Primary Urethral Cancer Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Radiation Oncology Review
Clinical Radiation Oncology Review Daniel M. Trifiletti University of Virginia Disclaimer: The following is meant to serve as a brief review of information in preparation for board examinations in Radiation Oncology and allow for an open-access, printable, updatable resource for trainees. Recommendations are briefly summarized, vary by institution, and there may be errors. NCCN guidelines are taken from 2014 and may be out-dated. This should be taken into consideration when reading. 1 Table of Contents 1) Pediatrics 6) Gastrointestinal a) Rhabdomyosarcoma a) Esophageal Cancer b) Ewings Sarcoma b) Gastric Cancer c) Wilms Tumor c) Pancreatic Cancer d) Neuroblastoma d) Hepatocellular Carcinoma e) Retinoblastoma e) Colorectal cancer f) Medulloblastoma f) Anal Cancer g) Epndymoma h) Germ cell, Non-Germ cell tumors, Pineal tumors 7) Genitourinary i) Craniopharyngioma a) Prostate Cancer j) Brainstem Glioma i) Low Risk Prostate Cancer & Brachytherapy ii) Intermediate/High Risk Prostate Cancer 2) Central Nervous System iii) Adjuvant/Salvage & Metastatic Prostate Cancer a) Low Grade Glioma b) Bladder Cancer b) High Grade Glioma c) Renal Cell Cancer c) Primary CNS lymphoma d) Urethral Cancer d) Meningioma e) Testicular Cancer e) Pituitary Tumor f) Penile Cancer 3) Head and Neck 8) Gynecologic a) Ocular Melanoma a) Cervical Cancer b) Nasopharyngeal Cancer b) Endometrial Cancer c) Paranasal Sinus Cancer c) Uterine Sarcoma d) Oral Cavity Cancer d) Vulvar Cancer e) Oropharyngeal Cancer e) Vaginal Cancer f) Salivary Gland Cancer f) Ovarian Cancer & Fallopian -

Glickman Urological & Kidney Institute
C L E V E GLICKMAN UROLOGICAL L A N D C L I N I C & KIDNEY INSTITUTE | G L I C K 2019 Year in Review M The Cleveland Clinic Foundation A N 9500 Euclid Ave. / AC311 U R O Cleveland, OH 44195 L O G I C A L & K I D N E Y I N S T I T U T E | 2 0 1 9 Y E A R I N R E V I E W 19-URL-5068 22877_CCFBCH_19URL4030_19URL5068_ACG.indd 29-31 2/6/20 3:06 PM CONTENTS 3 Glickman Kidney & Urological Institute at a Glance 7 Message from the Chairman 9 Two Clinical Trials, One Ambitious Goal to Personalize Kidney Medicine 11 A New Paradigm for Advanced Prostate Cancer Clinical Trials 13 Another Landmark Year for Cleveland Clinic’s Kidney Transplant Program 15 Getting It Right: Nephrologists Are Working to Minimize the ‘White-Coat Effect’ for Patients with Hypertension 17 ‘A FitBit for the Bladder’: UroMonitor Takes Monitoring Out of the Clinic 19 Virtual Reality Tool to Offer New Way of Understanding Renal Physiology 21 First Kidney Transplant Performed Using Single-Port Robot 22 2019 Achievements 28 Resources for Physicians ON THE COVER Georges Nakhoul, MD, Director of the Center for Chronic Kidney Disease, launched a virtual reality program to enhance the renal physiology learning experience for trainees. 22877_CCFBCH_19URL4030_19URL5068_ACG.indd 32-34 2/6/20 3:06 PM CLEVELAND CLINIC GLICKMAN UROLOGICAL & KIDNEY INSTITUTE | 3 Glickman Urological AT A GLANCE & Kidney Institute The Glickman Urological BY THE NUMBERS & Kidney Institute’s (2019) activities encompass a unique combination of high- 132,663 volume and challenging OUTPATIENT VISITS clinical cases, extensive basic and translational scientific efforts, and 14,098 innovative laboratory SURGICAL CASES research conducted in an environment that nurtures the future leaders of its 21,255 DIALYSIS TREATMENTS specialties. -

Urinary Bladder Neoplasia
Canine Urinary Tract Neoplasia Phyllis C Glawe DVM, MS The principal organs of the urinary tract are the kidneys, ureters, urinary bladder and urethra. The urinary bladder and urethra are the most commonly affected by cancer in the dog and the majority of cancers in these locations are malignant. The most common type of cancer is Transitional Cell Carcinoma (TCC). This handout reviews the facts about clinical symptoms, diagnosis and treatment of urinary tract cancer in the dog. Clinical Features More common in female dogs, urinary bladder and urethral cancer are typically associated with advanced age (9-10 years). Frequent urination, blood in the urine, and straining to urinate are typical symptoms. These signs are also similar to those of urinary tract infections, thus a cancer diagnosis can be missed early in the course of the disease. If the flow of urine is obstructed, abdominal pain, vomiting, depression and loss of appetite can occur. More rarely, dogs can present with back pain and weakness of the hind limbs due to metastases (spread) of the cancer to the spine and lymph nodes. Diagnosis Abdominal radiographs and abdominal ultrasound can be utilized to detect cancer in the lower urinary tract. Abdominal ultrasound is particularly helpful to assess whether other organs in the abdomen region are affected, such as the kidneys and ureters. Hydronephrosis and hydroureter are terms describing a back-up of urine flow due to the obstructive effects of a tumor. Regional lymph node enlargement and possible prostate enlargement in male dogs can be assessed quickly and accurately with ultrasound. Urine analysis is not very helpful as a diagnostic tool in most cases. -

Primary Urethral Carcinoma
EAU Guidelines on Primary Urethral Carcinoma G. Gakis, J.A. Witjes, E. Compérat, N.C. Cowan, V. Hernàndez, T. Lebret, A. Lorch, M.J. Ribal, A.G. van der Heijden Guidelines Associates: M. Bruins, E. Linares Espinós, M. Rouanne, Y. Neuzillet, E. Veskimäe © European Association of Urology 2017 TABLE OF CONTENTS PAGE 1. INTRODUCTION 3 1.1 Aims and scope 3 1.2 Panel composition 3 1.3 Publication history and summary of changes 3 1.3.1 Summary of changes 3 2. METHODS 3 2.1 Data identification 3 2.2 Review 3 2.3 Future goals 4 3. EPIDEMIOLOGY, AETIOLOGY AND PATHOLOGY 4 3.1 Epidemiology 4 3.2 Aetiology 4 3.3 Histopathology 4 4. STAGING AND CLASSIFICATION SYSTEMS 5 4.1 Tumour, Node, Metastasis (TNM) staging system 5 4.2 Tumour grade 5 5. DIAGNOSTIC EVALUATION AND STAGING 6 5.1 History 6 5.2 Clinical examination 6 5.3 Urinary cytology 6 5.4 Diagnostic urethrocystoscopy and biopsy 6 5.5 Radiological imaging 7 5.6 Regional lymph nodes 7 6. PROGNOSIS 7 6.1 Long-term survival after primary urethral carcinoma 7 6.2 Predictors of survival in primary urethral carcinoma 7 7. DISEASE MANAGEMENT 8 7.1 Treatment of localised primary urethral carcinoma in males 8 7.2 Treatment of localised urethral carcinoma in females 8 7.2.1 Urethrectomy and urethra-sparing surgery 8 7.2.2 Radiotherapy 8 7.3 Multimodal treatment in advanced urethral carcinoma in both genders 9 7.3.1 Preoperative platinum-based chemotherapy 9 7.3.2 Preoperative chemoradiotherapy in locally advanced squamous cell carcinoma of the urethra 9 7.4 Treatment of urothelial carcinoma of the prostate 9 8. -

Sarcomatoid Urothelial Carcinoma Arising in the Female Urethral Diverticulum
Journal of Pathology and Translational Medicine 2021; 55: 298-302 https://doi.org/10.4132/jptm.2021.04.23 CASE STUDY Sarcomatoid urothelial carcinoma arising in the female urethral diverticulum Heae Surng Park Department of Pathology, Ewha Womans University Seoul Hospital, Seoul, Korea A sarcomatoid variant of urothelial carcinoma in the female urethral diverticulum has not been reported previously. A 66-year-old woman suffering from dysuria presented with a huge urethral mass invading the urinary bladder and vagina. Histopathological examination of the resected specimen revealed predominantly undifferentiated pleomorphic sarcoma with sclerosis. Only a small portion of conven- tional urothelial carcinoma was identified around the urethral diverticulum, which contained glandular epithelium and villous adenoma. The patient showed rapid systemic recurrence and resistance to immune checkpoint inhibitor therapy despite high expression of pro- grammed cell death ligand-1. We report the first case of urethral diverticular carcinoma with sarcomatoid features. Key Words: Sarcomatoid carcinoma; Urothelial carcinoma; Urethral diverticulum Received: March 9, 2021 Revised: April 16, 2021 Accepted: April 23, 2021 Corresponding Author: Heae Surng Park, MD, PhD, Department of Pathology, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, 260 Gonghang-daero, Gangseo-gu, Seoul 07804, Korea Tel: +82-2-6986-5253, Fax: +82-2-6986-3423, E-mail: [email protected] Urethral diverticular carcinoma (UDC) is extremely rare; the urinary bladder, and vagina with enlarged lymph nodes at both most common histological subtype is adenocarcinoma [1,2]. femoral, both inguinal, and both internal and external iliac areas Sarcomatoid urothelial carcinoma (UC) is also unusual. Due to (Fig. 1B). -
EAU Guidelines Primary Urethral Carcinomas V2
Guidelines on Primary Urethral Carcinoma G. Gakis, J.A. Witjes, E. Compérat, N.C. Cowan, M. De Santis, T. Lebret, M.J. Ribal, A. Sherif © European Association of Urology 2013 TABLE OF CONTENTS PAGE 1. INTRODUCTION 3 2. METHODOLOGY 3 3. LEVEL OF EVIDENCE AND GRADE OF RECOMMENDATION 3 4. EPIDEMIOLOGY 4 5. ETIOLOGY AND RISK FACTORS 4 6. HISTOPATHOLOGY 5 7. CLASSIFICATION 5 7.1 TNM staging system 5 7.2 Tumour grade 6 8. SURVIVAL 6 8.1 Long-term survival after primary urethral carcinoma 6 8.2 Predictors of survival in primary urethral carcinoma 6 9. DIAGNOSIS AND STAGING 7 9.1 History 7 9.2 Clinical examination 7 9.3 Urinary cytology 7 9.4 Diagnostic urethrocystoscopy and biopsy 7 9.5 Radiological imaging 7 9.6 Regional lymph nodes 7 10. TREATMENT OF LOCALISED PRIMARY URETHRAL CARCINOMA 8 10.1 Treatment of localised primary urethral carcinoma in males 8 10.2 Treatment of localised urethral carcinoma in females 8 10.2.1 Urethrectomy and urethra-sparing surgery 8 10.2.2 Radiotherapy 8 11. MULTIMODAL TREATMENT IN ADVANCED URETHRAL CARCINOMA 9 11.1 Preoperative cisplatinum-based chemotherapy 9 11.2 Preoperative chemoradiotherapy in locally advanced squamous cell carcinoma of the urethra 9 12. TREATMENT OF UROTHELIAL CARCIMONA OF THE PROSTATE 10 13. FOLLOW-UP 10 14. REFERENCES 10 15. ABBREVIATIONS USED IN THE TEXT 15 2 PRIMARY URETHRAL CARCINOMAS - MARCH 2013 1. INTRODUCTION The European Association of Urology (EAU) Guidelines Group on Muscle-invasive and Metastatic Bladder Cancer has prepared these guidelines to deliver current evidence-based information on the diagnosis and treatment of patients with primary urethral carcinoma (UC). -

Summary of Services and Availability (By Location)
UPMC | University of Pittsburgh Medical Center For Reference Only UROLOGY 2013 Summary of Services and Availability (by location) Each location has sufficient space, equipment, staffing and financial resources in place or available in sufficient time as required to support each requested privilege. On an ongoing basis, the organization consistently determines the resources necessary for each requested privilege related to the facility's scope of service. Please review the following Summary of Services and Availability by Location prior to making your selections. If a facility is specifically identified below as NOT having a privilege/service available, you will NOT be considered for that privilege at that individual facility. Any request made that is identified as not available at an individual site will be considered Not Applicable for that site(s), and will be identified as such on your final approved Delineation of Privileges form. “x” means Privilege is Available at that location. “C” means contractual arrangement restricts granting this privilege. “N/A” means Privilege Not Available at that location. Facility Codes: UHOC= UPMC St. Margaret Harmar Outpatient Center Privilege UHOC Core privileges X Consultation Privileges N/A SURGERY OF THE KIDNEY, ADRENAL, URETER, AND BLADDER Biopsy, all techniques X Nephrotomy/pyelotomy/ureterotomy/ cystotomy for X stent placement, stone extraction, drainage abscess, biopsy, fulgeration, insertion of radioactive material Percutaneous nephroscopy, and other percutaneous X catheter techniques Nephrectomy, -

Male Urethral Cancer May Be Primary Or Secondary
Urethral cancer Male urethral cancer May be primary or secondary: primary rare; secondary commonly a/w urothelial carcinoma of the bladder Primary urethral carcinoma usually arises secondary to chronic irritation Urethral stricture Frequent STI/urethritis Presentation haematuria urethral bleeding persistent urethral stricture urethrocutaneous fistula Histology 80% squamous cell carcinoma (a/w HPV 16) 15% transitional cell carcinoma 5% other (adenoCa, melanoma etc.) Location 60% bulbomembranous 30% penile 10% prostatic Generally anterior urethral tumours do better than posterior urethral tumours Spread Anterior urethra – superficial and deep inguinal LNs (unlike penile carcinoma palpable LNs almost always metastatic) Posterior urethra – pelvic LNs Staging (UICC) Tx Tumour cannot be assessed T0 No evidence of primary tumour Tis CIS Ta Papillary, polypoid or verucoid tumour T1 Tumour invades subepithelial connective tissue T2 Tumour invades corpus spongiosum or prostate stroma T3 Corpus cavernosum, vagina or bladder neck T4 Other adjacent structures Nx Nodal disease cannot be assessed N0 No evidence of nodal disease N1 Metastasis to a single LN < 2cm N2 Metastasis to LN 2-5cm, or multiple LNs < 5cm N3 Metastasis to LN > 5cm Mx Distant mets cannot be assessed M0 No distant mets M1 Distant mets Tom Walton January 2011 1 Urethral cancer Management Depends on location and tumour stage: (i) Penile urethra Superficial (<T2) Transurethral resection Local excision and anastomosis Local excision and perineal urostomy Penis tip tumours may be treated -

Cancer in Urinary Tract and Bladder Caiga Du* Vancouver Prostate Centre, Jack Bell Research Centre, Canada
Surgica OPEN ACCESS Freely available online l & l U a r ic o d lo e g y M Medical & Surgical Urology ISSN: 2168-9857 Commentary Cancer in Urinary Tract and Bladder Caiga Du* Vancouver Prostate Centre, Jack Bell Research Centre, Canada Cancer is when cells in the body outgrow control, regularly shaping To understand cancer of the ureter and renal pelvis, it assists with a mass or tumor. In upper urinary tract cancer, unusual cells are realizing how these organs normally work. found in the: • Bladder Cancer: Symptoms and Signs. • Renal pelvis (where urine gathers in the kidneys before it goes • Blood or blood clusters in the urine. to the ureters and bladder) • Pain or burning sensation during urine. • Renal calyces (spaces deep in the kidneys) • Frequent urine. • Ureters (thin tubes, made of muscle, which move urine from the kidney to the bladder) • Feeling the need to urinate many times throughout the night. Cancers of the upper urinary tract are moderately uncommon. The • Feeling the need to urine, not being able to pass urine. most common of all upper urinary tract cancers are those found in • Lower back pain on 1 side of the body. the renal pelvis and renal calyces. Cancer in the ureters makes up about a fourth of all upper urinary tract cancers. Bladder cancer is exceptionally treatable when it is analyzed in the beginning phases. The fundamental sorts of therapies for bladder Tumors of the renal calyces, renal pelvis and ureters start in the cancer include: Surgery: Bladder cancer therapy quite often has layer of tissue that lines the bladder and the upper urinary ptract, a careful part that might be joined with other non-obtrusive called the urothelium. -

Dataset for Tumours of the Urinary Collecting System (Renal Pelvis, Ureter
Dataset for histopathological reporting of tumours of the urinary collecting system (renal pelvis, ureter, urinary bladder and urethra) August 2021 Authors: Dr Murali Varma, University Hospital of Wales, Cardiff Dr Jonathan H Shanks, The Christie NHS Foundation Trust, Manchester Dr Ashish Chandra, Guys and St Thomas’ NHS Foundation Trust, London Dr Lorna McWilliam, Central Manchester University Hospitals NHS Foundation Trust Unique document number G044 Document name Dataset for tumours of the urinary collecting system (renal pelvis, ureter, urinary bladder and urethra) Version number 3 Produced by Each of the authors is a consultant histopathologist with a special interest in urological pathology. Dr Murali Varma is a founder member and Chairman of the British Association of Urological Pathologists (BAUP), organises biannual uropathology courses on prostate and bladder pathology, and has published several original and review papers related to urological pathology. Dr Jonathan H Shanks regularly speaks at national and international meetings and has co- authored over 95 publications, mostly in the field of urological pathology. Dr Ashish Chandra is co-author of ACP Best Practice: Cut up and reporting of bladder cancer specimens and is on the NICE Clinical Guidelines Group for diagnosis and clinical management of bladder cancer. Dr Lorna McWilliam is a founder member of BAUP and speaks on bladder and prostate pathology at their biannual courses. She helped to develop national and regional guidelines for best practice in urological pathology. Date active August 2021 (to be implemented within three months) Date for review August 2024 Comments This document will replace the 2nd edition published in 2013. In accordance with the College’s pre-publications policy, this document was on the Royal College of Pathologists’ website for consultation from 27 May to 24 June 2021. -
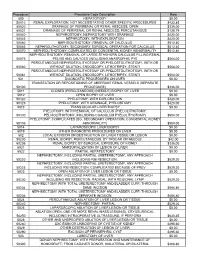
Procedure Procedure Code Description Rate 500
Procedure Procedure Code Description Rate 500 HEPATOTOMY $0.00 50010 RENAL EXPLORATION, NOT NECESSITATING OTHER SPECIFIC PROCEDURES $433.85 50020 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; OPEN $336.00 50021 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; PERCUTANIOUS $128.79 50040 NEPHROSTOMY, NEPHROTOMY WITH DRAINAGE $420.00 50045 NEPHROTOMY, WITH EXPLORATION $420.00 50060 NEPHROLITHOTOMY; REMOVAL OF CALCULUS $512.40 50065 NEPHROLITHOTOMY; SECONDARY SURGICAL OPERATION FOR CALCULUS $512.40 50070 NEPHROLITHOTOMY; COMPLICATED BY CONGENITAL KIDNEY ABNORMALITY $512.40 NEPHROLITHOTOMY; REMOVAL OF LARGE STAGHORN CALCULUS FILLING RENAL 50075 PELVIS AND CALYCES (INCLUDING ANATROPHIC PYE $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50080 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50081 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 501 DIAGNOSTIC PROCEDURES ON LIVER $0.00 TRANSECTION OR REPOSITIONING OF ABERRANT RENAL VESSELS (SEPARATE 50100 PROCEDURE) $336.00 5011 CLOSED (PERCUTANEOUS) (NEEDLE) BIOPSY OF LIVER $0.00 5012 OPEN BIOPSY OF LIVER $0.00 50120 PYELOTOMY; WITH EXPLORATION $420.00 50125 PYELOTOMY; WITH DRAINAGE, PYELOSTOMY $420.00 5013 TRANSJUGULAR LIVER BIOPSY $0.00 PYELOTOMY; WITH REMOVAL OF CALCULUS (PYELOLITHOTOMY, 50130 PELVIOLITHOTOMY, INCLUDING COAGULUM PYELOLITHOTOMY) $504.00 PYELOTOMY; COMPLICATED (EG, SECONDARY OPERATION, CONGENITAL KIDNEY 50135 ABNORMALITY) $504.00 5014 LAPAROSCOPIC LIVER BIOPSY $0.00 5019 OTHER DIAGNOSTIC PROCEDURES -

Urethral Carcinoma Recurrence in Ileal Orthotopic Neobladder: Urethrectomy and Conversion in a Continent Pouch with Abdominal Stoma
Case Report Urol Int 1999;62:213–216 Received: June 19, 1998 Accepted after revision: March 8, 1999 Urethral Carcinoma Recurrence in Ileal Orthotopic Neobladder: Urethrectomy and Conversion in a Continent Pouch with Abdominal Stoma Riccardo Bartoletti a Alessandro Natali a Mauro Gacci a Michelangelo Rizzoa Cesare Selli b Departments of Urology, aUniversity of Florence, and bUniversity of Udine, Italy Key Words incidence of complications such as nighttime inconti- Bladder carcinoma W Ileal neobladder W Urethral nence, high postvoid volume, urinary infections, lithiasis, carcinoma recurrence or long-term augmentation of reservoir capacity [1]. Ure- thral carcinoma recurrences are reported in about 5% of the patients treated with orthotopic urinary diversion and Abstract are often due to an inadequate preoperative evaluation of A patient who had previously undergone ileal neoblad- disease and localization of bladder carcinoma at the blad- der with Studer technique presented an urethral recur- der neck [2]. rence of a transitional cell carcinoma. Further surgical treatment consisted of urethrectomy and creation of an intussuscepted ileal loop which was anastomosed to the Case Report pouch and provided a continence mechanism allowing A 68-year-old male patient, who originally presented a T N M self-catheterization. 2 0 0 (G2) bladder tumor and underwent 12 months earlier orthotopic Copyright © 1999 S. Karger AG, Basel ileal neobladder diversion according to Studer, was admitted to our institution with hematuria. A cystourethrogram showed an urethral lesion (fig. 1a). Com- Introduction puted tomography and magnetic resonance imaging confirmed the presence of a solid lesion measuring about 3 ! 2 cm, infiltrating the corpus spongiosum (fig.