(1940-1960) : Vancomycin As an Example of The
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Antibiotic Assay Medium No. 3 (Assay Broth) Is Used for Microbiological Assay of Antibiotics. M042
HiMedia Laboratories Technical Data Antibiotic Assay Medium No. 3 (Assay Broth) is used for M042 microbiological assay of antibiotics. Antibiotic Assay Medium No. 3 (Assay Broth) is used for microbiological assay of antibiotics. Composition** Ingredients Gms / Litre Peptic digest of animal tissue (Peptone) 5.000 Beef extract 1.500 Yeast extract 1.500 Dextrose 1.000 Sodium chloride 3.500 Dipotassium phosphate 3.680 Potassium dihydrogen phosphate 1.320 Final pH ( at 25°C) 7.0±0.2 **Formula adjusted, standardized to suit performance parameters Directions Suspend 17.5 grams in 1000 ml distilled water. Heat if necessary to dissolve the medium completely. Sterilize by autoclaving at 15 lbs pressure (121°C) for 15 minutes. Advice:Recommended for the Microbiological assay of Amikacin, Bacitracin, Capreomycin, Chlortetracycline,Chloramphenicol,Cycloserine,Demeclocycline,Dihydrostreptomycin, Doxycycline, Gentamicin, Gramicidin, Kanamycin, Methacycline, Neomycin, Novobiocin, Oxytetracycline, Rolitetracycline, Streptomycin, Tetracycline, Tobramycin, Trolendomycin and Tylosin according to official methods . Principle And Interpretation Antibiotic Assay Medium is used in the performance of antibiotic assays. Grove and Randall have elucidated those antibiotic assays and media in their comprehensive treatise on antibiotic assays (1). Antibiotic Assay Medium No. 3 (Assay Broth) is used in the microbiological assay of different antibiotics in pharmaceutical and food products by the turbidimetric method. Ripperre et al reported that turbidimetric methods for determining the potency of antibiotics are inherently more accurate and more precise than agar diffusion procedures (2). Turbidimetric antibiotic assay is based on the change or inhibition of growth of a test microorganims in a liquid medium containing a uniform concentration of an antibiotic. After incubation of the test organism in the working dilutions of the antibiotics, the amount of growth is determined by measuring the light transmittance using spectrophotometer. -

Neomycin and Polymyxin B Sulfates and Gramicidin
NEOMYCIN AND POLYMYXIN B SULFATES AND GRAMICIDIN- neomycin sulfate, polymyxin b sulfate and gramicidin solution/ drops A-S Medication Solutions ---------- Neomycin and Polymyxin B Sulfates and Gramicidin Ophthalmic Solution, USP (Sterile) Rx only DESCRIPTION: Neomycin and Polymyxin B Sulfates and Gramicidin Ophthalmic Solution, USP is a sterile antimicrobial solution for ophthalmic use. Each mL contains: ACTIVES: Neomycin Sulfate, (equivalent to 1.75 mg neomycin base), Polymyxin B Sulfate equal to 10,000 Polymyxin B units, Gramicidin, 0.025 mg; INACTIVES: Sodium Chloride, Alcohol (0.5%), Poloxamer 188, Propylene Glycol, Purified Water. Hydrochloric Acid and/ or Ammonium Hydroxide may be added to adjust pH (4.7-6.0). PRESERVATIVE ADDED: Thimerosal 0.001%. Neomycin Sulfate is the sulfate salt of neomycin B and C, which are produced by the growth of Streptomyces fradiae Waksman (Fam. Streptomycetaceae). It has a potency equivalent of not less than 600 micrograms of neomycin base per milligram, calculated on an anhydrous basis. The structural formulae are: Polymyxin B Sulfate is the sulfate salt of polymyxin B1 and B2 which are produced by the growth of Bacillus polymyxa (Prazmowski) Migula (Fam. Bacillaceae). It has a potency of not less than 6,000 polymyxin B units per milligram, calculated on an anhydrous basis. The structural formulae are: Gramicidin (also called gramicidin D) is a mixture of three pairs of antibacterial substances (Gramicidin A, B and C) produced by the growth of Bacillus brevis Dubos (Fam. Bacillaceae). It has a potency of not less than 900 mcg of standard gramicidin per mg. The structural formulae are: CLINICAL PHARMACOLOGY: A wide range of antibacterial action is provided by the overlapping spectra of neomycin, polymyxin B sulfate, and gramicidin. -

Penicillin Allergy Guidance Document
Penicillin Allergy Guidance Document Key Points Background Careful evaluation of antibiotic allergy and prior tolerance history is essential to providing optimal treatment The true incidence of penicillin hypersensitivity amongst patients in the United States is less than 1% Alterations in antibiotic prescribing due to reported penicillin allergy has been shown to result in higher costs, increased risk of antibiotic resistance, and worse patient outcomes Cross-reactivity between truly penicillin allergic patients and later generation cephalosporins and/or carbapenems is rare Evaluation of Penicillin Allergy Obtain a detailed history of allergic reaction Classify the type and severity of the reaction paying particular attention to any IgE-mediated reactions (e.g., anaphylaxis, hives, angioedema, etc.) (Table 1) Evaluate prior tolerance of beta-lactam antibiotics utilizing patient interview or the electronic medical record Recommendations for Challenging Penicillin Allergic Patients See Figure 1 Follow-Up Document tolerance or intolerance in the patient’s allergy history Consider referring to allergy clinic for skin testing Created July 2017 by Macey Wolfe, PharmD; John Schoen, PharmD, BCPS; Scott Bergman, PharmD, BCPS; Sara May, MD; and Trevor Van Schooneveld, MD, FACP Disclaimer: This resource is intended for non-commercial educational and quality improvement purposes. Outside entities may utilize for these purposes, but must acknowledge the source. The guidance is intended to assist practitioners in managing a clinical situation but is not mandatory. The interprofessional group of authors have made considerable efforts to ensure the information upon which they are based is accurate and up to date. Any treatments have some inherent risk. Recommendations are meant to improve quality of patient care yet should not replace clinical judgment. -

Biological Function of Gramicidin: Studies on Gramicidin-Negative Mutants (Peptide Antibiotics/Sporulation/Dipicolinic Acid/Bacillus Brevis) PRANAB K
Proc. NatS. Acad. Sci. USA Vol. 74, No. 2, pp. 780-784, February 1977 Microbiology Biological function of gramicidin: Studies on gramicidin-negative mutants (peptide antibiotics/sporulation/dipicolinic acid/Bacillus brevis) PRANAB K. MUKHERJEE AND HENRY PAULUS Department of Metabolic Regulation, Boston Biomedical Research Institute, Boston, Massachusetts 02114; and Department of Biological Chemistry, Harvard Medical School, Boston, Massachusetts 02115 Communicated by Bernard D. Davis, October 28,1976 ABSTRACT By the use of a rapid radioautographic EXPERIMENTAL PROCEDURE screening rocedure, two mutants of Bacillus brevis ATCC 8185 that have lost the ability to produce gramicidin have been iso- lated. These mutants produced normal levels of tyrocidine and Bacterial Strains. Bacillus brevis ATCC 8185, the Dubos sporulated at the same frequency as the parent strain. Their strain, was obtained from the American Type Culture Collec- spores, however, were more heat-sensitive and had a reduced tion. Strain S14 is a streptomycin-resistant derivative of B. brevis 4ipicolinic acid content. Gramicidin-producing revertants oc- ATCC 8185, isolated on a streptomycin-gradient plate without curred at a relatively high frequency among tie survivors of mutagenesis. It grows well at 0.5 mg/ml of streptomycin, but prolonged heat treatment and had also regained the ability to produce heat-resistant spores. A normal spore phenotype could growth is retarded by streptomycin at 1.0 mg/ml. Strain B81 also be restored by the addition of gramicidin to cultures of the is a rifampicin-resistant derivative of strain S14, isolated on mutant strain at the end of exponential growth. On the other rifampicin-gradient plates after mutagenesis of spores with hand, the addition of dipicolinic acid could not cure the spore ethyl methanesulfonate (11). -

Topical Antibiotics for Impetigo: a Review of the Clinical Effectiveness and Guidelines
CADTH RAPID RESPONSE REPORT: SUMMARY WITH CRITICAL APPRAISAL Topical Antibiotics for Impetigo: A Review of the Clinical Effectiveness and Guidelines Service Line: Rapid Response Service Version: 1.0 Publication Date: February 21, 2017 Report Length: 23 Pages Authors: Rob Edge, Charlene Argáez Cite As: Topical antibiotics for impetigo: a review of the clinical effectiveness and guidelines. Ottawa: CADTH; 2017 Feb. (CADTH rapid response report: summary with critical appraisal). ISSN: 1922-8147 (online) Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

UNASYN® (Ampicillin Sodium/Sulbactam Sodium)
NDA 50-608/S-029 Page 3 UNASYN® (ampicillin sodium/sulbactam sodium) PHARMACY BULK PACKAGE NOT FOR DIRECT INFUSION To reduce the development of drug-resistant bacteria and maintain the effectiveness of UNASYN® and other antibacterial drugs, UNASYN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION UNASYN is an injectable antibacterial combination consisting of the semisynthetic antibiotic ampicillin sodium and the beta-lactamase inhibitor sulbactam sodium for intravenous and intramuscular administration. Ampicillin sodium is derived from the penicillin nucleus, 6-aminopenicillanic acid. Chemically, it is monosodium (2S, 5R, 6R)-6-[(R)-2-amino-2-phenylacetamido]- 3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylate and has a molecular weight of 371.39. Its chemical formula is C16H18N3NaO4S. The structural formula is: COONa O CH3 N CH O 3 NH S NH2 Sulbactam sodium is a derivative of the basic penicillin nucleus. Chemically, sulbactam sodium is sodium penicillinate sulfone; sodium (2S, 5R)-3,3-dimethyl-7-oxo-4-thia 1-azabicyclo [3.2.0] heptane-2-carboxylate 4,4-dioxide. Its chemical formula is C8H10NNaO5S with a molecular weight of 255.22. The structural formula is: NDA 50-608/S-029 Page 4 COONa CH3 O N CH3 S O O UNASYN, ampicillin sodium/sulbactam sodium parenteral combination, is available as a white to off-white dry powder for reconstitution. UNASYN dry powder is freely soluble in aqueous diluents to yield pale yellow to yellow solutions containing ampicillin sodium and sulbactam sodium equivalent to 250 mg ampicillin per mL and 125 mg sulbactam per mL. -
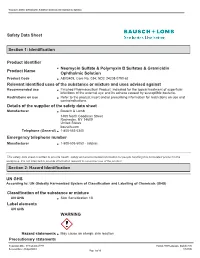
Identification Product Identifier Product Name Neomycin Sulfate
Neomycin Sulfate & Polymyxin B Sulfates & Gramicidin Ophthalmic Solution Safety Data Sheet Section 1: Identification Product identifier Neomycin Sulfate & Polymyxin B Sulfates & Gramicidin Product Name Ophthalmic Solution Product Code AB03409; Core No. 034; NDC 24208-0790-62 Relevant identified uses of the substance or mixture and uses advised against Recommended use Finished Pharmaceutical Product; Indicated for the topical treatment of superficial infections of the external eye and its adnexa caused by susceptible bacteria. Restrictions on use Refer to the product insert and/or prescribing information for restrictions on use and contraindications. Details of the supplier of the safety data sheet Manufacturer Bausch & Lomb 1400 North Goodman Street Rochester, NY 14609 United States bausch.com Telephone (General) 1-800-553-5340 Emergency telephone number Manufacturer 1-800-535-5053 - Infotrac This safety data sheet is written to provide health, safety and environmental information for people handling this formulated product in the workplace. It is not intended to provide information relevant to consumer use of the product. Section 2: Hazard Identification UN GHS According to: UN Globally Harmonized System of Classification and Labelling of Chemicals (GHS) Classification of the substance or mixture UN GHS Skin Sensitization 1B Label elements UN GHS WARNING Hazard statements May cause an allergic skin reaction Precautionary statements Preparation Date: 07/September/1994 Format: GHS Language: English (US) Revision Date: 24/April/2015 UN GHS Page 1 of 10 Neomycin Sulfate & Polymyxin B Sulfates & Gramicidin Ophthalmic Solution Prevention Wash thoroughly after handling. Response IF ON SKIN: Wash with plenty of soap and water. If skin irritation or rash occurs: Get medical advice/attention. -

I BOOK REVIEWS
Indian Inst. Sci. 63 (d), Mar. I983„ Pp. 4-.31 ic Indian Institute of science, Printed in India. BOOK REVIEWS The enchanted ring : The untold story of penicillin by John C. Sheehan. The Mb' press, Cambridge, Massachusetts 02142, USA, 1982, pp. xvi + 224, $ 15 (Asia $ 17.25). Despite the large number of monographs, review articles and popular literature avail. , able on penicillins and 13-lactum antibiotics, many facets of the development of the wonder drug are not known to the lay scientists. The readers of literature on penicillin gene- rally consider penicillin as a triumph of British science as the great names associated with the isolation and structure elucidation of penicillin were British stalwarts such as Alexander Fleming, Florey, Chain, Abraham Heatley and even Sir Robert Robinson. It was English crystallographer Dorothy Hodgkin who elucidated the correct structure. It is also generally accepted that the superior microbial techniques, the dynamic and innovative methodology of the American fermentation industry which made the drug available to millions at the end of the Second World War. in 1957, when John Sheehan reported the first acceptable total synthesis of penicillin he created a great sensation. The Enchanted Ring tells the story of Sheehan's involvement in the process. It is a story of indomitable faith and courage as well as superhuman perseverence which finally led to the success. The most amazing event in the history of penicillin is the confusion regarding its exact composition and structure. No other compound of a molecular weight of about 300 has baffled so many brilliant chemists. Even after the structure of penicillin was una equivocally established, Sir Robert Robinson held on. -

Antibiotics & Common Infections ABX-2
- - Summaries: Trial SSTI Related toxicity rare - Evidence/Safety, Q&As/Extras: Nitrofurantion documents/GeriRxFiles-UTI.pdf http://www.rxfiles.ca/rxfiles/uploads/ Adults: UTIinOlder Geri-RxFiles RxFILES EXTRAS FROM lookup/59/2/e10 https://academic.oup.com/cid/article- Infections Tissue Skin &Soft IDSA2014: U.S. TISSUEINFECTIONS SKIN &SOFT assets/files/guidelines/en/1121.pdf https://www.cua.org/themes/web/ UTI Recurrent 2011: CUA 2163(16)34717-X/pdf http://www.jogc.com/article/S1701- UTI Recurrent SOGC 2010: 19April2013.pdf photos/custom/UTI%20Guidelines%20 https://saskpic.ipac-canada.org/ Settings Care UTI inContinuing 2013: SK MOH lookup/52/5/e103 https://academic.oup.com/cid/article- (UTI) Pylonephritis Cystitisand Acute Uncomplicated IDSA2010: U.S. CYSTITIS / UTI http://www.mumshealth.com MUMS Guidelines: http://www.bugsanddrugs.ca/ &Drugs: Bugs CANADIAN LINKS ABX-2 RELATED Skin Abscess: I&D +/- ABX I&D +/-ABX Skin Abscess: Clindamycin vs TMP/SMX vsTMP/SMX Clindamycin GUIDELINES/REFERENCES GUIDELINES/REFERENCES - Antibiotics & Common Infections &CommonInfections Antibiotics Stewardship, Effectiveness, Safety & Clinical Pearls-April2017 & Stewardship, Effectiveness,Safety ( Susceptibility of of Susceptibility 1) CYSTISIS UNCOMPLICATED CAUGHTOUREYE... FROMINSIDE THAT ABX-2: AFEWPEARLS Pad”. “Viral Prescription at allavailable These are friendly postersandthepatient suchasthe“GoneViral?”office/clinic extra supporttools on discussions inSaskatchewan. withproviders discussions detailing our springacademic Our tissue(SSTI)infections. and skin&soft willsupport The newchartsinthisnewsletter cystitis uncomplicated of onthetreatment topic tobringouttheABX-2 excited are We ONABX RxFILES ACADEMIC DETAILING pg9) (see Know youroptions! anaphylaxis). (e.g. allergy mediated atrueIgE will have ___ only “allergy”, penicillin 7) ALLERGY LACTAM BETA cellulitis. of treatment successful inthe essential -often 5) verywell. -

Cephalosporin Administration to Patients with a History of Penicillin Allergy Adverse Reactions to Drugs, Biologicals and Latex Committee
Work group report May, 2009 Cephalosporin Administration to Patients with a History of Penicillin Allergy Adverse Reactions to Drugs, Biologicals and Latex Committee Work Group Members : Roland Solensky, MD FAAAAI, Chair Aleena Banerji, MD Gordon R. Bloomberg, MD FAAAAI Marianna C. Castells, MD PhD FAAAAI Paul J. Dowling, MD George R. Green, MD FAAAAI Eric M. Macy, MD FAAAAI Myngoc T. Nguyen, MD FAAAAI Antonino G. Romano, MD PhD Fanny Silviu-Dan, MD FAAAAI Clifford M. Tepper, MD FAAAAI INTRODUCTION Penicillins and cephalosporins share a common beta-lactam ring structure, and hence the potential for IgE-mediated allergic cross-reactivity. Allergic cross-reactivity between penicillins and cephalosporins potentially may also occur due to presence of identical or similar R-group side chains, in which case IgE is directed against the side chain, rather the core beta-lactam structure. This work group report will address the administration of cephalosporins in patients with a history of penicillin allergy. First, published data will be reviewed regarding 1) cephalosporin challenges of patients with a history of penicillin allergy (without preceding skin testing or in vitro testing), and 2) cephalosporin challenges of patients proven to have a type I allergy to penicillins (via positive penicillin skin test, in vitro test or challenge). Secondly, 1 2/9/2011 recommendations on cephalosporin administration to patients with a history of penicillin allergy will be presented. Unless specifically noted, the term ‘penicillin allergy’ will be used to indicate an allergy to one or more of the penicillin-class antibiotics, not just to penicillin itself. The following discussion includes references, in certain clinical situations, to performing cephalosporin graded challenges in patients with a history of penicillin allergy. -
![Subpart J—Certain Other Dosage Forms [Reserved] PART](https://docslib.b-cdn.net/cover/6583/subpart-j-certain-other-dosage-forms-reserved-part-1016583.webp)
Subpart J—Certain Other Dosage Forms [Reserved] PART
Pt. 448 21 CFR Ch. I (4±1±96 Edition) (ii) Samples required: Subpart HÐRectal Dosage Forms (a) The oxytetracycline hydro- [Reserved] chloride used in making the batch: 10 packages, each containing approxi- mately 300 milligrams. Subpart IÐ[Reserved] (b) The polymyxin B sulfate used in making the batch: 10 packages, each Subpart JÐCertain Other Dosage containing approximately 300 milli- Forms [Reserved] grams. (c) The batch: A minimum of 30 tab- PART 448ÐPEPTIDE ANTIBIOTIC lets. DRUGS (b) Tests and methods of assayÐ(1) Po- tencyÐ(i) Oxytetracycline content. Pro- Subpart AÐBulk Drugs ceed as directed in § 436.106 of this chap- ter, preparing the sample for assay as Sec. 448.10 Bacitracin. follows: Place a representative number 448.10a Sterile bacitracin. of tablets into a high-speed glass blend- 448.13 Bacitracin zinc. er jar containing sufficient 0.1N hydro- 448.13a Sterile bacitracin zinc. chloric acid to obtain a stock solution 448.15a Sterile capreomycin sulfate. of convenient concentration containing 448.20a Sterile colistimethate sodium. not less than 150 micrograms of oxytet- 448.21 Colistin sulfate. racycline per milliliter (estimated). 448.23 Cyclosporine. Blend for 3 to 5 minutes. Remove an al- 448.25 Gramicidin. iquot of the stock solution and further 448.30 Polymyxin B sulfate. dilute with sterile distilled water to 448.30a Sterile polymyxin B sulfate. the reference concentration of 0.24 448.75 Tyrothricin. microgram of oxytetracycline per mil- liliter (estimated). Subpart BÐOral Dosage Forms (ii) Polymyxin B content. Proceed as 448.121 Colistin sulfate for oral suspension. directed in § 436.105 of this chapter, pre- 448.123 Cyclosporine oral dosage forms. -

Design and Syntheses of Gramicidin S Analogs, Cyclo(-X-Leu-XD
The Journal of Antibiotics (2011) 64, 583–585 & 2011 Japan Antibiotics Research Association All rights reserved 0021-8820/11 $32.00 www.nature.com/ja NOTE Design and syntheses of gramicidin S analogs, cyclo(-X-Leu-X-D-Phe-Pro-)2 (X¼His, Lys, Orn, Dab and Dap) Makoto Tamaki1, Kenta Fujinuma1, Takuji Harada1, Kazumasa Takanashi1, Mitsuno Shindo2, Masahiro Kimura2 and Yoshiki Uchida2 The Journal of Antibiotics (2011) 64, 583–585; doi:10.1038/ja.2011.43; published online 25 May 2011 Keywords: gramicidin S; polycationic analog; structure-activity relationship; synthesis 1,1¢ 2,2¢ 3,3¢ 4,4¢ 5,5¢ 1–3 Gramicidin S (GS), cyclo(-Val -Orn -Leu -D-Phe -Pro -)2, solid phase peptide synthesis on oxime resin (loading of oxime group: is a potent cyclopeptide antibiotic isolated from Bacillus brevis.Its 0.35 mmol gÀ1 resins) (Scheme 1).8 Yresidue(Y¼His(3-Bom), Lys(Z), secondary structure has been established as an antiparallel b-sheet Orn(Z), Dab(Z) and Dap(Z)) as a C-terminal amino acid residue was conformation with amphiphilicity.4,5 The conformation is charac- used based on the propensity of the biosynthetic precursor of GS teristically featured with the orientation of side chains in such a way to form a conformation highly favorable for head–tail cyclization.2,3 that the charged Orn side chains are situated on one side of the The cyclization-cleavage of H-D-Phe-Pro-Y-Leu-Y-D-Phe-Pro-Y-Leu- molecule and the hydrophobic Val and Leu side chains are situated on Y-oxime from the resin was performed in 1,4-dioxane with 2 equiv the other side.