rx? -100 A glance at the future… Atherosclerosis • LDL • HDL • TG • Lp(a) • Inflammation Lipid Modifying Drugs • Cholesterol absorption inhibitors • Squalene synthase inhibitors (SSI) • Microsomal triglyceride transfer protein (MTP) inhibitors • Acyl coenzyme A acyltransferase (ACAT) inhibitors • Diacylglycerol acyltransferase (DGAT) inhibitors • Thyroxin receptor agonists • ApoB mRNA antisense drugs • PCSK9 antibodies • ApoA1-based strategies (iv) • Cholesterol ester transfer protein (CETP) inhibitors ApoA-1 based therapy ApoA1 Mimetics, such as APL-180 Novartis Full-length ApoA1, such as ApoA1 Cerenis Therapeutics Pre-Beta HDL, as generated by delipidation, HDL Therapeutics Inc. Reconstituted HDL, CSL Ltd. ApoA1 Milano MDCO216, The Medicines Company Trimeric ApoA1, Borean Pharma and now Roche RVX-208, as developed by Resverlogix Fx-5A, as developed by Kinemed Inc. HDL -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

Clinical Pharmacokinetics and Pharmacodynamics of Dalcetrapib
Clin Pharmacokinet https://doi.org/10.1007/s40262-018-0656-3 REVIEW ARTICLE Clinical Pharmacokinetics and Pharmacodynamics of Dalcetrapib 1 2 3 3 3 Donald M. Black • Darren Bentley • Sunny Chapel • Jongtae Lee • Emily Briggs • Therese Heinonen1 Ó The Author(s) 2018 Abstract The cholesterol ester transfer protein (CETP) inhibitor dalcetrapib has been under evaluation for its Key Points potential to prevent cardiovascular (CV) events for almost two decades. The current clinical development program, Dalcetrapib is a selective cholesterol ester transfer representing new advances in precision medicine and protein (CETP) inhibitor that modulates reverse focused on a genetically defined population with acute cholesterol transport. An analysis of a large coronary syndrome (ACS), is supported by a large body of cardiovascular (CV) endpoint study has indicated pharmacokinetic and pharmacodynamic data as well as that dalcetrapib reduces CV events in patients with substantial clinical experience in over 13,000 patients and the AA genotype at rs7309 of the adenylate cyclase volunteers. Dalcetrapib treatment of 600 mg/day produces type 9 (ADCY9) gene. significant inhibition of CETP activity, and has been uti- lized in phase II and III studies, including CV endpoint The oral bioavailability of dalcetrapib is low and trials. Numerous studies have investigated the interactions limited by extensive first-pass metabolism. The between dalcetrapib and most drugs commonly prescribed timing and size of a meal also influences the to CV patients and have not demonstrated -

Study Design of Dal-Gene, a Pharmacogenetic Trial Targeting
Trial Design Study design of Dal-GenE, a pharmacogenetic trial targeting reduction of cardiovascular events with dalcetrapib Jean-Claude Tardif, MD, a Marie-Pierre Dubé, PhD, a,b Marc A. Pfeffer, MD, PhD, c David D. Waters, MD, d Wolfgang Koenig, MD, PhD, e Aldo P. Maggioni, MD, f John J. V. McMurray, MB, ChB, g Vincent Mooser, MD, h Harvey D. White, DsC, i Therese Heinonen, DVM, j Donald M. Black, MD, j and Marie-Claude Guertin, PhD k, for the dal-GenE Investigators 1 The objectives of precision medicine are to better match patient characteristics with the therapeutic intervention to optimize the chances of beneficial actions while reducing the exposure to unneeded adverse drug experiences. In a retrospective genome- wide association study of the overall neutral placebo-controlled dal-Outcomes trial, the effect of the cholesteryl ester transfer protein (CETP) modulator dalcetrapib on the composite of cardiovascular death, myocardial infarction or stroke was found to be influenced by a polymorphism in the adenylate cyclase type 9 (ADCY9) gene. Whereas patients with the AA genotype at position rs1967309 experienced fewer cardiovascular events with dalcetrapib, those with the GG genotype had an increased rate and the heterozygous AG genotype exhibited no difference from placebo. Measurements of cholesterol efflux and C- reactive protein (CRP) offered directionally supportive genotype-specific findings. In a separate, smaller, placebo-controlled trial, regression of ultrasonography-determined carotid intimal-medial thickness was only observed in dalcetrapib-treated patients with the AA genotype. Collectively, these observations led to the hypothesis that the cardiovascular effects of dalcetrapib may be pharmacogenetically determined, with a favorable benefit-risk ratio only for patients with this specific genotype. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -
Pharmacological Targeting of the Atherogenic Dyslipidemia Complex: the Next Frontier in CVD Prevention Beyond Lowering LDL Cholesterol
Diabetes Volume 65, July 2016 1767 Changting Xiao,1 Satya Dash,1 Cecilia Morgantini,1 Robert A. Hegele,2 and Gary F. Lewis1 Pharmacological Targeting of the Atherogenic Dyslipidemia Complex: The Next Frontier in CVD Prevention Beyond Lowering LDL Cholesterol Diabetes 2016;65:1767–1778 | DOI: 10.2337/db16-0046 Notwithstanding the effectiveness of lowering LDL cho- has been the primary goal of dyslipidemia management, lesterol, residual CVD risk remains in high-risk popula- with statins as the treatment of choice for CVD prevention. tions, including patients with diabetes, likely contributed Large-scale, randomized, clinical trials of LDL-lowering PERSPECTIVES IN DIABETES to by non-LDL lipid abnormalities. In this Perspectives therapies have demonstrated significant reduction in CVD in Diabetes article, we emphasize that changing demo- events over a wide range of baseline LDL-C levels (2,3). graphics and lifestyles over the past few decades have However, even with LDL-C levels lowered substantially or “ resulted in an epidemic of the atherogenic dyslipidemia at treatment goals with statin therapy, CVD risks are not ” complex, the main features of which include hypertrigly- eliminated and there remains significant “residual risk.” In- ceridemia, low HDL cholesterol levels, qualitative changes tensifying statin therapy may provide additional benefits in LDL particles, accumulation of remnant lipoproteins, (4,5); this approach, however, has limited potential, owing and postprandial hyperlipidemia. We brieflyreviewthe to tolerability, side effects, and finite efficacy. Further LDL-C underlying pathophysiology of this form of dyslipidemia, lowering may also be achieved with the use of nonstatin in particular its association with insulin resistance, obe- sity, and type 2 diabetes, and the marked atherogenicity agents, such as cholesterol absorption inhibitors and PCSK9 of this condition. -

Articles Article: Non-Statin Treatments for Managing LDL Cholesterol and Their Outcomes Download
Clinical Therapeutics/Volume 37, Number 12, 2015 Review Article Non-statin Treatments for Managing LDL Cholesterol and Their Outcomes Traci Turner, MD; and Evan A. Stein, MD, PhD Metabolic & Atherosclerosis Research Center, Cincinnati, Ohio ABSTRACT agents are being developed as orphan indications ex- Purpose: Over the past 3 decades reducing LDL-C pressly for patients with homozygous familial hyper- has proven to be the most reliable and easily achiev- cholesterolemia, including peroxisome proliferator able modifiable risk factor to decrease the rate of activated receptor-δ agonists, angiopoietin-like protein 3 cardiovascular morbidity and mortality. Statins are inhibitors, and gene therapy. effective, but problems with their side effects, adher- Implications: Monoclonal antibodies that inhibit ence, or LDL-C efficacy in some patient groups PCSK9 were shown to be very effective reducers of remain. Most currently available alternative lipid- LDL-C and well tolerated despite subcutaneous ad- modifying therapies have limited efficacy or tolerabil- ministration, and no significant safety issues have yet ity, and additional effective pharmacologic modalities emerged during large Phase II and III trials. They have to reduce LDL-C are needed. the potential to substantially impact further the risk of Methods: Recent literature on new and evolving cardiovascular disease. A number of additional new, LDL-C–lowering modalities in preclinical and clinical but less effective, oral LDL-C–lowering agents are development was reviewed. also in various stages of development, including Findings: Several new therapies targeting LDL-C are some which are targeted only to patients with homo- in development. Inhibition of proprotein convertase sub- zygous familial hypercholesterolemia. (Clin Ther. -

Effects of the Cholesteryl Ester Transfer Protein Inhibitor Dalcetrapib in Patients with Recent Acute Coronary Syndrome
Effects of the Cholesteryl Ester Transfer Protein Inhibitor Dalcetrapib in Patients with Recent Acute Coronary Syndrome Gregory G. Schwartz, MD PhD VA Medical Center and University of Colorado School of Medicine, Denver, Colorado On behalf of the dal-OUTCOMES* investigators * Funded by F. Hoffmann-La Roche, Ltd. Background • In observational analyses, higher levels of HDL-C are associated with lower cardiovascular risk • However, it is uncertain whether raising HDL-C therapeutically reduces cardiovascular risk • Inhibition of cholesteryl ester transfer protein (CETP) raises HDL-C and therefore might reduce cardiovascular risk • Dalcetrapib is a CETP inhibitor that raised HDL-C by approximately 30% in Phase 2 trials, without effect on blood pressure or neurohormones. Objective of the dal-OUTCOMES trial • To compare the effects of dalcetrapib with placebo, added to evidence-based background therapy, on cardiovascular risk in patients with recent acute coronary syndrome Entry criteria • Age ≥45 years • Acute coronary syndrome • Evidence-based management of LDL-C • No restriction on entry level of HDL-C • Key exclusions: Triglycerides >400 mg/dl; treatment with niacin, fibrates, or bile acid sequestrants. Study design Double-blind Until 1600 primary Single-blind Dalcetrapib 600 mg endpoint placebo run-in events. 4-12 weeks Placebo Two pre- specified interim analyses Identify Randomization patient 1 : 1 with ACS 935 sites in 27 countries Outcome measures • Primary outcome composite (time to first occurrence): – Coronary heart disease death -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Old and New in Lipid Lowering Therapy: Focus on The
FARMACIA, 2014, Vol. 62, 5 811 OLD AND NEW IN LIPID LOWERING THERAPY: FOCUS ON THE EMERGING DRUGS DANIELA BARTOȘ, CAMELIA DIACONU, ELISABETA BĂDILĂ*, ANA MARIA DARABAN University of Medicine and Pharmacy Carol Davila, Internal Medicine Clinic, Clinical Emergency Hospital of Bucharest, România * corresponding author: [email protected] Abstract The link between cholesterol and atherosclerosis has been long known. Studies on HDL (high density lipoprotein) cholesterol showed that it has two important roles: one in the transport of cholesterol and another directly on vascular endothelium, with a protective action and potential anti-atherogenic effects. Statins are the most common lipid- lowering drugs. Other drugs used in the treatment dyslipidemia are bile acid sequestrants, nicotinic acid, ezetimibe, probucol, neomycin, and fibrates. Because the response to treatment is not always satisfactory, new classes of drugs with different mechanisms of action have been developed in the latest years. Rezumat Legătura dintre colesterol şi ateroscleroză este de mult timp cunoscută. Studiile efectuate asupra HDL-colesterolului (high density lipoprotein) au arătat două roluri importante: unul asupra transportului de colesterol şi altul direct asupra endoteliului vascular, având o acţiune protectoare şi cu efecte potenţial anti-aterogene. Statinele sunt cele mai cunoscute medicamente hipolipemiante. Alte categorii de medicamente folosite în tratamentul dislipidemiilor sunt: sechestranţii de acizi biliari, acidul nicotinic, ezetimib, probucol, neomicina, fibraţii. Deoarece răspunsul la tratament nu este totdeauna satisfăcător, în ultimii ani au fost introduse în terapie noi clase de medicamente hipolipemiante, cu mecanisme de acţiune diferite faţă de cele cunoscute până acum. Keywords: dislipidemia, new lipid lowering drugs. Introduction In 1910, the German researchers have drawn attention to the link between cholesterol and atherosclerosis. -

Vascular Effects and Safety of Dalcetrapib in Patients with Or at Risk of Coronary Heart Disease: the Dal-VESSEL Randomized Clinical Trial
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library European Heart Journal (2012) 33, 857–865 CLINICAL doi:10.1093/eurheartj/ehs019 Vascular effects and safety of dalcetrapib in patients with or at risk of coronary heart disease: the dal-VESSEL randomized clinical trial Thomas F. Lu¨scher1*, Stefano Taddei2, Juan-Carlos Kaski3, J. Wouter Jukema4, David Kallend5, Thomas Mu¨nzel6, John J.P. Kastelein7, and John E. Deanfield8, on behalf of the dal-VESSEL Investigators 1Department of Cardiology, Cardiovascular Centre, University of Zurich, 8091 Zurich, Switzerland; 2Department of Internal Medicine, University of Pisa, Pisa, Italy; 3Cardiovascular Sciences Research Centre, St George’s, University of London, London, UK; 4Department of Cardiology, Leiden University Medical Center, Leiden, The Netherlands; 5Department of Medicine II, Johannes Gutenberg-University Mainz, Mainz, Germany; 6Department of Vascular Medicine, Academic Medical Center, Amsterdam, The Netherlands; 7F. Hoffmann-La Roche Ltd, Basle, Switzerland; and 8University College, London, UK Received 7 December 2011; revised 13 January 2012; accepted 20 January 2012; online publish-ahead-of-print 16 February 2012 This paper was guest edited by Prof. Bernard Gersh, Mayo Clinic, Division of Cardiovascular Diseases, Rochester, MN, USA See page 819 for the editorial comment on this article (doi:10.1093/eurheartj/ehs040) Aims High-density lipoprotein cholesterol (HDL-C) is inversely associated with cardiovascular (CV) events and thus an attractive therapeutic target. However, in spite of marked elevations in HDL-C, the first cholesterol transport protein (CETP) inhibitor torcetrapib raised blood pressure (BP), impaired endothelial function, and increased CV mortality and morbidity.