Agenda 23 December 2020 WSCCG PCCC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Grass Cutting 2021 Target Dates (SCC Website).Xlsx
Grassing cutting programme 2021 SUFFOLK C&U CUT TARGET DATES Parish: Target date (week commencing) Blythburgh 24 May 2021 Bramfield 24 May 2021 Bungay 24 May 2021 Chediston 24 May 2021 Cookley 24 May 2021 Cratfield 24 May 2021 Dunwich 24 May 2021 Ellough 24 May 2021 Flixton 24 May 2021 Heveningham 24 May 2021 Homersfield 24 May 2021 Hoo 24 May 2021 Huntingfield 24 May 2021 Ilketshall St John 24 May 2021 Ilketshall St Andrew 24 May 2021 Ilketshall St Lawrence 24 May 2021 Ilketshall St Margaret 24 May 2021 Linstead Magna 24 May 2021 Linstead Parva 24 May 2021 South Elmham St Cross 24 May 2021 South Elmham St James 24 May 2021 South Elmham St Margaret 24 May 2021 South Elmham St Mary 24 May 2021 South Elmham St Michael 24 May 2021 South Elmham St Nicholas 24 May 2021 South Elmham St Peter 24 May 2021 Thorington 24 May 2021 Ubbeston 24 May 2021 Walberswick 24 May 2021 Walpole 24 May 2021 Wenhaston with Mells Hamlet 24 May 2021 Barking 24 May 2021 Barnham 24 May 2021 Barningham 24 May 2021 Battisford 24 May 2021 Beck Row 24 May 2021 Belstead 24 May 2021 Bramford 24 May 2021 Brandon 24 May 2021 Brantham 24 May 2021 Buxhall 24 May 2021 Chelmondiston 24 May 2021 Combs 24 May 2021 Coney Weston 24 May 2021 East Bergholt 24 May 2021 Elveden 24 May 2021 Eriswell 24 May 2021 Erwarton 24 May 2021 Euston 24 May 2021 Fakenham Magna 24 May 2021 Flowton 24 May 2021 Freston 24 May 2021 Great Blakenham 24 May 2021 Great Bricett 24 May 2021 Great Finborough 24 May 2021 Harkstead 24 May 2021 Harleston 24 May 2021 Holbrook 24 May 2021 Honington 24 May 2021 Hopton -

Wratting Croft, Haverhill Road, Little Wratting, Suffolk
WRATTING CROFT, HAVERHILL ROAD, LITTLE WRATTING, SUFFOLK An opportunity WRATTING to acquire CROFT, a building HAVERHILL plot with planning ROAD, permission LITTLE for 10 properties WRATTING on the ,outskirts SUFFOLK of Haverhill. The site comprises of 8 x 3 bedroom terraced cottages and 2 detached 4 bedroom homes all with parking and generous gardens. Guide £1,100,000 Wratting Croft, Haverhill Road, Little Wratting, Haverhill, Suffolk, CB9 7UD 1 – 1,340 sq.ft Detached House 1 – 1,296 sq.ft Detached House 3 - 933 sq.ft 3 Bedroom Terraced Houses 4 - 890 sq.ft 3 Bedroom Terraced Houses Location Little Wratting is situated approximately 1 mile from the popular village of Kedington, which has a number of facilities including shops, pubs and a school. Kedington is located approximately 4 miles to the west of Clare and has easy access to Cambridge (20 miles), Stansted Airport (20 miles) and Bury St Edmunds (17 miles). Further amenities including supermarkets, shops, restaurants and cinema are available locally in Haverhill. Viewing strictly by appointment with David Burr. Additional information Clare 01787 277811 Services: Available Castle Hedingham (01787) 463404 None of the services have been tested by the agent. Leavenheath (01206) 263007 Long Melford (01787) 883144 Local authority: West Suffolk Council. Newmarket (01638) 669035 Woolpit (01359) 245245 Bury St Edmunds (01284) 725525 Linton & Villages (01440) 784346 NOTICE. Whilst every effort has been made to ensure the accuracy of these sales London (020) 78390888 details, they are for guidance purposes only and prospective purchasers or lessees are advised to seek their own professional advice as well as to satisfy themselves by DAVIDBURR.CO.UK inspection or otherwise as to their correctness. -

Wratting Croft Haverhill Road, Little Wratting, Suffolk
Wratting Croft Haverhill Road, Little Wratting, Suffolk Wratting Croft, Haverhill Road, Little Wratting, Suffolk CB9 7UD Little Wratting is situated approximately 1 mile from the popular village of Kedington, which has a number of facilities including shops, pubs and a school. Kedington is located approximately 4 miles to the west of Clare and has easy access to Cambridge (20 miles), Stansted Airport (20 miles) and Bury St Edmun ds (17 miles). Further amenities including supermarkets, shops, restaurants and cinema are available locally in Haverhill. This substantial 4,000 sq.ft detached Edwardian residence sits in a prominent location convenient for local amenities. The property has recently undergone an extensive refurbishment programme blending original period features with modern finishes including a stunning open plan kitchen/breakfast room and luxurious bathrooms, all set within mature gardens with ample parking. In all about 0.33 of an acre. An exceptional detached home situated in a prominent location having recently been refurbished to a high specification. Entrance porch into the: RECEPTION HALL A spacious and welcoming hallway with double DINING ROOM Also featuring an attractive fireplace with wooden mantel cloaks cupboard, chequered tiled floor, painted oak panelling and impressive and cupboard to the side and outlook over the rear garden. turning staircase rising to the first floor. UTILITY Fitted with units under worktops with a stainless steel sink and DRAWING ROOM A charming triple aspect room featuring a tiled drainer and plumbing for a washing machine. fireplace with a wooden surround, parquet flooring and French doors leading to the: CLOAKROOM WC and wash basin and heated towel rail. -

Records Relating to 1914-1918 War-Part 1
Records Relating to 1914-1918 War-part 1 This leaflet is the first draft pulling together references to sources held by Suffolk Record Office relating to the 1914-1918 War. It will be added to throughout the commemoration period as new material is deposited or comes to light as a result of research. If you have references to any Suffolk Record Office WW1 material which is not included in the leaflet, please send the details to Collections Manager Bridget Hanley ([email protected]) so they can be added. The Record Office holds a considerable amount of material illustrating various aspects of the war as it affected Suffolk people, whether they were combatants or those on the ‘Home Front’. Such was its effect on society that, in a sense, any records created between August 1914 and November 1918 – and beyond – could throw light, direct or indirect, on the First World War. The records of institutions contain in their pages a considerable amount of essential background information, and help in understanding other documents that were created as a result of, or relate specifically to, the War. The authorities administering the county, the two County Councils, the Boroughs and District Councils and Parish Councils – all reveal the effects of war on the running of local government through their minute books and committee minutes. Similarly school log books, petty sessions, court register and Anglican register of services all show a variety of different responses to the stresses imposed on society by total war. Log books record enforced changes in routine and the way children were drawn into the war effort; court registers reveal a variety of novel offences created by the war, while registers of services can suggest to what extent people turned to organised religion in a time of crisis. -

SEBC Planning Decisions 44/17
ST EDMUNDSBURY BOROUGH COUNCIL PLANNING AND GROWTH DECISIONS WEEK ENDING 27/10/2017 PLEASE NOTE THE DECISIONS LIST RUN FROM MONDAY TO FRIDAY EACH WEEK DC/17/1724/HH Householder Planning Application - Cleveland DECISION: Extension to garage The Green Approve Application Bardwell DECISION TYPE: APPLICANT: Mr Barry Heywood Bury St Edmunds Delegation Panel AGENT: Mr John Brand Suffolk ISSUED DATED: IP31 1AW 26 Oct 2017 WARD: Bardwell PARISH: Bardwell DC/16/2511/FUL Planning Application - conversion of first First And Second Floors DECISION: and second floor retail space in to 4no. one 30-32 St Johns Street Approve Application bedroom flats, and 1no. 2 Bedroom flat as Bury St Edmunds DECISION TYPE: amended by the plans received IP33 1SN Delegated 29/08/2017 ISSUED DATED: 27 Oct 2017 APPLICANT: Mr Peter Hays WARD: Risbygate AGENT: Ski Property Management - Mr PARISH: Bury St Kazimierz Swierdzewski Edmunds Town Council (EMAIL) DC/17/1622/FUL Planning Application - (i) Change of use 79 Whiting Street DECISION: from residential building (C3) to offices Bury St Edmunds Approve Application (B1A), and (ii) removal of garage lintel and IP33 1NX DECISION TYPE: replace with full height gates and; (iii) 1no. Delegated Pear tree - canopy to be lifted to clear ISSUED DATED: height of 3 metres. 25 Oct 2017 WARD: Abbeygate APPLICANT: Mr James Mellish PARISH: Bury St AGENT: Mr Mark Cleveland - Whitworth Edmunds Town Council (EMAIL) DC/17/1623/LB Application for Listed Building Consent - 79 Whiting Street DECISION: removal of garage lintel and replace with -

Option a - Rural Wards
Option A - Rural wards Key Key Two-member ward Within 10% of the ideal electorate of 2056 Variance against ideal electorate of more than 10% % Away from No. of Total Average Ward No. Proposed name of ward members electorate (Variance) Parishes Changes made as a result of consultation Details of feedback received and other comments Other options that could be considered See comment against Kedington ward below. Barnadiston, Cowlinge, Great and Little Bradley, Great and Little 1 Withersfield ward 1 1950 -5.16% None In January 2018 the councils undertook a community links consultation to inform the See Options A1 and A2 for alternative options Thurlow, Withersfield and Great and Little Wratting warding review. Withersfield Parish Council responded to confirm their natural link to the Great and Little Thurlow parishes 2 Hundon & Wickhambrook ward 1 2247 9.29% Hundon, Stradishall & Wickhambrook None See comment against Kedington ward below See Options A1 and A2 for alternative options In March 2018 the councils undertook a consultation on the draft ward options and feedback was received from Poslingford Parish Council regarding being a small parish in 3 Clare ward 1 1992 -3.11% Clare and Poslingford None this ward with Clare. Unfortunately Clare is too large to be combined with a neighbouring parish and is too small to be a standalone ward. Further evidence would be required to be able to demonstrate the case for a substantially larger than threshold ward. Cavendish, Brockley, Denston, Hawkedon, Rede, Stansfield & 4 Cavendish ward 1 1989 -3.26% None Support from Hawkedon Parish Council received during the March 2018 consultation Whepstead In March 2018 the councils undertook a consultation on the draft ward options and feedback was received from Stoke by Clare Parish Council and Wixoe Parish Meeting regarding their local connections with Hundon parish and not with the Kedington parish. -

1. Parish : Little Wratting
1. Parish : Little Wratting Meaning: Place where crosswort grew 2. Hundred: Risbridge Deanery: Clare Union: Risbridge RDC/UDC: (W. Suffolk) Clare RD (−1974), St. Edmundsbury DC (1974−) Other administrative details: Civil boundary change 1883 Ecclesiastical boundary change 1819 to create Great Wratting with Little Wratting Risbridge Petty Sessional Division Haverhill County Court District 3. Area: 936 acres (1912) 4. Soils: Mixed: a. Slowly permeable calcareous/non calcareous clay soils, slight risk water erosion b. Deep well drained fine loam, coarse loam and sandy soils, locally flinty and in places over gravel. Slight risk water erosion 5. Types of farming: 1086 Wratting: 23 acres meadow, 2 oxen, 2 mills, 5 cobs, 23 cattle, 106 pigs, 800 sheep, 40 goats, wood for 8 pigs, 6 beehives 1500–1640 Thirsk: Wood-pasture region, mainly pasture, meadow, engaged in rearing and dairying with some pig keeping, horse breeding and poultry. Crops mainly barley with some wheat, rye, oats, peas, vetches, hops and occasionally hemp. Also has similarities with sheep-corn region where sheep are main fertilising agent, bred for fattening, barley main cash crop. 1818 Marshall: Wide variations of crop and management techniques including summer fallow in preparation for corn and rotation of turnip, barley, clover, wheat on lighter lands 1937 Main crops: Wheat, barley, beans, peas, roots 1 1969 Trist: More intensive cereal growing and sugar beet. 6. Enclosure: 7. Settlement: 1960 Small parish with no recognisable centre of development. Church situated in NE sector near small number of dwellings. Scattered farms. Inhabited houses: 1674 – 8, 1801 – 12, 1851 – 42, 1871 – 46, 1901 – 36, 1951 – 55, 1981 – 57 8. -

Parish Share 2021
Parish Share 2021 Deanery Summary: 28 February 2021 29th February Deanery Received 2020 Received Clare £ 9,574 £ 14,582 Gipping Valley £ 67,109 £ 95,058 Hadleigh £ 13,409 £ 31,772 Ixworth £ 13,388 £ 16,755 Lavenham £ 42,024 £ 38,734 Mildenhall £ 16,483 £ 19,781 Sudbury £ 39,197 £ 32,414 Thingoe £ 79,127 £ 77,186 Sudbury Archdeaconry £ 280,311 £ 326,282 Colneys £ 54,479 £ 66,254 Hartismere £ 15,289 £ 21,384 Hoxne £ 9,110 £ 15,569 Loes £ 21,994 £ 42,071 Samford £ 15,972 £ 16,199 Saxmundham £ 35,181 £ 48,089 Waveney & Blyth £ 46,260 £ 52,586 Woodbridge £ 44,720 £ 62,613 Suffolk Archdeaconry £ 243,005 £ 324,766 Ipswich £ 76,329 £ 63,850 Ipswich Archdeaconry £ 76,329 £ 63,850 Other Donations £ 490 £ - February 2021 /2020 £ 600,135 £ 714,897 05/05/2021 P:\Accounts General\Parish Share\2021\Reports\Share Report-Funds Received as at 28th February 2021 Parish Share 2021 Clare Deanery: 2021 Parish/Benefice Received Haverhill £ - Withersfield £ - Waiver agreed by Finance Committee Haverhill with Withersfield Total £ - Barnardiston £ - Great Bradley £ - Great Thurlow £ - Great Wratting £ - Kedington £ - Little Bradley £ - Little Thurlow £ - Little Wratting £ - Under-allocation £ - Stourhead Benefice Total £ - Cowlinge £ - Denston £ - Lidgate £ - Ousden £ 1,000 Stansfield £ - Stradishall £ - Wickhambrook £ 800 To be allocated The Benefice of Bansfield Total £ 1,800 Chedburgh £ - Chevington £ 2,536 Depden £ - Hargrave £ 500 Hawkedon £ 1,238 Rede £ - The Benefice of Suffolk Heights Total £ 4,274 Cavendish £ - Clare with Poslingford £ 3,500 Hundon £ -

SLHC LOCAL RECORDERS SCHEME PARISHES Without Local Recorder
SLHC LOCAL RECORDERS SCHEME PARISHES without Local Recorder Updated: January 2016 Please contact [email protected] if you are interested in finding out how to become the Local Recorder for any of the parishes below: ACTON BRAMPTON CRATFIELD AKENHAM BRANDESTON CREETING ST MARY FRESTON ALDEBURGH BRANTHAM CREETING ST PETER GAZELEY ALDERTON BRETTENHAM DALHAM GEDDING ALDHAM BRIGHTWELL DALLINGHOO GOSBECK ALDRINGHAM BROCKLEY DARMSDEN GREAT BARTON ALPHETON BRUISYARD DENHAM (Eye) GREAT BRADLEY ASSINGTON BUCKLESHAM DENSTON GREAT BRICETT BARHAM BURES ST MARY DEPDEN GREAT CORNARD BARKING BURGATE DRINKSTONE GREAT WALDINGFIELD BARNARDISTON BUTLEY EASTON GREAT WELNETHAM GREAT WENHAM BARNBY CAPEL ST ANDREW ELMSETT GREAT WRATTING BARNHAM CAPEL ST MARY ELVEDEN HARDWICK BARNINGHAM CARLTON COLVILLE ERWARTON HAWKEDON BARROW CAVENHAM FARNHAM & STRATFORD ST. ANDREW HELMINGHAM BARSHAM CHARSFIELD FELIXSTOWE HEMLEY BECCLES CHEVINGTON FELSHAM HENGRAVE BEDFIELD CHEDBURGH FINNINGHAM HEPWORTH BENACRE CHELSWORTH FLEMPTON HERRINGSWELL BILDESTON CHILTON FLIXTON (Bungay) HEVENINGHAM BLYFORD CLAYDON with WHITTON RURAL FLOWTON HOLBROOK BOULGE COTTON FORNHAM ALL SAINTS HOLTON ST PETER BRADFIELD ST GEORGE COWLINGE FOXHALL HONINGTON HOO LITTLE FINBOROUGH RUSHBROOKE with ROUGHAM TROSTON HORRINGER LITTLE GLEMHAM RUMBURGH UFFORD HUNDON LITTLE WENHAM RUSHMERE (near Lowestoft) WANGFORD (near Thetford) ICKLINGHAM LITTLE WRATTING SANTON DOWNHAM WATTISFIELD ICKWORTH LOWESTOFT (North) SAPISTON WATTISHAM IKEN LOWESTOFT (South) SEMER WENHASTON ILKETSHALL ST JOHN MARKET WESTON SHADINGFIELD -
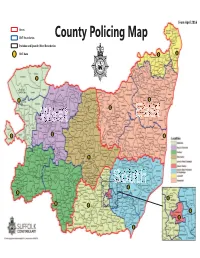
County Policing Map
From April 2016 Areas Somerleyton, Ashby and Herringfleet SNT Boundaries County Policing Map Parishes and Ipswich Ward Boundaries SNT Base 17 18 North Cove Shipmeadow Ilketshall St. John Ilketshall St. Andrew Ilketshall St. Lawrence St. Mary, St. Margaret South Ilketshall Elmham, Henstead with Willingham St. May Hulver Street St. Margaret, South Elmham St. Peter, South ElmhamSt. Michael, South Elmham HomersfieldSt. Cross, South Elmham All Saints and 2 St. Nicholas, South Elmham St. James, South Elmham Beck Row, Holywell Row and Kenny Hill Linstead Parva Linstead Magna Thelnetham 14 1 Wenhaston with Mildenhall Mells Hamlet Southwold Rickinghall Superior 16 Rickinghall Inferior Thornham Little Parva LivermLivermore Ixworthxwo ThorpeThorp Thornham Magna Athelington St.S GenevieveFornhamest Rishangles Fornham All Saints Kentford 4 3 15 Wetheringsett cum Brockford Old Newton Ashfield cum with Thorpe Dagworth Stonham Parva Stratford Aldringham Whelnetham St. Andrew Little cum Thorpe Brandeston Whelnetham Great Creeting St. Peter Chedburgh Gedding Great West Monewden Finborough 7 Creeting Bradfield Combust with Stanningfield Needham Market Thorpe Morieux Brettenham Little Bradley Somerton Hawkedon Preston Kettlebaston St. Mary Great Blakenham Barnardiston Little BromeswellBrome Blakenham ut Sutton Heath Little Little 12 Wratting Bealings 6 Flowton Waldringfield Great 9 Waldingfield 5 Rushmere St. Andrew 8 Chattisham Village Wenham Magna 11 Stratton Hall 10 Rushmere St. Andrew Town Stratford Trimley St. Mary St. Mary 13 Erwarton Clare Needham Market Sproughton Melton South Cove Bedingfi eld Safer Neighbourhood Cowlinge Nettlestead Stoke-by-Nayland Orford Southwold Braiseworth Denston Norton Stratford St. Mary Otley Spexhall Brome and Oakley Teams and parishes Depden Offton Stutton Pettistree St. Andrew, Ilketshall Brundish Great Bradley Old Newton with Tattingstone Playford St. -

Roll of Honour – Parishes
Parish Surname First name Honours Rank Major unit Sub unit Notes Lackford Foreman Cecil NULL Sergeant East Surrey Regt NULL NULL Lackford Harding Herbert NULL Lance/Corporal Royal Fusiliers NULL NULL Lackford Kidd William NULL Private Suffolk Regt NULL NULL Lackford Meekins Frederick NULL Private Suffolk Regt NULL NULL Lackford Sharpe Richard NULL Driver Army Service Corps NULL NULL Lakenheath Allsop Robert NULL Private Essex Regt NULL NULL Lakenheath Allsop William Henry NULL Gunner Royal Garrison Artillery NULL NULL Lakenheath Ashman Donald NULL Private Suffolk Regt 11th Batt NULL Lakenheath Bailey Alec NULL Private Suffolk Regt 11th Batt NULL Lakenheath Bailey Arthur NULL Corporal Devonshire Regt 12th Batt NULL Lakenheath Bilsland James NULL Private Canadian Expeditionary Force 4th Batt NULL Lakenheath Brooks Claud DCM Sergeant King's Shropshire Light Infantry NULL NULL Lakenheath Brooks George R NULL Private Essex Regt NULL NULL Lakenheath Brown Harry NULL Private Suffolk Regt 1st Batt NULL Lakenheath Bullen Forester W NULL Private Northumberland Fusiliers 11th Batt NULL Lakenheath Carpenter Arthur NULL Private Suffolk Regt 11th Batt NULL Lakenheath Coleman Arthur NULL Private Suffolk Regt 3rd Batt NULL Lakenheath Coleman George Taff NULL Private Bedfordshire Regt 1st Batt NULL Lakenheath Coleman Sargent NULL Private Northamptonshire Regt NULL NULL Lakenheath Coleman Sydney NULL Rifleman '8th Rifles' NULL NULL Lakenheath Cooper John W NULL Private East Surrey Regt 8th Batt NULL Lakenheath Dicks John H NULL Private Queen's Own Royal -

Villages and Parishes Catchment Area List 2022 2023
Villages and Parishes Catchment Area List for the 2022/2023 school year only Your catchment area school may not be your nearest suitable school. School travel eligibility is based on a child attending their nearest suitable school that would have had a place available for them. This means that your child might not be eligible for Suffolk County Council funded school travel to your catchment area school. We strongly recommend that you check which school is your nearest suitable school on our Nearest School Checker because this might not be your catchment area school. You can find out which are your three nearest Suffolk schools (based on the statutory walking distance including Public Rights of Way) by putting your postcode into our nearestschool.suffolk.gov.uk. We update this each year to include new roads and developments. Suffolk County Council (SCC) Funded School Travel Please be aware: You must consider how your child will travel to and from school before you apply for a school place. Further information on how to apply for a school place can be found on the relevant page at www.suffolk.gov.uk/admissions. Full details about SCC funded school travel, including the School Travel Policy, additional arrangements for low income families and those with Special Educational Needs and Disabilities (SEND), can be found at www.suffolkonboard.com/schooltravel. Catchment area list The information given in this list should be used as a guide only and may change. It is correct at the time of publication (31/08/21). For up-to-date information about a particular address, please contact the Admissions Team on 0345 600 0981.