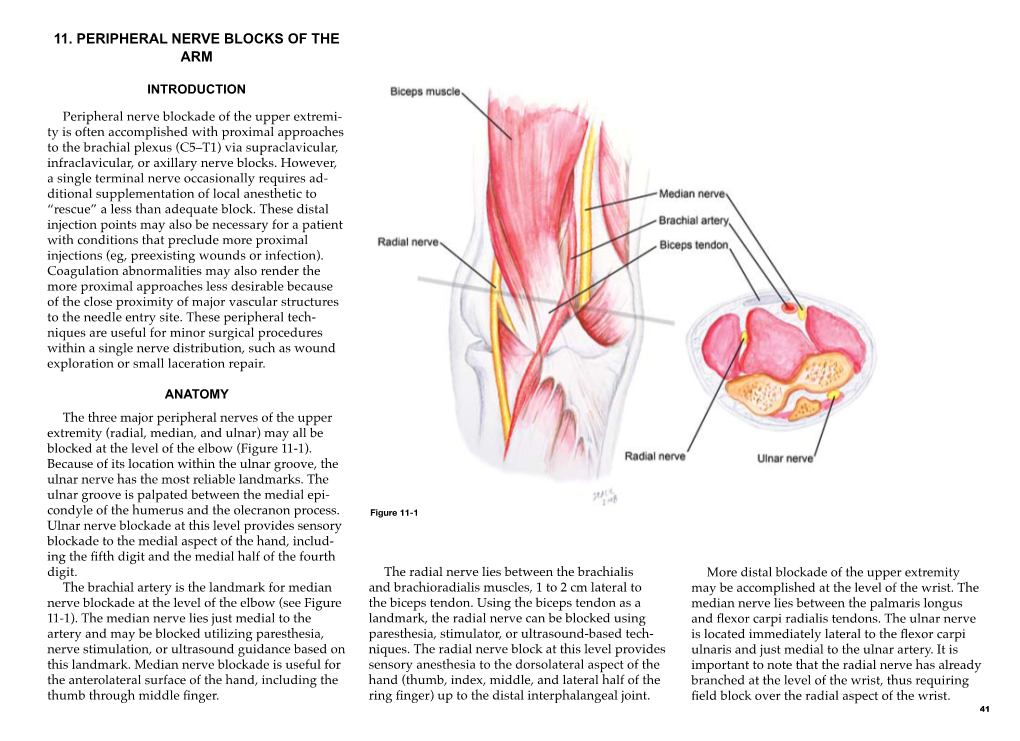
11. Peripheral Nerve Blocks of the Arm
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Considered a Bone of Both Shoulder Girdle and Shoulder Joint. the Shoulder Girdle Is Comprised of the Clavicle and the Scapula
Considered a bone of both shoulder girdle and shoulder joint. The shoulder girdle is comprised of the clavicle and the scapula. The shoulder joint consists of the scapula and the humerus. The primary function of the shoulder girdle is to position itself to accommodate movements of the shoulder joint. 1 Superior angle—top point Inferior angle—bottom point Vertebral border—side closest to vertebral column Axillary border—side closest to arm Subscapular fossa—anterior fossa Glenoid fossa, glenoid labrum, glenoid cavity --The glenoid fossa is the shallow cavity where the humeral head goes. The glenoid labrum is the cartilage that goes around the glenoid fossa. So the glenoid fossa and glenoid labrum together comprise the glenoid cavity. Supraspinous fossa—posterior, fossa above the spine Spine of the scapula—the back projection Infraspinous fossa—posterior depression/fossa below spine Coracoid process—anterior projection head Acromion process—posterior projection head above spine 2 Scapulothoracic “joint” = NOT a true joint; there are no ligaments or articular capsule. The scapula just rests on the muscle over top the rib cage, which allows for passive movements. Sternoclavicular joint=where the clavicle (collarbone) and the sternum (breastbone) articulate; movement is slight in all directions and of a gliding, rotational type Acromioclavicular joint = where the clavicle and scapula (acromion process) articulate; AKA: AC Joint; movement is a slight gliding when elevation and depression take place. Glenohumeral joint = the shoulder joint 3 4 All 3 true joints: Sternoclavicular, AC and glenohumeral (GH) all work together to move arm in all directions. The GH allows the arm to go out to the side and be abducted, then the AC and Sternoclavicular joints kick in to allow the arm to go above shoulder level by allowing the shoulderblade to move up to increase the range of motion (ROM). -

Wrist Fracture – Advice Following Removal of Your Cast
Wrist Fracture – advice following removal of your cast A plaster cast usually prevents a fracture from moving, but allows your fingers to move. The cast also reduces pain. What to expect It usually takes four to six weeks for new bone to form to heal your fracture. When the cast is removed most people find that their wrist is stiff, weak and uncomfortable to start with. It may also be prone to swelling and the skin dry or flaky, this is quite normal. It is normal to get some pain after your fracture. If you need painkillers you should take them as prescribed as this will allow you to do your exercises and use your wrist for light activities. You can ask a Pharmacist about over the counter painkillers. If your pain is severe, continuous or excessive you should contact your GP. The new bone gradually matures and becomes stronger over the next few months. It is likely to be tender and may hurt if you bang it. The muscles will be weak initially, but they should gradually build up as you start to use your hand and wrist. When can I start to use my hand and wrist? It is important to try and use your hand and wrist as normally as possible. Start with light activities like fastening buttons, washing your face, eating, turning the pages of books over etc. Build up as pain allows. Avoid lifting a kettle for 4 weeks If I have been given a Wrist splint You may have been given a wrist splint to wear. -

Anatomical Variations of the Brachial Plexus Terminal Branches in Ethiopian Cadavers
ORIGINAL COMMUNICATION Anatomy Journal of Africa. 2017. Vol 6 (1): 896 – 905. ANATOMICAL VARIATIONS OF THE BRACHIAL PLEXUS TERMINAL BRANCHES IN ETHIOPIAN CADAVERS Edengenet Guday Demis*, Asegedeche Bekele* Corresponding Author: Edengenet Guday Demis, 196, University of Gondar, Gondar, Ethiopia. Email: [email protected] ABSTRACT Anatomical variations are clinically significant, but many are inadequately described or quantified. Variations in anatomy of the brachial plexus are important to surgeons and anesthesiologists performing surgical procedures in the neck, axilla and upper limb regions. It is also important for radiologists who interpret plain and computerized imaging and anatomists to teach anatomy. This study aimed to describe the anatomical variations of the terminal branches of brachial plexus on 20 Ethiopian cadavers. The cadavers were examined bilaterally for the terminal branches of brachial plexus. From the 40 sides studied for the terminal branches of the brachial plexus; 28 sides were found without variation, 10 sides were found with median nerve variation, 2 sides were found with musculocutaneous nerve variation and 2 sides were found with axillary nerve variation. We conclude that variation in the median nerve was more common than variations in other terminal branches. Key words: INTRODUCTION The brachial plexus is usually formed by the may occur (Moore and Dalley, 1992, Standring fusion of the anterior primary rami of the C5-8 et al., 2005). and T1 spinal nerves. It supplies the muscles of the back and the upper limb. The C5 and C6 fuse Most nerves in the upper limb arise from the to form the upper trunk, the C7 continues as the brachial plexus; it begins in the neck and extends middle trunk and the C8 and T1 join to form the into the axilla. -

Wrist Fracture
Hand Conditions: WRIST FRACTURE A wrist fracture is a break in one or more of the bones in the wrist. The wrist is made up of the two bones in the forearm called the radius and the ulna. It also includes eight carpal bones. The carpal bones lie between the end of the forearm bones and the bases of the fi ngers. The most commonly fractured carpal bone is called the scaphoid or navicular bone. This fact sheet will focus on fractures of the carpal bones of the wrist. Causes A wrist fracture is caused by trauma to the bones in the wrist. Trauma may be caused by: • Falling on an outstretched arm • Direct blow to the wrist • Severe twist of the wrist Risk Factors Factors that increase your chance of developing a wrist fracture include: • Participating in contact sports, such as football or soccer • Participating in activities such as in-line skating, skateboarding, or bike riding • Participating in any activity which could cause you to fall on your outstretched hand • Violence or high-velocity trauma, such as an automobile accident Symptoms If you have any of these symptoms, do not assume they are due to a wrist fracture. Symptoms of a wrist fracture include. • Pain • Swelling and tenderness around the wrist • Bruising around the wrist • Limited range of wrist or thumb motion • Visible deformity in the wrist For more information visit us online at www.ptandme.com Hand Conditions: WRIST FRACTURE Diagnosis Your doctor will ask about your symptoms, physical activity, and how the injury occurred. The injured area will be examined. -

Anastomotic Branch from the Median Nerve to the Musculocutaneous Nerve: a Case Report
Case Report www.anatomy.org.tr Recieved: February 10, 2008; Accepted: April 22, 2008; Published online: October 31, 2008 doi:10.2399/ana.08.063 Anastomotic branch from the median nerve to the musculocutaneous nerve: a case report Feray Güleç Uyaro¤lu1, Gülgün Kayal›o¤lu2, Mete Ertürk2 1Department of Neurology, Ege University Faculty of Medicine, Izmir, Turkey 2Department of Anatomy, Ege University Faculty of Medicine, Izmir, Turkey Abstract Anomalies of the brachial plexus and its terminal branches are not uncommon. Communicating branch arising from the mus- culocutaneous nerve to the median nerve is a frequent variation, whereas the presence of an anastomotic branch arising from the median nerve and joining the musculocutaneous nerve is very rare. During routine dissection of cadaver upper limbs, we observed an anastomotic branch arising from the median nerve running distally to join with the branches of the musculocutaneous nerve in a left upper extremity. The anastomotic branch originated from the median nerve 11.23 cm prox- imal to the interepicondylar line. After running distally and coursing between the biceps brachii and the brachialis muscles, this anastomotic branch communicated with two branches of the musculocutaneous nerve separately. The presence of the communicating branches between these nerves should be considered during surgical interventions and clinical investigations of the arm. Key words: anatomy; brachial plexus; communicating branch; upper limb; variation Anatomy 2008; 2: 63-66, © 2008 TSACA Introduction neous nerve (C5, C6, and C7) connects with the median nerve in the arm.2,3 The musculocutaneous nerve is the Variations of the brachial plexus and its terminal continuation of the lateral cord of the brachial plexus. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

PE1897 Wrist and Hand Stretches
Patient and Family Education Wrist and Hand Stretches How can I help my child do the stretches? Use these exercises to help stretch the You play an important role in your child’s therapy. Older children may need wrist and hand. reminders to do their stretches every day. You may need to help position your younger child for the stretches. Or you may need to help stretch your child’s hand or arm. Be sure to pay attention to your child’s alignment and posture to make sure each stretch is performed correctly. How often should my child do the stretches? These stretches should be done twice a day, or as instructed by your therapist: ______________________________________________________________ Stretches Wrist extension Hold arm out in front Use opposite hand to bend wrist up with fingers straight Option to straighten elbow for increased stretch Hold for 30 seconds or _______ Repeat 2 times or ___________ VHI Wrist extension Sit with elbows on table Place palms together Slowly lower wrists to table Hold for 30 seconds or ______ Repeat 2 times or __________ VHI Wrist flexion Hold arm out in front Use opposite hand to bend wrist down Option to straighten elbow for increased stretch Option to curl fingers for increased stretch Hold for 30 seconds or ______ VHI Repeat 2 times or __________ 1 of 2 Wrist and Hand Stretches Wrist radial/ulnar deviation To Learn More Hold arm at side of body with palm • Occupational/Physical facing forward Therapy 206-987-2113 Use opposite hand to straighten wrist toward the thumb side Do not allow the wrist to flex forward to extend backward Free Interpreter Hold for 30 seconds or ______ Services Repeat 2 times or __________ • In the hospital, ask BioEx Systems Inc.* your child’s nurse. -

The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications
diagnostics Article The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications F. Kip Sawyer 1,2,* , Joshua J. Stefanik 3 and Rebecca S. Lufler 1 1 Department of Medical Education, Tufts University School of Medicine, Boston, MA 02111, USA; rebecca.lufl[email protected] 2 Department of Anesthesiology, Stanford University School of Medicine, Stanford, CA 94305, USA 3 Department of Physical Therapy, Movement and Rehabilitation Science, Bouve College of Health Sciences, Northeastern University, Boston, MA 02115, USA; [email protected] * Correspondence: [email protected] Received: 20 May 2020; Accepted: 29 May 2020; Published: 2 June 2020 Abstract: Background: This study attempted to clarify the innervation pattern of the muscles of the distal arm and posterior forearm through cadaveric dissection. Methods: Thirty-five cadavers were dissected to expose the radial nerve in the forearm. Each muscular branch of the nerve was identified and their length and distance along the nerve were recorded. These values were used to determine the typical branching and motor entry orders. Results: The typical branching order was brachialis, brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, supinator, extensor digitorum, extensor carpi ulnaris, abductor pollicis longus, extensor digiti minimi, extensor pollicis brevis, extensor pollicis longus and extensor indicis. Notably, the radial nerve often innervated brachialis (60%), and its superficial branch often innervated extensor carpi radialis brevis (25.7%). Conclusions: The radial nerve exhibits significant variability in the posterior forearm. However, there is enough consistency to identify an archetypal pattern and order of innervation. These findings may also need to be considered when planning surgical approaches to the distal arm, elbow and proximal forearm to prevent an undue loss of motor function. -

Standing Shoulder Flexion with Resistance
Prepared by Samantha Bohy Michigan STEP 1 STEP 2 Standing Shoulder Flexion with Resistance REPS: 15 | SETS: 2 | WEEKLY: 5x | Setup Begin in a standing upright position holding one end of a resistance band anchored under your foot with your thumb pointing forward. Movement Lift your arm straight forward to shoulder height, then slowly lower it back down and repeat. STEP 1 STEP 2 Single Arm Shoulder Extension with Resistance REPS: 15 | SETS: 2 | WEEKLY: 5x | Setup Begin standing tall, holding the end of a band that is anchored in front of you. Movement Pull your arm back, bringing your hand behind you. Return to the starting position and repeat. STEP 1 STEP 2 Standing Single Arm Shoulder Abduction with Resistance REPS: 15 | SETS: 2 | WEEKLY: 5x | Setup Begin in a standing upright position holding one end of a resistance band anchored under your feet with your thumb pointing up. Movement Lift your arm straight out to your side, to shoulder height, then lower it back down and repeat. Tip Make sure to maintain good posture and do not shrug your shoulder during the exercise. STEP 1 STEP 2 Shoulder Adduction with Anchored Resistance REPS: 15 | SETS: 2 | WEEKLY: 5x | Setup Begin in a standing upright position holding the end of a resistance band in one hand with your arm straight and palm facing downward, to the side of the anchor point. Movement Pull your arm down against the resistance band to your side, then slowly return to the starting position and repeat. STEP 1 STEP 2 Shoulder External Rotation with Anchored Resistance REPS: 15 | SETS: 2 | WEEKLY: 5x | Setup Begin standing upright with your elbow bent at 90 degrees and a towel roll tucked under your arm, holding a resistance band that is anchored out to your opposite side. -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -

Ulnar Nerve Injury & Repair
1/8/16 Ulnar Nerve Injury & Repair: Philadelphia’s Rehabilita6on & Ortho6c Magic Gardens Intervenon 1020 South Street Jenifer M. Haines,MS,OTR /L,CHT The Philadelphia Hand Center Outcomes Following Ulnar Nerve Repair Purpose: quan4fy variables influencing outcome aer 1. Outcomes & Expectaons ulnar & median nerve repair 2. Anatomy Methods: meta-analysis, literature review, 23 ar4cles 3. Clinical presentaon ulnar Results: nerve injury 1) 45% “sasfactory motor outcome” (71% < median nerve) 4. Func4onal deficits 41% “sasfactory sensory outcome” (approx. = median 5. Acute post-operave stage nerve) 6. ReHabilitaon stage 2) HigH level injury - poor motor outcome *irreversible motor damage by 1 ½-2 years (before re- innervaon of muscle) Ruijs, 2005 Long Term Outcomes of Ulnar 3) Paents < 16 years old 4x more likely sasfactory Nerve Injury motor recovery than those > 40 * neuroplas4city Purposes: 1. assess long term outcomes of paents following 4) Delayed surgery, lower cHance motor & sensory peripHeral repair recovery 2. determine relaonsHips between measures of Hand * Improvement possible up to 3 years func4on and nerve recovery. Methods: evaluated 32 paents approx. 5 years post-op Rosen and Lundborg scale, sensory, motor, and pain/ symptom tests, and self-report measures Ruijs, 2005 MacDermid J, 2010 1 1/8/16 Results: Paents retained 82.91% global func4on: 44.48%-84.90% sensory funcon “Factors that predict outcomes aer the repair of 80.13%-89.89% motor func4on peripHeral nerve injuries of the upper limb include age, 89.75%-93.19% pain/symptom experience gender, repair 4me, repair materials, defect length, duraon of follow-up and nerve injured.” Self-report measures of Hand func4on were more closely related to nerve recovery than were pHysical measures. -
The Appendicular Skeleton Appendicular Skeleton
THE SKELETAL SYSTEM: THE APPENDICULAR SKELETON APPENDICULAR SKELETON The primary function is movement It includes bones of the upper and lower limbs Girdles attach the limbs to the axial skeleton SKELETON OF THE UPPER LIMB Each upper limb has 32 bones Two separate regions 1. The pectoral (shoulder) girdle (2 bones) 2. The free part (30 bones) THE PECTORAL (OR SHOULDER) GIRDLE UPPER LIMB The pectoral girdle consists of two bones, the scapula and the clavicle The free part has 30 bones 1 humerus (arm) 1 ulna (forearm) 1 radius (forearm) 8 carpals (wrist) 19 metacarpal and phalanges (hand) PECTORAL GIRDLE - CLAVICLE The clavicle is “S” shaped The medial end articulates with the manubrium of the sternum forming the sternoclavicular joint The lateral end articulates with the acromion forming the acromioclavicular joint THE CLAVICLE PECTORAL GIRDLE - CLAVICLE The clavicle is convex in shape anteriorly near the sternal junction The clavicle is concave anteriorly on its lateral edge near the acromion CLINICAL CONNECTION - FRACTURED CLAVICLE A fall on an outstretched arm (F.O.O.S.H.) injury can lead to a fractured clavicle The clavicle is weakest at the junction of the two curves Forces are generated through the upper limb to the trunk during a fall Therefore, most breaks occur approximately in the middle of the clavicle PECTORAL GIRDLE - SCAPULA Also called the shoulder blade Triangular in shape Most notable features include the spine, acromion, coracoid process and the glenoid cavity FEATURES ON THE SCAPULA Spine -