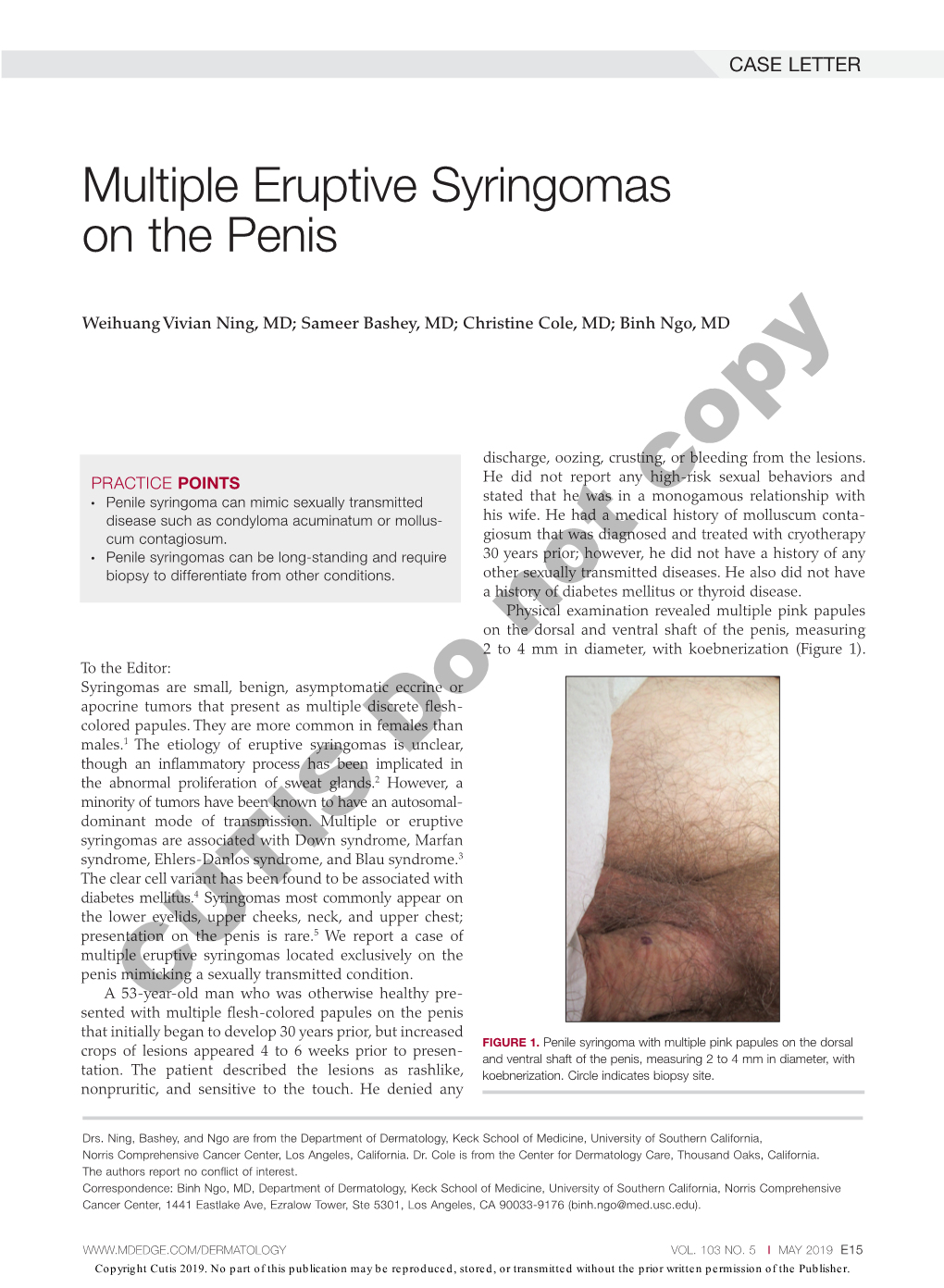
Multiple Eruptive Syringomas on the Penis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genital Dermatology
GENITAL DERMATOLOGY BARRY D. GOLDMAN, M.D. 150 Broadway, Suite 1110 NEW YORK, NY 10038 E-MAIL [email protected] INTRODUCTION Genital dermatology encompasses a wide variety of lesions and skin rashes that affect the genital area. Some are found only on the genitals while other usually occur elsewhere and may take on an atypical appearance on the genitals. The genitals are covered by thin skin that is usually moist, hence the dry scaliness associated with skin rashes on other parts of the body may not be present. In addition, genital skin may be more sensitive to cleansers and medications than elsewhere, emphasizing the necessity of taking a good history. The physical examination often requires a thorough skin evaluation to determine the presence or lack of similar lesions on the body which may aid diagnosis. Discussion of genital dermatology can be divided according to morphology or location. This article divides disease entities according to etiology. The clinician must determine whether a genital eruption is related to a sexually transmitted disease, a dermatoses limited to the genitals, or part of a widespread eruption. SEXUALLY TRANSMITTED INFECTIONS AFFECTING THE GENITAL SKIN Genital warts (condyloma) have become widespread. The human papillomavirus (HPV) which causes genital warts can be found on the genitals in at least 10-15% of the population. One study of college students found a prevalence of 44% using polymerase chain reactions on cervical lavages at some point during their enrollment. Most of these infection spontaneously resolved. Only a minority of patients with HPV develop genital warts. Most genital warts are associated with low risk HPV types 6 and 11 which rarely cause cervical cancer. -

Treatment of Warts with Topical Cidofovir in a Pediatric Patient
Volume 25 Number 5| May 2019| Dermatology Online Journal || Case Report 25(5):6 Treatment of warts with topical cidofovir in a pediatric patient Melissa A Nickles BA, Artem Sergeyenko MD, Michelle Bain MD Affiliations: Department of Dermatology, University of Illinois at Chicago College of Medicine, Chicago, llinois, USA Corresponding Author: Artem Sergeyenko MD, 808 South Wood Street Suite 380, Chicago, IL 60612, Tel: 847-338-0037, Email: a.serge04@gmail topical cidofovir is effective in treating HPV lesions Abstract and molluscum contagiosum in adult patients with Cidofovir is an antiviral nucleotide analogue with HIV/AIDS [2]. Case reports have also found topical relatively new treatment capacities for cidofovir to effectively treat anogenital squamous dermatological conditions, specifically verruca cell carcinoma (SCC), bowenoid papulosis, vulgaris caused by human papilloma virus infection. condyloma acuminatum, Kaposi sarcoma, and HSV-II In a 10-year old boy with severe verruca vulgaris in adult patients with HIV/AIDS [3]. Cidofovir has recalcitrant to multiple therapies, topical 1% experimentally been shown to be effective in cidofovir applied daily for eight weeks proved to be an effective treatment with no adverse side effects. treating genital condyloma acuminata in adult This case report, in conjunction with multiple immunocompetent patients [4] and in a pediatric published reports, suggests that topical 1% cidofovir case [5]. is a safe and effective treatment for viral warts in Cidofovir has also been used in pediatric patients to pediatric patients. cure verruca vulgaris recalcitrant to traditional treatment therapies. There have been several reports Keywords: cidofovir, verruca vulgaris, human papilloma that topical 1-3% cidofovir cream applied once or virus twice daily is effective in treating verruca vulgaris with no systemic side effects and low rates of recurrence in immunocompetent children [6-8], as Introduction well as in immunocompromised children [9, 10]. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Colposcopy of the Vulva, Perineum and Anal Canal
VESNA KESIC Colposcopy of the vulva, perineum and anal canal CHAPTER 14 Colposcopy of the vulva, perineum and anal canal VESNA KESIC INTRODUCTION of the female reproductive system. The vulva is responsive for Colposcopy of the vulva – vulvoscopy – is an important part the sex steroids. The alterations that are clinically recog- of gynaecological examination. However, it does not provide as nizable in the vulva throughout life and additional cyclic much information about the nature of vulvar lesions as col- changes, occurring during the reproductive period, are the poscopy of the cervix. This is due to the normal histology of this result of sequential variations of ovarian hormone secretion. area, which is covered by a keratinized, stratified squamous Significant changes happen during puberty, sexual inter- epithelium. The multifocal nature of vulvar intraepithelial dis- course, pregnancy, delivery, menopause and the postmeno- ease makes the examination more difficult. Nevertheless, col- pausal period, which alter the external appearance and func- poscopy should be performed in the examination of vulvar pa- tion of the vulva. Knowledge about this cyclical activity is im- thology because of its importance in identifying the individual portant in diagnosis and treatment of vulvar disorders. components of the lesions, both for biopsy and treatment pur- poses. Anatomically, the vulva, the term that designates exter- It should be remembered that the vestibule, as an endodermal nal female genital organs, consists of the mons pubis, the labia derivate, is less sensitive to sex hormones than adjacent struc- majora, the labia minora, the clitoris including frenulum and tures. This should be taken into consideration during the treat- prepuce, the vestibule (the vestibule, the introitus), glandular ment of certain vulvar conditions such as vestibulitis. -

Safety and Efficacy of Topical Cidofovir to Treat High-Grade Perianal And
Safety and efficacy of topical cidofovir to treat high-grade perianal and vulvar intraepithelial neoplasia in HIV-positive men and women Elizabeth A. Stiera, Stephen E. Goldstoneb, Mark H. Einsteinc, Naomi Jayd, John M. Berryd, Timothy Wilkine, Jeannette Y. Leef, Teresa M. Darraghg, Maria Da Costad, Lori Pantherh, David Aboulafiai and Joel M. Palefskyd 09/15/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD35y8U/jUqeEzZu3CM2R+euzaQ04PJ10v9LxBxxWvdNy4= by https://journals.lww.com/aidsonline from Downloaded Downloaded Objective: To evaluate the safety and efficacy of topical cidofovir for treatment of high- from grade squamous perianal intraepithelial neoplasia (PAIN) and vulvar intraepithelial https://journals.lww.com/aidsonline neoplasia (VIN) lesions in HIV-positive individuals. Design: Phase IIa prospective multicenter trial conducted at eight clinical sites through the AIDS Malignancy Consortium. Methods: HIV-positive patients with biopsy-proven high-grade PAIN that was at least 3cm2 were enrolled. PAIN biopsy specimens were assessed for human papillomavirus by (HPV) using PCR and type-specific HPV probing. Participants applied 1% topical BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD35y8U/jUqeEzZu3CM2R+euzaQ04PJ10v9LxBxxWvdNy4= cidofovir to PAIN and VIN (if present) for six 2-week cycles. Results were designated as complete response (CR), partial response (PR) (>50% reduction in size), stable disease, or progressive disease (PD). Results: Twenty-four men and nine women (eight with high-grade VIN as well) were enrolled. Mean age was 44 years and mean CD4þ cell count was 412 cells/ml. HPV DNA (most commonly HPV16) was detected in all pretreatment study specimens. Twenty six (79%) participants completed treatment per protocol: CR, five (15%); PR, 12 (36%), stable disease, seven (21%); PD, two (6%) (one with a superficially invasive cancer and one with new area of high-grade PAIN). -

Human Immunodeficiency Virus and Malignancy: Thoughts on Viral
SPECIAL ARTICLE Human Immunodeficiency Virus and Malignancy Thoughts on Viral Oncogenesis William P. Schecter, MD n the spring of 1981, as a newly minted assistant professor of surgery at the University of California–San Francisco, I was called to see a 33-year-old man with bilateral interstitial pulmonary infiltrates who was dying of acute respiratory failure at San Francisco General Hospital. My medical colleagues requested an open-lung biopsy. To our mutual amaze- Iment, this previously healthy gay man had Pneumocystis carinii pneumonia, despite the fact that there was no history of lymphoma or organ transplantation. The first cluster of cases of this pneu- monia was reported the same year.1 At approximately the same time, a previ- surgeons in San Francisco and elsewhere ously rare tumor, Kaposi sarcoma (KS), be- spent a lot of time performing biopsies on gan to appear in epidemic numbers, first HIV-infected gay men with generalized reported in Los Angeles, Calif, and New lymphadenopathy. It was not long before York, NY.2 By 1983, Luc Montagnier had B-cell lymphomas, located in the gut, brain, discovered an RNA retrovirus associated liver, and other relatively unusual sites, be- with the disease complex occurring pri- came common devastating problems.8 marily in gay men, which had been termed One of my early patients was a pre- the acquired immune deficiency syndrome viously healthy 29-year-old gay man with (AIDS).3 The viral etiology of AIDS was not no known history of HIV infection who generally accepted in the United States un- presented with a small-bowel obstruc- til 1984, when Gallo et al4 confirmed Mon- tion and computed tomographic evi- tagnier’s work with specimens obtained dence of a large soft tissue mass involv- from Montagnier. -
C O N F E R E N C E 11 5 December 2018
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2018-2019 C o n f e r e n c e 11 5 December 2018 Conference Moderator: Charles W. Bradley, VMD, DACVP Assistant Professor, Pathobiology University of Pennsylvania School of Veterinary Medicine 4005 MJR-VHUP 3900 Delancey Street Philadelphia, PA, 19104 CASE I: P15/141 JPC 4066260) macrophages, eosinophils and neutrophils (exocytosis), and rare, multifocal, discrete, Signalment: 2.5-year-old, Aubrac bull, Bos shrunken, hypereosinophilic keratinocytes taurus with pyknotic nuclei (apoptosis). The superficial dermis and a variable part of the History: The bull presented to Veterinary adjacent deep dermis are markedly and Teaching Hospital with history of chronic diffusely expanded by a moderate, skin lesions of unknown reason. coalescing, perivascular, and nodular to diffuse infiltration of macrophages, plasma Gross Pathology: Multifocal areas of cells, lymphocytes, eosinophilic alopecia granulocytes and to a locally variable extent also neutrophilic granulocytes, as well as a Laboratory results: PCR positive for B. low to moderate, coalescing amount of besnoiti, ELISA positive for B. besnoiti bundles of fibroblasts and fibrocytes within a collagenous stroma (fibrosis). There is a Microscopic Description: marked coalescing to diffuse loss of Haired skin. The epidermis displays low to moderate, diffuse, orthokeratotic hyperkeratosis, moderate, diffuse, epidermal hyperplasia characterized by acanthosis and irregular rete ridge formation, rare, multifocal, individual, -

Topical Imiquimod for Bowenoid Papulosis in an HIV-Positive Woman
212 Letters to the Editor Topical Imiquimod for Bowenoid Papulosis in an HIV-positive Woman Pedro Redondo and Pedro Lloret Department of Dermatology, University Clinic of Navarra, School of Medicine, P.O. Box 4209, ES-31080, Pamplona, Spain. E-mail: [email protected] Accepted February 18, 2002. Sir, CASE REPORT Bowenoid papulosis consists clinically of multiple verru- coid papules, usually situated in the anogenital region A 36-year-old woman presented with perianal and gen- of young men and women. Histologically, it is an in situ ital skin lesions of 6 years’ duration. The patient’s HIV-1 squamous cell carcinoma (1) and is most commonly infection had been diagnosed approximately 10 years associated with high-risk oncogenic genotypes of human earlier, and had been well controlled during most of papillomavirus (HPV ) types 16, 18, 33 and 39 (2, 3). that time with antiviral therapy. The patient’s viral load Bowenoid papulosis usually follows a benign course and and CD4 levels were 50 copies/ml and 750/mm3, respect- may spontaneously resolve in immunocompetent ively. She had received previous treatment with cryo- patients. In older women and immunocompromised therapy and local excision with electrocoagulation, with patients it generally persists and may progress to an relapses. Physical examination revealed perianal and invasive squamous cell carcinoma. Conventional treat- perivulvar red plaques covered with warty papules ments include local excision, electrocoagulation, elec- (Fig. 1A). Histological specimens con rmed the clinical trodessication, cryosurgery, laser removal and topical diagnosis of bowenoid papulosis. Topical treatment with 5- uorouracil. Imiquimod, an imidazoquinoline amine, imiquimod 5% cream was proposed. -

Download PDF Clinical, Histological and Therapeutic Features of Bowen S
Rom J Morphol Embryol 2017, 58(1):33–40 R J M E EVIEW Romanian Journal of R Morphology & Embryology http://www.rjme.ro/ Clinical, histological and therapeutic features of Bowen’s disease TIBERIU PAUL NEAGU1,2), MIRELA ŢIGLIŞ3), DELIA BOTEZATU4), VALENTIN ENACHE5), CLAUDIA OANA COBILINSCHI6,7), MUREŞ SEBASTIAN VÂLCEA-PRECUP8,9), IOANA MARINA GRINŢESCU3,10) 1)Department of Plastic Surgery and Reconstructive Microsurgery, Emergency Clinical Hospital of Bucharest, Romania 2)Clinical Department No. 11, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania 3)Department of Anesthesiology and Intensive Care, Emergency Clinical Hospital of Bucharest, Romania 4)Department of Dermato-Venereology, “Prof. Dr. Victor Babeş” Clinical Hospital of Infectious and Tropical Diseases, Bucharest, Romania 5)Department of Pathology, Emergency Clinical Hospital of Bucharest, Romania 6)Department of Rheumatology and Internal Medicine, “Sf. Maria” Clinical Hospital, Bucharest, Romania 7)Clinical Department No. 5, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania 8)Department of General Surgery, Emergency Clinical Hospital of Bucharest, Romania 9)Clinical Department No. 10, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania 10)Clinical Department No. 14, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania Abstract Squamous cell carcinoma (SCC) in situ or Bowen’s disease (BD) is a slowly progressive malignancy. However, cases of regression have been reported. Recent reviews cover only certain aspects of this disease; therefore, this paper’s aim is to cover all the relevant aspects for medical practice, such as clinical, histological and therapeutic details. BD may affect all regions of the skin and mucosa, but in accordance with the region and etiologic factor, it may embrace different clinical forms, some of them very similar with other skin lesions. -

Infectious Disease: Viral Infections
Chris Hixon DO, PGY4 Megan Joint DO, PGY 4 Lewis Gale Hospital Montgomery / VCOM Program Director: Daniel S. Hurd DO, FAOCD Human Herpes Virus 1-8 Parvo Virus Molluscum Contagiousum Milker’s Nodule Human Papilloma Virus Measles Rubella Hand-Foot-Mouth Disease Orf Vaccinia Cowpox Classification Lytic Infection Latent Infection Herpes Simplex Virus Alphaherpesvirinae Epithelial cells Neuron type 1 Herpes SimplexVirus Alphaherpesvirinae Epithelial cells Neuron type 2 HHV 3 – Varicella Alphaherpesvirinae Epithelial cells Neuron Zoster virus HHV 4 - EBV Gammaherpesvirinae Epithelial cells B Lymphocytes and B – cells HHV 5 - CMV Betaherpesvirinae Lymphocytes, Macrophages, Macrophages Lymphocytes and Endothelial cells HHV 6 Betaherpesvirinae CD4 T cells Lymphocytes HHV 7 Betaherpesvirinae T cells T Lymphocytes HHV8 Gammaherpesvirinae Lymphocytes Lymphocytes and Endothelial cells HSV - 1 HSV 2 Initial presentation: . Prodrome Initial presentation: . Gingivostomatitis . Frequently asymptomatic . Painful, erosive balanitis, vulvitis or vaginitis Recurrent lesions: . Herpetiform vesicles on the vermilion border of lip Usually mild recurrence with resolution within 1 week Herpetic whitlow Eczema herpeticum (Kaposi’s varicelliform eruption) Ocular infections . Infection in areas of . branching dendritic corneal lesions dermatitis/skin barrier disruption Herpes Folliculitis Herpes Gladiatorum Chronic enlarging ulcers Encephalitis Temporal lobe Neonatal HSV infection DIAGNOSIS TREATMENT Tzanck smear Oral Antiviral medications -

Male Genital Lesions
Male Genital Lesions Conrad L. Brimhall, MD, FAAD Kentucky Dermatology & Skin Cancer Clinic Lexinggyton & London, Kentucky Categories o f Les io ns Infectious Neoplastic Herpes Simplex BowenBowens’sDisease Disease Syphilis Squamous Cell Carcinoma Condyloma accuminata Verrucous Carcinoma Candida Extramammary Paget’s Pearly Penile Papules Other Other Inflammatory Traumatic Psoriasis Automobile Accidents Lichen Planus Crush Injuries Contact Dermatitis Suction/vacuum erection device FFedDugEuptoixed Drug Eruption PilTPenile Tourni quet tSd Syndrome Lichen Sclerosis et trophicus Zipper Entrapment Zoon’s Balanitis Sexually Induced Other Iatrogenic Differential Diagnosis Fixed drug eruption Allergic/irritant contact dermatitis IfInfecti on Neoplastic Trauma Psoriasiform/Papulosquamous Balanitides Mnemonic: F.A.I.N.T. with Psoriatic Balanitis Evaluation History Nature of complaints Circumcised or uncircumcised Recurrences and duration Sexual practices Coital partner complaints Prophylactic measures Dysuria Medications: oral and topical Allergies RiReview o f systems: S ystemi c comp lilaints Evaluation Physical Examination Inflammation Edema UthldihUrethral discharge Erosion Ulcers Chancres Atrophy HyperHyper--or Hypopigmentation Nodule or tumor Other cutaneous findings: generalized or scattered Evaluation Laboratory Evaluation DarkDark--fieldfield preparation Tzanck preparation Potassium hydroxide preparation Gram’s stain HIV/syphilis serology Bacterial/mycotic cultures Biopsy -

12 Complications and Diseases Associated with Atopic Eczema
Chapter 12 Complications and Diseases Associated 12 with Atopic Eczema D. Vieluf, J. Rieker, T. Ruzicka 12.1 Introduction 12.2 Numerous factors lead to great difficulties in assessing Infections in Atopic Eczema: General Remarks the possible complications and diseases associated with atopic eczema (AE) [134, 281]. A major problem As yet, it is still controversial whether the increased iscorrectdiagnosisofAE,whichhasonlyrecently susceptibility to and severity of different viral, mycotic, been subjected to a certain standardization [31, 76, and bacterial skin infections in AE is a direct conse- 124, 133, 135, 136, 138, 140, 183, 236, 309, 347, 393]. A quence of defective cell-mediated immunity and/or survey of the innumerable case reports and review other immunological abnormalities [31, 125, 133, 135, articles dealing with this topic is hampered by the vari- 159, 189, 244, 287, 301, 303, 309] or is due to a defective able definition of AE and by imprecise description of barrier function of the skin. In addition, eczematous skin lesions, particularly in the nondermatological skin with crusted erosions and excoriations may pro- literature, making proper classification impossible. vide a favorable milieu for the growth and multiplica- Exact epidemiological data concerning the prevalence tion of infectious agents [143, 215]. Finally, prolonged of atopic diseases are rare. Thus, it is even more diffi- topical or systemic glucocorticoid treatment may cult to assess the frequency of diseases associated with enhance the susceptibility of the skin to specific viral or AE, and to answer the question whether the associa- bacterialinfectionsduetoitsimmunosuppressive tion is incidental, rare, frequent, or constant. In addi- effects.