The China Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Of Becoming and Remaining Vegetarian
Wang, Yahong (2020) Vegetarians in modern Beijing: food, identity and body techniques in everyday experience. PhD thesis. http://theses.gla.ac.uk/77857/ Copyright and moral rights for this work are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This work cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Enlighten: Theses https://theses.gla.ac.uk/ [email protected] Vegetarians in modern Beijing: Food, identity and body techniques in everyday experience Yahong Wang B.A., M.A. Submitted in fulfilment of the requirements for the Degree of Doctor of Philosophy School of Social and Political Sciences College of Social Sciences University of Glasgow March 2019 1 Abstract This study investigates how self-defined vegetarians in modern Beijing construct their identity through everyday experience in the hope that it may contribute to a better understanding of the development of individuality and self-identity in Chinese society in a post-traditional order, and also contribute to understanding the development of the vegetarian movement in a non-‘Western’ context. It is perhaps the first scholarly attempt to study the vegetarian community in China that does not treat it as an Oriental phenomenon isolated from any outside influence. -

Fun with Foodella
Fun with Foodella Fun with Foodella is a nutrition education activity book designed for second grade students. This is the second major revision of the original Food Fun with Foodella, which was undertaken as a pilot project by seven South Dakota elementary school teachers in the summer of 1975 to strengthen nutrition education for students at the second grade level. The first revision occurred in 1992. This revision and reprinting was initiated at the prompting of elementary teachers who had previously used the workbook in their classes. The 2006 Fun with Foodella follows the updated food guidance system known as MyPyramid introduced by the U.S. Department of Agriculture in 2005. Using the Teacher’s Guide The Fun with Foodella Teacher’s Guide provides the objectives and directions for each unit of the Fun with Foodella workbook. The directions include the background information necessary to teach each unit. Also, for each unit, additional ideas/activities are provided to further enhance and reinforce the student’s learning. Please be aware that by nature websites and web addresses change over the course of time. Hopefully we have provided enough background with each website given that you will be able to find additional information as necessary. 1 Acknowledgements The researching, writing and graphics necessary to move Fun with Foodella into the electronic age as well as make it compatible with the U.S. Department of Agriculture’s MyPyramid, involved time and input from a myriad of people. It involved individuals from the South Dakota departments of Health and Education, South Dakota State University, Lower Brule Community College and the private sector. -

Subethnic Variation in the Diets of Moslem, Sikh and Hindu Pregnant Women at Sorrento Maternity Hospital, Birmingham
Downloaded from https://doi.org/10.1079/BJN19840114 British Journal of Nutrition (1984), 52, 469-476 469 https://www.cambridge.org/core Subethnic variation in the diets of Moslem, Sikh and Hindu pregnant women at Sorrento Maternity Hospital, Birmingham BY P. A. WHARTON, P. M. EATON* AND B. A. WHARTONT Sorrento Maternity Hospital, Birmingham B13 9HE . IP address: (Received 25 January 1984 - Accepted 1 June 1984) 1. The previous paper (Eaton et al. 1984) described the nutrient intake of pregnant Asian women attending 170.106.202.226 Sorrento Maternity Hospital, Birmingham using the weighed and recall methods. The present paper describes the subethnic variation in nutrient intake by comparing the results from Pakistanis, Sikhs, Hindus and Bangladeshis and also describes food eaten by the pregnant women. 2. Generally. Sikhs had the highest intake of most nutrients (mean energy 7.5 MJ (1800 kcal)/d) and the greatest variety of foods; they ate chapatti and paratha but few ate meat. Hindus had a very similar diet but more ate , on meat, chicken and rice. Pakistanis had an energy intake about 10% below that of the Sikhs and Hindus; meat was eaten, and intake of fruit, and therefore vitamin C, was quite large. Bangladeshis were the smallest women; 29 Sep 2021 at 14:11:24 they had the lowest intake of energy (mean energy 6.5 MJ (1555 kcal)/d) and most nutrients, except for protein, so that 15% of energy was provided by protein. Fish, rice and a low-fat intake were other features of their diet. 3. From a nutritional standpoint, peoples coming from the Asian subcontinent should be divided into subethnic groups; the collective term ‘Asian’ is insufficient. -

Vegetables, Fruits, Whole Grains, and Beans
Vegetables, Fruits, Whole Grains, and Beans Session 2 Assessment Background Information Tips Goals Vegetables, Fruit, Assessment of Whole Grains, Current Eating Habits and Beans On an average DAY, how many servings of these Could be Needs to foods do you eat or drink? Desirable improved be improved 1. Greens and non-starchy vegetables like collard, 4+ 2-3 0-1 mustard, or turnip greens, salads made with dark- green leafy lettuces, kale, broccoli, cauliflower, Brussels sprouts, carrots, okra, zucchini, squash, turnips, onions, cabbage, spinach, mushrooms, bell peppers, or tomatoes (including tomato sauce) 2. Fresh, canned (in own juice or light syrup), or 3+ 1-2 0 frozen fruit or 100% fruit juice (½ cup of juice equals a serving) 3a. Bread, rolls, wraps, or tortillas made all or mostly Never Some Most of with white flour of the time the time 3b. Bread, rolls, wraps, or tortillas made all or mostly Most Some Never with whole wheat flour of the time of the time In an average WEEK, how many servings of these foods do you eat? 4. Starchy vegetables like acorn squash, butternut 4-7 2-3 0-1 squash, beets, green peas, sweet potatoes, or yams (do not include white potatoes) 5. White potatoes, including French fries and 1 or less 2-3 4+ potato chips 6. Beans or peas like pinto beans, kidney beans, 3+ 1-2 0 black beans, lentils, butter or lima beans, or black-eyed peas Continued on next page Vegetables, Fruit, Whole Grains, and Beans 19 Vegetables, Fruit, Whole Grains, Assessment of and Beans Current Eating Habits In an average WEEK, how often or how many servings of these foods do you eat? 7a. -
Eating for 2 Degrees New and Updated Livewell Plates Summary Report © J Oh N D a I E Ls / WWF
EATING FOR 2 DEGREES NEW AND UPDATED LIVEWELL PLATES SUMMARY REPORT © J OH N D A N I E LS / WWF Cover photo © Kelly Sillaste / Getty Images / WWF Contributors Gerard Kramer, Bart Durlinger, Lody Kuling, Willem-Jan van Zeist, Hans Blonk, Roline Broekema, Sarah Halevy Design madenoise.com CONTENTS May 2017 FOREWORD .............................................................................................4 About WWF KEY FINDINGS ........................................................................................6 WWF is the world’s leading independent conservation organisation. We’re CAll TO ACTION ...................................................................................7 creating solutions to the most important environmental challenges facing the WHAT WE SET OUT TO DO ...............................................................8 planet. We work with communities, businesses and governments in over METHODOLOGY .....................................................................................9 100 countries to help people and nature thrive. Together, we’re safeguarding the LIVEWell PRINCIPLES .................................................................... 10 natural world, tackling dangerous climate change and enabling people to use only ADULT 2020 PlATE ...........................................................................11 their fair share of natural resources. ADULT 2030 PlATE .......................................................................... 12 Food is at the heart of many key environmental issues -

Healthy Eating Continued…
Whole Grain, Plant-based Lifestyle What is a Whole Grain, Plant-based Lifestyle (WGPB)? This type of lifestyle involves the elimination of all animal-based products, including meat, dairy and eggs. Also included in the diet are unprocessed or minimally processed grains. Although, similar to a vegan diet, it is not the same. There are different motivations behind adopting such a lifestyle. A WGPB lifestyle focuses on plants, including fruits, vegetables, whole grains, legumes, seeds and nuts. One of the main reasons to choose this lifestyle is the many health benefits. It can assist with weight-loss since it is full of fiber and high water content, which causes you to feel full sooner. Additionally, studies have shown that individuals who adhere to a WGPB diet have improved blood glucose levels. Therefore, those who are diabetic can decrease their need for medications. What are some other benefits? Plant-based foods are loaded with healthy fats, vitamins, minerals, and phytochemicals which improve skin clarity. Vitamin C, for instance, is a great antioxidant that can be found in foods such as; broccoli, papaya, apricot, and bell peppers. They assist in stimulating collagen production, smoothing lines and reducing wrinkles. As a result of the elimination of processed foods, sugars and flour, individuals have found an increase in energy due to decreased spikes in sugar levels. A WGPB diet consists of a clean source of protein, carbohydrates and fruits that help sustain a natural energy level. Another benefit is the increase in our gut’s natural flora, the bacteria that creates a healthy microbiome. -

Upfield Plant-Based Spreads and Margarine Vs. Dairy Butter
Upfield plant-based spreads and margarine vs. dairy butter Life Cycle Assessment Technical Summary March 2020 Version 1 PLANT-BASED SPREADS AND MARGARINE VS. DAIRY BUTTER. LCA TECHNICAL SUMMARY 1 LIFE CYCLE ASSESMENT …….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….. 3 METHOD …….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…... 3 CRITICAL REVIEW …….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….3 FUNCTIONAL UNIT ………….…….…….…….…….…….…….…….…….…….…….…….…….…….…….……….. 3 ENVIRONMENTAL IMPACT INDICATORS CONSIDERED ……….…….…….…….…….…….…….…..….. 3 FROM FARM-TO-PLATE ……..…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….. 4 DATA COLLECTION AND MODELLING………….…….…….…….…….…….…….…….…….…….…….……... 4 RESULTS AND DISCUSSION …….…….…….…….…….…….…….…….…….…….…….…….…….…….……….. 5 CLIMATE CHANGE IMPACTS ………….…….…….…….…….…….…….…….…….…….…….…….…….……... 5 FRESHWATER CONSUMPTION ……….…….…….…….…….…….…….…….…….…….…….…….………..….. 6 LAND OCCUPATION ………….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….... 6 LCA CONCLUSIONS AND OUTLOOK ………….…….…….…….…….…….…….…….…….…….…….………... 7 CALCULATION OF EQUIVALENCIES ………….…….…….…….…….…….…….…….…….…….…….………... 8 ABOUT QUANTIS ………….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….. 9 REFERENCES ……….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….…….……….. 9 PLANT-BASED SPREADS AND MARGARINE VS. DAIRY BUTTER. LCA TECHNICAL SUMMARY 2 In 2018 Quantis conducted a Life Cycle Assessment (LCA) of Upfield’s plant-based spreads and margarines in 21 European and North American markets. These products were compared to dairy butter sold in the same -
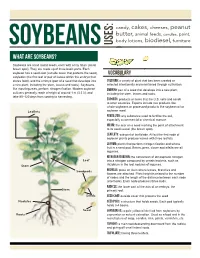
What Are Soybeans?
candy, cakes, cheeses, peanut butter, animal feeds, candles, paint, body lotions, biodiesel, furniture soybeans USES: What are soybeans? Soybeans are small round seeds, each with a tiny hilum (small brown spot). They are made up of three basic parts. Each soybean has a seed coat (outside cover that protects the seed), VOCABULARY cotyledon (the first leaf or pair of leaves within the embryo that stores food), and the embryo (part of a seed that develops into Cultivar: a variety of plant that has been created or a new plant, including the stem, leaves and roots). Soybeans, selected intentionally and maintained through cultivation. like most legumes, perform nitrogen fixation. Modern soybean Embryo: part of a seed that develops into a new plant, cultivars generally reach a height of around 1 m (3.3 ft), and including the stem, leaves and roots. take 80–120 days from sowing to harvesting. Exports: products or items that the U.S. sells and sends to other countries. Exports include raw products like whole soybeans or processed products like soybean oil or Leaflets soybean meal. Fertilizer: any substance used to fertilize the soil, especially a commercial or chemical manure. Hilum: the scar on a seed marking the point of attachment to its seed vessel (the brown spot). Leaflets: sub-part of leaf blade. All but the first node of soybean plants produce leaves with three leaflets. Legume: plants that perform nitrogen fixation and whose fruit is a seed pod. Beans, peas, clover and alfalfa are all legumes. Nitrogen Fixation: the conversion of atmospheric nitrogen Leaf into a nitrogen compound by certain bacteria, such as Stem rhizobium in the root nodules of legumes. -

Review of the China Study
FACT SHEET REVIEW OF THE CHINA STUDY By Team, General Conference Nutrition Council In 1905 Ellen White described the diet our Creator chose for us as a balanced plant-based diet including foods such as grains, fruit and vegetables, and nuts (1). Such a diet provides physical and mental vigor and endurance. She also recognized that such a diet may need to be adjusted according to the season, the climate, occupation, individual tolerance, and what foods are locally available (2). The General Conference Nutrition Council (GCNC) therefore recommends the consumption of a balanced vegetarian diet consisting of a rich variety of plant-based foods. Wherever possible those should be whole foods. Thousands of peer-reviewed research papers have been published over the last seven decades validating a balanced vegetarian eating plan. With so much support for our advocacy of vegetarian nutrition we have no need to fortify our well-founded position with popular anecdotal information or flawed science just because it agrees with what we believe. The methods used to arrive at a conclusion are very important as they determine the validity of the conclusion. We must demonstrate careful, transparent integrity at every turn in formulating a sound rationale to support our health message. It is with this in mind that we have carefully reviewed the book, The China Study (3). This book, published in 2004, was written by T. Colin Campbell, PhD, an emeritus professor of Nutritional Biochemistry at Cornell University and the author of over 300 research papers. In it Campbell describes his personal journey to a plants-only diet. -

Soy Free Diet Avoiding Soy
SOY FREE DIET AVOIDING SOY An allergy to soy is common in babies and young children, studies show that often children outgrow a soy allergy by age 3 years and the majority by age 10. Soybeans are a member of the legume family; examples of other legumes include beans, peas, lentils and peanut. It is important to remember that children with a soy allergy are not necessarily allergic to other legumes, request more clarification from your allergist if you are concerned. Children with a soy allergy may have nausea, vomiting, abdominal pain, diarrhea, bloody stool, difficulty breathing, and or a skin reaction after eating or drinking soy products. These symptoms can be avoided by following a soy free diet. What foods are not allowed on a soy free diet? Soy beans and edamame Soy products, including tofu, miso, natto, soy sauce (including sho yu, tamari), soy milk/creamer/ice cream/yogurt, soy nuts and soy protein, tempeh, textured vegetable protein (TVP) Caution with processed foods - soy is widely used manufactured food products – remember to carefully read labels. o Soy products and derivatives can be found in many foods, including baked goods, canned tuna and meat, cereals, cookies, crackers, high-protein energy bars, drinks and snacks, infant formulas, low- fat peanut butter, processed meats, sauces, chips, canned broths and soups, condiments and salad dressings (Bragg’s Liquid Aminos) USE EXTRA CAUTION WITH ASIAN CUISINE: Asian cuisine are considered high-risk for people with soy allergy due to the common use of soy as an ingredient and the possibility of cross-contamination, even if a soy-free item is ordered. -

Food Habits and Nutritional Status of East Indian Hindu
FOOD HABITS AND NUTRITIONAL STATUS OF EAST INDIAN HINDU CHILDREN IN BRITISH COLUMBIA by CLARA MING LEE£1 B.Sc.(Food Science), McGill University, 1975 A THESIS.: SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE in the Division of HUMAN NUTRITION SCHOOL OF HOME ECONOMICS We accept this thesis as confirming to the required standard. THE UNIVERSITY OF BRITISH COLUMBIA September, 1977 fcT) CLARA MING LEE PI, 1978 In presenting this thesis in partial fulfilment of the requirements for an advanced degree at the University of British Columbia, I agree that the Library shall make it freely available for reference and study. I further agree that permission for extensive copying of this thesis for scholarly purposes may be granted by the Head of my Department or by his representatives. It is understood that copying or publication of this thesis for financial gain shall not be allowed without my written permission. Department of HOME ECONOMICS The University of British Columbia 2075 Wesbrook Place Vancouver, Canada V6T 1WS FEB 8, 1978 i ABSTRACT A cross-sectional study was carried out to assess the nutritional stutus of a sample of East Indian children in the Vancouver area. The study sample consisted of 132 children from 3 months to 1$ years of age, whose parents belonged to the congregation of the Vishwa Hindu Parished Temple in Bur- naby, B.C. In the dietary assessment of nutritional status, a 24-hour diet recall and a food habits questionnaire were em• ployed on the 132 children. The Canadian Dietary Standard (revised 1975) and Nutrition Canada categories were used for an evaluation of their dietary intake. -

5 a Day Month Recipes
Fruit and Veggie Recipes Out of This Whirled Shake Preparation Time: 5 minutes Makes 2 servings (½ cup fruit per person) ½ banana, peeled and sliced 1 cup unsweetened frozen berries (strawberries, blueberries, and/or blackberries) ½ cup low fat (1%) milk or soft tofu ½ cup 100% orange juice • Place all ingredients in a blender container. Cover tightly. • Blend until smooth. If mixture is too thick, add ½ cup cold water and blend again. • Pour into 2 glasses and serve. Nutrients per serving made with low fat milk and blueberries: 120 calories, 1g fat, 0g saturated fat, 0g trans fat, 5mg cholesterol, 40mg sodium, 26g carbohydrate, 3g dietary fiber, 3g protein. Diabetic Exchanges: 2 fruit. This set of recipes was originally developed by the Network for a Healthy California and has been adapted by the New Hampshire Fruit and Vegetable Program in collaboration with the Centers for Disease Control and Prevention (CDC) to meet the Fruits & Veggies—More Matters® recipe criteria. NH DHHS y DPHS y Fruit and Vegetable Program y 603-271-4830 y www.dhhs.nh.gov/DHHS/NHP/fruitsandveggies y Jan 2008 y Page 1 of 10 Oprah’s Outtasight Salad Makes 4 servings (½ cup fruits and vegetables per person) Preparation Time: 20 minutes Salad 2 cups salad greens of your choice 1 cup chopped vegetables of your choice (tomatoes, cucumbers, carrots, green beans) 1 cup fresh orange segments or canned* pineapple chunks, drained (canned fruit packed in 100% fruit juice) ¼ cup Dynamite Dressing 2 tablespoons raisins or dried cranberries 2 tablespoons chopped nuts, any kind *canned fruit packed in 100% fruit juice.