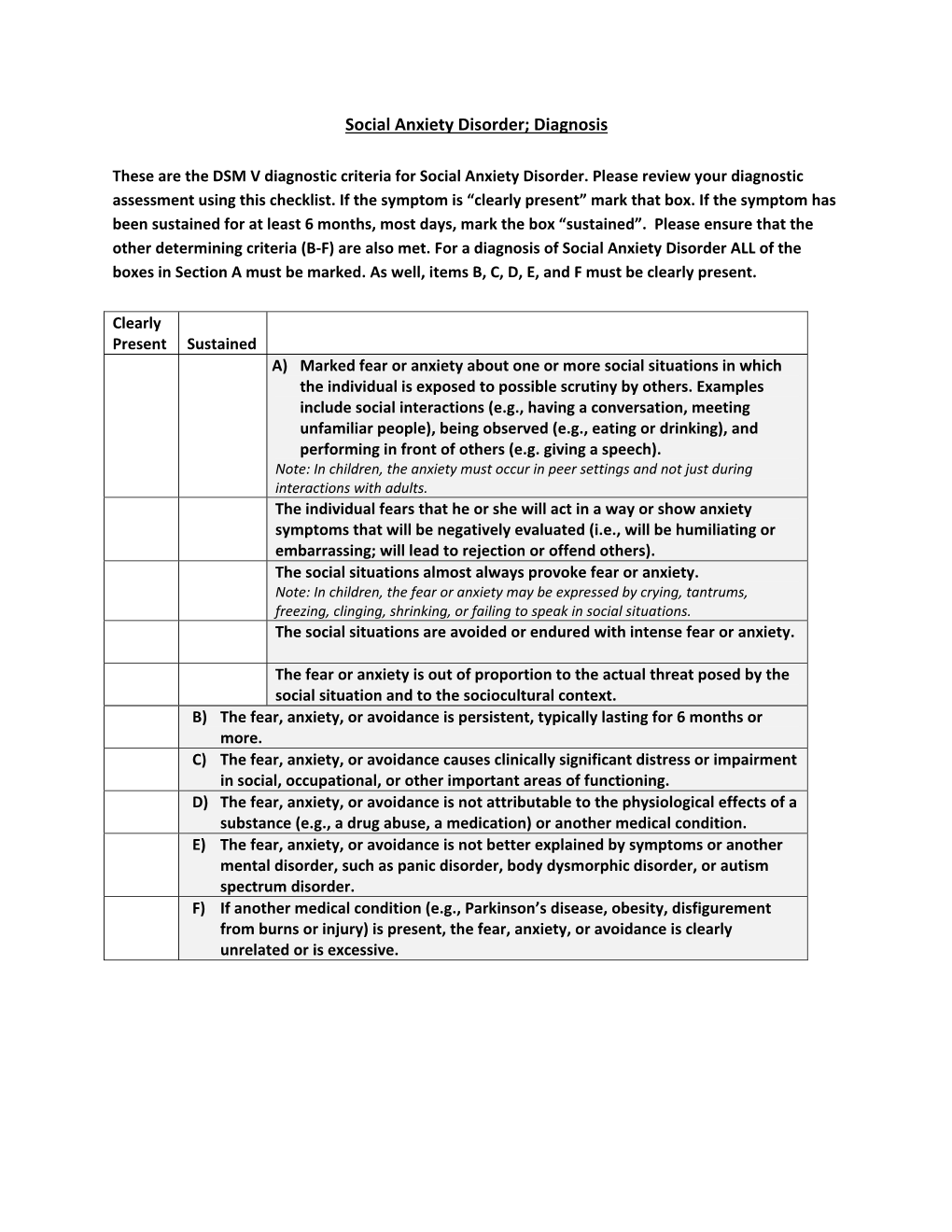
Social Anxiety Disorder; Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bipolar Disorder in ADULTS the Disorder, Its Treatment and Prevention
Bipolar lidelse hos voksne, engelsk Information about BIPOLAR DISORDER IN ADULTS The disorder, its treatment and prevention Psykiatri og Social psykinfomidt.dk CONTENTS 03 What is bipolar disorder? 04 What causes bipolar disorder? 06 What are the symptoms of bipolar disorder? 09 How is bipolar disorder diagnosed? 10 Different progressions and modes of expression 11 How can bipolar disorder be treated and prevented? 14 What can you do to help yourself if you have bipolar disorder? 16 What can your loved ones do? Bipolar affective disorder (the term we will use in this publication is “bipolar disorder”) is a serious mental disorder. When a person has bipolar disorder, knowledge of the illness is important. The more you know, the better you can handle and prevent the illness and its consequences. This brochure describes the illness as well as options for its treatment and prevention. It is mainly intended for people being treated for bipolar disorder by the psychiatric service in Region Midtjylland. We hope this brochure will help you and your loved ones to learn more about the diagnosis of bipolar disorder. Kind regards The psychiatric service in Region Midtjylland Tingvej 15, 8800 Viborg Tel.: 7841 0000 Bipolar disorder in adults WHAT IS BIPOLAR DISORDER? Bipolar disorder is a mental illness lot in terms of reducing the progression characterised by episodes of mania, of symptoms and decreasing the hypomania (a mild form of mania), psychological and social costs to the depression and/or mixed state (a state individual and the family. where manic and depressive symptoms coexist or occur in rapid succession). -
Autistic Traits and Social Anxiety Predict Differential Performance on Social Cognitive Tasks in Typically Developing Young Adults
W&M ScholarWorks Arts & Sciences Articles Arts and Sciences 3-29-2018 Autistic traits and social anxiety predict differential performance on social cognitive tasks in typically developing young adults. Cheryl L. Dickter College of William and Mary, [email protected] J A. Burk K M. Fleckenstein C T. Kozikowski Follow this and additional works at: https://scholarworks.wm.edu/aspubs Part of the Cognitive Psychology Commons Recommended Citation Dickter, Cheryl L.; Burk, J A.; Fleckenstein, K M.; and Kozikowski, C T., Autistic traits and social anxiety predict differential performance on social cognitive tasks in typically developing young adults. (2018). PLoS ONE, 13(3). https://doi.org/10.1371/journal.pone.0195239 This Article is brought to you for free and open access by the Arts and Sciences at W&M ScholarWorks. It has been accepted for inclusion in Arts & Sciences Articles by an authorized administrator of W&M ScholarWorks. For more information, please contact [email protected]. RESEARCH ARTICLE Autistic traits and social anxiety predict differential performance on social cognitive tasks in typically developing young adults Cheryl L. Dickter1*, Joshua A. Burk1, Katarina Fleckenstein1, C. Teal Kozikowski1,2 1 Psychological Sciences, College of William & Mary, Williamsburg, VA, United States of America, 2 Psychiatry & Behavioral Sciences, Eastern Virginia Medical School, Norfolk, VA, United States of America * [email protected] Abstract a1111111111 The current work examined the unique contribution that autistic traits and social anxiety a1111111111 a1111111111 have on tasks examining attention and emotion processing. In Study 1, 119 typically-devel- a1111111111 oping college students completed a flanker task assessing the control of attention to target a1111111111 faces and away from distracting faces during emotion identification. -

Social Anxiety Disorder in Psychosis: a Critical Review
Chapter 7 Social Anxiety Disorder in Psychosis: A Critical Review Maria Michail Additional information is available at the end of the chapter http://dx.doi.org/10.5772/53053 1. Introduction Eugene Bleuler was one of the first to emphasize the importance of affect and its pro‐ nounced impact upon the course and outcome of psychosis. The famous “Krapelian dichtoco‐ my” which supported the clear distinction between mood and psychotic illnesses on the basis of etiological origins, symptomatology, course and outcome was first challenged by Bleuler. Bleuler recognized the disorders of affect as one of the four primary symptoms (blunted 'Affect', loosening of 'Associations', 'Ambivalence', and 'Autism') of schizophrenia, as opposed to delusions and hallucinations which were perceived as secondary. Bleuler further postulated the incongruity between emotions and thought content in people with schizo‐ phrenia as well as their diminished or complete lack of emotional responsiveness. Bleuler’s recognition of the importance of affective disturbances in schizophrenia has influenced cur‐ rent diagnostic definitions and criteria of schizophrenia. The sharp distinction between affect and psychosis which has dominated both research and clinical practice during the nineteenth and twentieth century has gradually been abandoned. New evidence from epidemiological, familial and molecular genetic studies (Cardno et al, 2005; Craddock et al, 2005; Craddock & Owen, 2005) have come to light demonstrating the endemic nature of affective disturbances in psychosis. In a twin study by Cardno et al (2002), the authors identified significant overlap in risk factors between the schizophrenic, schizoaffective and manic syndromes. Specifically, considerable genetic correlations were reported between the schizophrenic and manic syndromes. -

Psychiatric Assessment of Severe Presentations in Autism Spectrum Disorders and Intellectual Disability
Psychiatric Assessment of Severe Presentations in Autism Spectrum Disorders and Intellectual Disability a,b, b Bryan H. King, MD *, Nina de Lacy, MD , c,d,e Matthew Siegel, MD KEYWORDS Autism Intellectual disability Self-injury Aggression Hyperactivity Psychiatric evaluation KEY POINTS Psychiatric illnesses are common in autism spectrum disorder (ASD)/intellectual disability (ID). Externalizing behaviors are common presenting symptoms but are etiologically nonspecific. Genetic conditions associated with ASD/ID may inform medical surveillance as well as potential therapeutics. Co-occurring medical conditions are common in ASD/ID and may contribute to symptom presentation. Environmental factors, for example, change in caregiver or experience of trauma, may be particularly significant in the setting of ASD/ID. INTRODUCTION Decades ago, Sovner and Hurley1 somewhat rhetorically debated whether individ- uals with ID experience affective illness. Although the answer then as now is an un- equivocal yes, uncertainty does remain as to how the presentation of psychiatric Disclosure Statement: B.H. King has received research funding and has served as a consultant for Seaside Therapeutics and Roche. Drs N. de Lacy and M. Siegel report no financial disclosures. a Department of Psychiatry and Behavioral Medicine, Seattle Children’s Autism Center, Seattle Children’s Hospital, Seattle, WA, USA; b Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA, USA; c Developmental Disorders Program, Spring Harbor Hospital, ME, USA; d Tufts University School of Medicine, Boston, MA, USA; e Maine Medical Center Research Institute, ME, USA * Corresponding author. E-mail address: [email protected] Child Adolesc Psychiatric Clin N Am 23 (2014) 1–14 http://dx.doi.org/10.1016/j.chc.2013.07.001 childpsych.theclinics.com 1056-4993/14/$ – see front matter Ó 2014 Elsevier Inc. -
An Evidence Based Guide to Anxiety in Autism
Academic excellence for business and the professions The Autism Research Group An Evidence Based Guide to Anxiety in Autism Sebastian B Gaigg, Autism Research Group City, University of London Jane Crawford, Autism and Social Communication Team West Sussex County Council Helen Cottell, Autism and Social Communication Team West Sussex County Council www.city.ac.uk November 2018 Foreword Over the past 10-15 years, research has confirmed what many parents and teachers have long suspected – that many autistic children often experience very significant levels of anxiety. This guide provides an overview of what is currently known about anxiety in autism; how common it is, what causes it, and what strategies might help to manage and reduce it. By combining the latest research evidence with experience based recommendations for best practice, the aim of this guide is to help educators and other professionals make informed decisions about how to promote mental health and well-being in autistic children under their care. 3 Contents What do we know about anxiety in autism? 5 What is anxiety? 5 How common is anxiety and what does it look like in autism? 6 What causes anxiety in autism? 7-9 Implications for treatment approaches 10 Cognitive Behaviour Therapy 10 Coping with uncertainity 11 Mindfulness based therapy 11 Tools to support the management of anxiety in autism 12 Sensory processing toolbox 12-13 Emotional awareness and alexithymia toolbox 14-15 Intolerance of uncertainty toolbox 16-17 Additional resources and further reading 18-19 A note on language in this guide There are different preferences among members of the autism community about whether identity-first (‘autistic person’) or person-first (‘person with autism’) language should be used to describe individuals who have received an autism spectrum diagnosis. -

Social Anxiety Disorder in First-Episode Psychosis: Incidence, Phenomenology and Relationship with Paranoia Maria Michail and Max Birchwood
The British Journal of Psychiatry (2009) 195, 234–241. doi: 10.1192/bjp.bp.108.053124 Social anxiety disorder in first-episode psychosis: incidence, phenomenology and relationship with paranoia Maria Michail and Max Birchwood Background Social anxiety disorder constitutes a significant problem avoidance and depression. Social anxiety in psychosis was for people with psychosis. It is unclear whether this is not related to the positive symptoms of the Positive and a by-product of persecutory thinking. Negative Syndrome Scale (PANSS) including suspiciousness/ persecution. However, a significantly greater percentage of Aims socially anxious v. non-socially anxious individuals with To compare the phenomenology of social anxiety disorder in psychosis expressed perceived threat from persecutors, first-episode psychosis with that in a group without although this did not affect the severity of social anxiety psychosis. The relationship between social anxiety and within the FEP/SaD group. The majority of those in the FEP/ psychosis symptoms was investigated. SaD group did not have concurrent persecutory delusions. Method Conclusions A sample of people with first-episode psychosis (FEP group) Social anxiety is a significant comorbidity in first-episode was compared with a sample with social anxiety disorder psychosis. It is not simply an epiphenomenon of psychotic without psychosis (SaD group). symptoms and clinical paranoia, and it has more than one causal pathway. For a subgroup of socially anxious people Results with psychosis, anticipated harm is present and the Of the individuals in the FEP group (n = 80) 25% were processes that underlie its relationship with social anxiety diagnosed with an ICD–10 social anxiety disorder (FEP/SaD warrant further investigation. -

Mental Health and Chronic Diseases CDC Fact Sheet
Mental Health and Chronic Diseases Issue Brief No. 2 October 2012 Background Chronic diseases are non-communicable illnesses that are prolonged in duration, do not resolve spontaneously, and are rarely cured completely. They are the leading cause of death and disability in the United States. They cause 7 out of 10 deaths each year and are among the most preventable and treatable of all health problems (see figure below). Chronic diseases include illness such as heart disease, diabetes, cancer, and arthritis.1 Mental health disorders are medical conditions that disrupt a person's thinking, feeling, mood, ability to relate to others and daily functioning. They are medical conditions that often result in a reduced ability to cope with the routine daily activities such as going to work or raising a family. Just like chronic diseases, mental health disorders are treatable. Most people diagnosed with a serious mental health disorder can receive relief from their symptoms by following a treatment plan specifically designed for them by a trained psychologist or psychiatrist. Mental health disorders are not exclusive to those who exhibit a lack of personal strength, personality traits like being shy, or have a certain socioeconomic status. Mental health disorders include illnesses such as major depression, bipolar disorder, obsessive compulsive disorder, and post-traumatic stress disorder. One common finding is that people who suffer from a chronic disease are more likely to also suffer from depression.2 Scientists have yet to determine if having a chronic disease increases the prevalence of depression or depression increases the risk of obtaining a chronic disease. -

Mental Health Disorders by David Murphey, Ph.D., Megan Barry, B.A., and Brigitte Vaughn, M.S
ADOLESCENT HEALTH HIGHLIGHT Publication # 2013-1 January 2013 Fast Facts Mental Health Disorders By David Murphey, Ph.D., Megan Barry, B.A., and Brigitte Vaughn, M.S. Mental disorders are diagnosable conditions characterized by changes in Mental disorders in adolescence are 1. thinking, mood, or behavior (or some combination of these) that can cause a common: An estimated one in five person to feel stressed out and impair his or her ability to function. These adolescents has a diagnosable disorders are common in adolescence. This Adolescent Health Highlight disorder.1 presents the warning signs of mental disorders; describes the types of mental disorders and their prevalence and trends; discusses the 2. Adolescence is the time when many consequences and risk of mental disorders; presents treatment options and mental disorders first arise. More barriers to accessing mental health care; and provides mental health than half of all mental disorders and resources. problems with substance abuse The definition and complexities of mental disorders (such as binge drinking and illegal drug use) begin by age 14.2 Medical science increasingly recognizes the vital link between a person’s physical health and his or her mental/emotional health. Mind and body are connected as one, each affected by the other, and both are influenced by a 3. The most prevalent mental disorder person’s genetic inheritance, environment, and experience. Just as the experienced among adolescents is 4 absence of disease does not adequately define physical health, mental depression, with more than one in health consists of more than the absence of mental disorders. Mental health four high school students found to is best seen as falling along a continuum, which fluctuates over time, and have at least mild symptoms of this across individuals, as well as within a single individual.3 condition.5 As defined in this Highlight, mental disorders are diagnosable conditions characterized by changes in thinking, mood, or behavior (or some 4. -

Cognitive-Behavioral Treatment of Social Anxiety Disorder and Comorbid Paranoid Schizophrenia Monnica T
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Faculty Publications, Department of Psychology Psychology, Department of 2015 Cognitive-Behavioral Treatment of Social Anxiety Disorder and Comorbid Paranoid Schizophrenia Monnica T. Williams University of Louisville, [email protected] Michelle C. Capozzoli University of Nebraska–Lincoln, [email protected] Erica V. Buckner University of Louisville David Yuska University of Pennsylvania Follow this and additional works at: https://digitalcommons.unl.edu/psychfacpub Part of the Clinical Psychology Commons, and the Personality and Social Contexts Commons Williams, Monnica T.; Capozzoli, Michelle C.; Buckner, Erica V.; and Yuska, David, "Cognitive-Behavioral Treatment of Social Anxiety Disorder and Comorbid Paranoid Schizophrenia" (2015). Faculty Publications, Department of Psychology. 711. https://digitalcommons.unl.edu/psychfacpub/711 This Article is brought to you for free and open access by the Psychology, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Faculty Publications, Department of Psychology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Published in Clinical Case Studies 14:5 (2015), pp. 323– 341. doi 10.1177/1534650114559717 Copyright © 2014 Monnica T. Williams, Michelle C. Capozzoli, Erica V. Buckner, and David Yusko; published by SAGE Publications. Used by permission. digitalcommons.unl.edu Cognitive-Behavioral Treatment of Social Anxiety Disorder -

The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research
The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research World Health Organization Geneva The World Health Organization is a specialized agency of the United Nations with primary responsibility for international health matters and public health. Through this organization, which was created in 1948, the health professions of some 180 countries exchange their knowledge and experience with the aim of making possible the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life. By means of direct technical cooperation with its Member States, and by stimulating such cooperation among them, WHO promotes the development of comprehensive health services, the prevention and control of diseases, the improvement of environmental conditions, the development of human resources for health, the coordination and development of biomedical and health services research, and the planning and implementation of health programmes. These broad fields of endeavour encompass a wide variety of activities, such as developing systems of primary health care that reach the whole population of Member countries; promoting the health of mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; coordinating the global strategy for the prevention and control of AIDS; having achieved the eradication of smallpox, promoting mass immunization against a number of other -

Psychotic Symptoms in Social Anxiety Disorder with Bipolar
Cartas aos editores Psychotic symptoms in social Discussion The case presented in this letter highlights the relationship anxiety disorder with bipolar- between SA and BD. We observed a patient with SA who, after like progression symptom improvement with antidepressants, had a clear manic phase. Other studies have also reported clinical similarities between Sintomas psicóticos na fobia SA and BD-II3, as well as a link between BD-I and SA: 12.5% of patients with BD-I also have SA4. Himmelhoch3 studied the social com evolução bipolar treatment outcome of 32 social anxiety disorder patients and found that 18 had remission (>50%) of their SA symptoms. Moreover, 14 out of those 18 became hypomanic, according to mania scales and expert clinical diagnosis. We found that this patient with SA that Dear Editor, featured a bipolar-like progression experienced manic symptoms, Previously, our research group discovered that there is a sub- and particularly a mixed episode. We identified additional group of social anxiety (SA) patients who improve while taking occurrences of psychotic symptoms related to SA worries, such antidepressants and present a clear hypomanic phase. Without as concern about being accepted by others. the antidepressant, the symptoms of SA return1. SA and bipolar Once patients with SA begin to feel preoccupied with the disorder II (BD-II) patients have a similar number of previous minds of others, they show a predisposition toward psychotic depressive episodes, alcohol abuse, suicide attempts, and family symptoms5. Another predisposing factor in some patients with history of mood disorder1. SA is the observation of bipolar-like progression, which indicates There is a lack of studies on the association between SA the possibility not only of hypomanic episodes but also of manic and mania. -

Autism Spectrum Disorder 299.00 (F84.0)
Autism Spectrum Disorder 299.00 (F84.0) Diagnostic Criteria according to the Diagnostic Statistical Manual V A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive, see text): 1. Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions. 2. Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication. 3. Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts; to difficulties in sharing imaginative play or in making friends; to absence of interest in peers. Specify current severity – Social Communication: Level 1 – Requiring Support 2- Substantial Support 3-Very Substantial Support Please refer to attached table for definition of levels. B. Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text): 1. Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases). 2. Insistence on sameness, inflexible adherence to routines, or ritualized patterns or verbal nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat food every day).