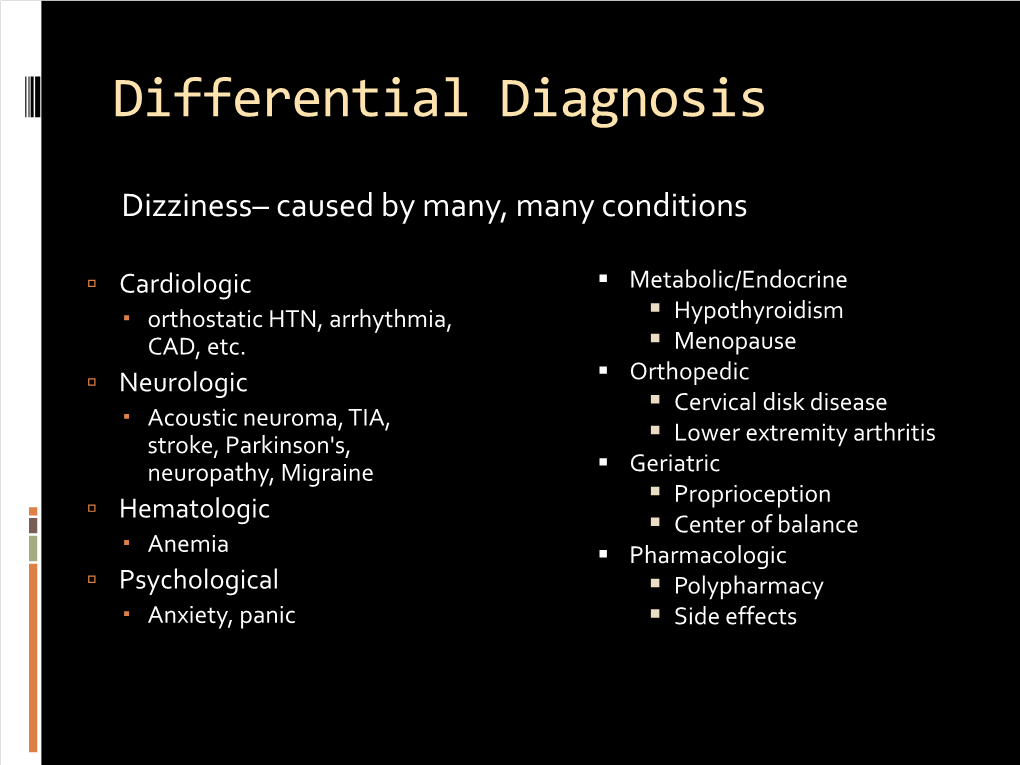
Differential Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Allergic Bronchopulmonary Aspergillosis Revealing Asthma
CASE REPORT published: 22 June 2021 doi: 10.3389/fimmu.2021.695954 Case Report: Allergic Bronchopulmonary Aspergillosis Revealing Asthma Houda Snen 1,2*, Aicha Kallel 2,3*, Hana Blibech 1,2, Sana Jemel 2,3, Nozha Ben Salah 1,2, Sonia Marouen 3, Nadia Mehiri 1,2, Slah Belhaj 3, Bechir Louzir 1,2 and Kalthoum Kallel 2,3 1 Pulmonary Department, Hospital Mongi Slim, La Marsa, Tunisia, 2 Faculty of Medicine, Tunis El Manar University, Tunis, Tunisia, 3 Parasitology and Mycology Department, La Rabta Hospital, Tunis, Tunisia Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disorder caused by hypersensitivity to Aspergillus which colonizes the airways of patients with asthma and cystic fibrosis. Its diagnosis could be difficult in some cases due to atypical Edited by: presentations especially when there is no medical history of asthma. Treatment of ABPA is Brian Stephen Eley, frequently associated to side effects but cumulated drug toxicity due to different molecules University of Cape Town, South Africa is rarely reported. An accurate choice among the different available molecules and Reviewed by: effective on ABPA is crucial. We report a case of ABPA in a woman without a known Shivank Singh, Southern Medical University, China history of asthma. She presented an acute bronchitis with wheezing dyspnea leading to an Richard B. Moss, acute respiratory failure. She was hospitalized in the intensive care unit. The Stanford University, United States bronchoscopy revealed a complete obstruction of the left primary bronchus by a sticky *Correspondence: Houda Snen greenish material. The culture of this material isolated Aspergillus fumigatus and that of [email protected] bronchial aspiration fluid isolated Pseudomonas aeruginosa. -

HEENT EXAMINIATION ______HEENT Exam Exam Overview
HEENT EXAMINIATION ____________________________________________________________ HEENT Exam Exam Overview I. Head A. Visual inspection B. Palpation of scalp II. Eyes A. Visual Acuity B. Visual Fields C. Extraocular Movements/Near Response D. Inspection of sclera & conjunctiva E. Pupils F. Ophthalmoscopy III. Ears A. External Inspection B. Otoscopy C. Hearing Acuity D. Weber/Rinne IV. Nose A. External Inspection B. Speculum/otoscope C. Sinus areas V. Throat/Mouth A. Mouth Examination B. Pharynx Examination C. Bimanual Palpation VI. Neck A. Lymph nodes B. Thyroid gland 29 HEENT EXAMINIATION ____________________________________________________________ HEENT Terms Acuity – (ehk-yu-eh-tee) sharpness, clearness, and distinctness of perception or vision. Accommodation - adjustment, especially of the eye for seeing objects at various distances. Miosis – (mi-o-siss) constriction of the pupil of the eye, resulting from a normal response to an increase in light or caused by certain drugs or pathological conditions. Conjunctiva – (kon-junk-ti-veh) the mucous membrane lining the inner surfaces of the eyelids and anterior part of the sclera. Sclera – (sklehr-eh) the tough fibrous tunic forming the outer envelope of the eye and covering all of the eyeball except the cornea. Cornea – (kor-nee-eh) clear, bowl-shaped structure at the front of the eye. It is located in front of the colored part of the eye (iris). The cornea lets light into the eye and partially focuses it. Glaucoma – (glaw-ko-ma) any of a group of eye diseases characterized by abnormally high intraocular fluid pressure, damaged optic disk, hardening of the eyeball, and partial to complete loss of vision. Conductive hearing loss - a hearing impairment of the outer or middle ear, which is due to abnormalities or damage within the conductive pathways leading to the inner ear. -

Temporo-Mandibular Joint (Tmj) Dysfunction
Office: (310) 423-1220 BeverlyHillsENT.com Fax: (310) 423-1230 TEMPORO-MANDIBULAR JOINT (TMJ) DYSFUNCTION You may not have heard of it, but you use it hundreds of times every day. It is the Temporo- Mandibular Joint (TMJ), the joint where the mandible (the lower jaw) joins the temporal bone of the skull, immediately in front of the ear on each side of your head. You move the joint every time you chew or swallow. You can locate this joint by putting your finger on the triangular structure in front of your ear. Then move your finger just slightly forward and press firmly while you open your jaw all the way and shut it. The motion you feel is the TMJ. You can also feel the joint motion in your ear canal. These maneuvers can cause considerable discomfort to a patient who is having TMJ trouble, and physicians use these maneuvers with patients for diagnosis. TMJ Dysfunction can cause the following symptoms: Ear pain Sore jaw muscles Temple/cheek pain Jaw popping/clicking Locking of the jaw Difficulty in opening the mouth fully Frequent head/neck aches The pain may be sharp and searing, occurring each time you swallow, yawn, talk, or chew, or it may be dull and constant. It hurts over the joint, immediately in front of the ear, but pain can also radiate elsewhere. It often causes spasms in the adjacent muscles that are attached to the bones of the skull, face, and jaws. Then, pain can be felt at the side of the head (the temple), the cheek, the lower jaw, and the teeth. -

FOCUSED PRACTICE in HOSPITAL MEDICINE Maintenance of Certification (MOC) Examination Blueprint
® FOCUSED PRACTICE IN HOSPITAL MEDICINE Maintenance of Certification (MOC) Examination Blueprint ABIM invites diplomates to help develop the Purpose of the Hospital Medicine MOC exam Hospital Medicine MOC exam blueprint The MOC exam is designed to evaluate the knowledge, Based on feedback from physicians that MOC assessments diagnostic reasoning, and clinical judgment skills expected of should better reflect what they see in practice, in 2016 the the certified hospitalist in the broad domain of the discipline. American Board of Internal Medicine (ABIM) invited all certified The exam emphasizes diagnosis and management of prevalent hospitalists and those enrolled in the focused practice program conditions, particularly in areas where practice has changed to provide ratings of the relative frequency and importance of in recent years. As a result of the blueprint review by ABIM blueprint topics in practice. diplomates, the MOC exam places less emphasis on rare This review process, which resulted in a new MOC exam conditions and focuses more on situations in which physician blueprint, will be used on an ongoing basis to inform and intervention can have important consequences for patients. update all MOC assessments created by ABIM. No matter For conditions that are usually managed by other specialists, what form ABIM’s assessments ultimately take, they will need the focus is on recognition rather than on management. The to be informed by front-line clinicians sharing their perspective exam is developed jointly by the ABIM and the American on what is important to know. Board of Family Medicine. A sample of over 100 hospitalists, similar to the total invited Exam format population of hospitalists in age, gender, geographic region, and time spent in direct patient care, provided the blueprint The traditional 10-year MOC exam is composed of 220 single- topic ratings. -

Rhinitis and Sinusitis
Glendale Animal Hospital 623-934-7243 www.familyvet.com Rhinitis and Sinusitis (Inflammation of the Nose and Sinuses) Basics OVERVIEW Rhinitis—inflammation of the lining of the nose Sinusitis—inflammation of the sinuses The nasal cavity communicates directly with the sinuses; thus inflammation of the nose (rhinitis) and inflammation of the sinuses (sinusitis) often occur together (known as “rhinosinusitis”) “Upper respiratory tract” (also known as the “upper airways”) includes the nose, nasal passages, throat (pharynx), and windpipe (trachea) “Lower respiratory tract” (also known as the “lower airways”) includes the bronchi, bronchioles, and alveoli (the terminal portion of the airways, in which oxygen and carbon dioxide are exchanged) SIGNALMENT/DESCRIPTION OF PET Species Dogs Cats Breed Predilections Short-nosed, flat-faced (known as “brachycephalic”) cats are more prone to long-term (chronic) inflammation of the nose (rhinitis), and possibly fungal rhinitis Dogs with a long head and nose (known as “dolichocephalic dogs,” such as the collie and Afghan hound) are more prone to Aspergillus (a type of fungus) infection and nasal tumors Mean Age and Range Cats—sudden (acute) viral inflammation of the nose and sinuses (rhinosinusitis) and red masses in the nasal cavity and throat (known as “nasopharyngeal polyps”) are more common in young kittens (6–12 weeks of age) Congenital (present at birth) diseases (such as cleft palate) are more common in young pets Tumors/cancer and dental disease—are more common in older pets Foreign -

Bronchiolitis
6 Sand Hill Road, Suite 102 Flemington, NJ 08822 PHONE 908-782-6700 FAX 908-788-5861 hunterdonpediatrics.org BRONCHIOLITIS Bronchiolitis is an infection of the small breathing tubes (bronchioles) that lead to the lung. Bronchiolitis is not the same as bronchitis, which is an infection in the large breathing tubes (bronchi). Bronchiolitis is usually seen in infants and young toddlers. It is not usually seen in older children or adults. A virus causes bronchiolitis. The most common virus is RSV (respiratory syncytial virus). Since RSV infection does not usually result in immunity, people can get it again; however, beyond the age of two, RSV usually causes just a bad cold. RSV is very contagious and spreads rapidly through childcare groups and families from October through April. Some studies suggest that babies who get RSV are more likely to have asthma in the future. Also, people with asthma who get RSV infection may trigger an asthma attack. Babies with RSV have severe nasal congestion, usually followed by a worsening cough. There may be a mild fever at the beginning of the illness. Signs of trouble with RSV include: ● Poor feeding/decreased urine output ● Rapid breathing ● Grunting sound with breathing ● Tightening of chest or stomach muscles with breathing ● Wheezing (high pitched whistling sound with breathing out) ● Blue tint around mouth or fingers/toes ● Fever lasting more than two days, or over 104 The vast majority of patients with bronchiolitis recover well. Certain children are especially likely to have trouble with bronchiolitis: ● Infants under two months of age ● Infants who were premature and have not reached their “due date” yet ● Patients with lung diseases like cystic fibrosis or bronchopulmonary dysplasia (BPD) ● Patients with severe heart disease ● Patients with AIDS or other immunity problems ● Patients on chemotherapy or with organ transplants Treatment for bronchiolitis is mostly supportive; that is, treatment is aimed at helping the patient breathe better. -

Respiratory Syncytial Virus Bronchiolitis in Children DUSTIN K
Respiratory Syncytial Virus Bronchiolitis in Children DUSTIN K. SMITH, DO; SAJEEWANE SEALES, MD, MPH; and CAROL BUDZIK, MD Naval Hospital Jacksonville, Jacksonville, Florida Bronchiolitis is a common lower respiratory tract infection in infants and young children, and respiratory syncytial virus (RSV) is the most common cause of this infection. RSV is transmitted through contact with respiratory droplets either directly from an infected person or self-inoculation by contaminated secretions on surfaces. Patients with RSV bronchiolitis usually present with two to four days of upper respiratory tract symptoms such as fever, rhinorrhea, and congestion, followed by lower respiratory tract symptoms such as increasing cough, wheezing, and increased respira- tory effort. In 2014, the American Academy of Pediatrics updated its clinical practice guideline for diagnosis and man- agement of RSV bronchiolitis to minimize unnecessary diagnostic testing and interventions. Bronchiolitis remains a clinical diagnosis, and diagnostic testing is not routinely recommended. Treatment of RSV infection is mainly sup- portive, and modalities such as bronchodilators, epinephrine, corticosteroids, hypertonic saline, and antibiotics are generally not useful. Evidence supports using supplemental oxygen to maintain adequate oxygen saturation; however, continuous pulse oximetry is no longer required. The other mainstay of therapy is intravenous or nasogastric admin- istration of fluids for infants who cannot maintain their hydration status with oral fluid intake. Educating parents on reducing the risk of infection is one of the most important things a physician can do to help prevent RSV infection, especially early in life. Children at risk of severe lower respiratory tract infection should receive immunoprophy- laxis with palivizumab, a humanized monoclonal antibody, in up to five monthly doses. -

Review of the Existing Recommendations for Essential Medicines for Ear, Nose and Throat Conditions in Adults and Children and Suggested Modifications
REVIEW OF THE EXISTING RECOMMENDATIONS FOR ESSENTIAL MEDICINES FOR EAR, NOSE AND THROAT CONDITIONS IN ADULTS AND CHILDREN AND SUGGESTED MODIFICATIONS 2012 Shelly Chadha, Andnet Kebede Prevention of Blindness and Deafness, World Health Organization REVIEW OF THE EXISTING RECOMMENDATIONS FOR ESSENTIAL MEDICINES (Ear, Nose and Throat conditions) FOR USE IN ADULTS AND CHILDREN AND SUGGESTED MODIFICATIONS Context: The WHO Essential Medicines List includes a section for ENT conditions in children. The current section does not make any reference to medicines and dosages recommended for adults. As most of the conditions for which the listed medicines are indicated, are common in adults, the list needs to be appropriately reviewed in that context. Methodology: Each of the medicines listed in the EML for children was reviewed to consider its appropriateness for inclusion in the EML for adults. The recommended dosages for adults and children were also considered. Recommendations: The medicine list should include a list for adults as well as children. The list for adults should include Xylometazoline hydrochloride nasal spray 0.1%. It should be stated that the medicine (xylometazoline nasal spray) should not be used for prolonged periods of time, unless specifically advised and under medical supervision. The adult list should also include the other medicines mentioned in the list of children, i.e.: o Ciprofloxacin ear drops: 0.3%, as hydrochloride, for tropical use. o Aectic acid ear drops, 2% in alcohol, for topical use. Budesonide nasal spray listed in the EML for children needs greater, in depth review, which may be considered for the next EML update. 1 Xylometazoline Hydrochloride nasal spray Indications: Nasal congestion is obstruction of nasal passages, mainly caused by mucosal inflammation due to increased venous engorgement, nasal secretions and tissue swelling. -

The Common Cold.Pdf
PATIENT TEACHING AID The Common Cold PERFORATION ALONG TEAR Everyone has experienced the misery of the common Rhinovirus Infection cold. A cold causes familiar symptoms such as a runny nose, sore throat, congestion, postnasal drip, and cough. For most sufferers, these symptoms are annoying, but not serious. Cold symptoms gradually improve and disappear over 7 to 10 days without complications. Colds are viral infections, so treatment with an antibiotic is not helpful. The best treatment for a cold is rest, fluids, and nonprescription medicines to help relieve symptoms. Although there is no vaccine to prevent colds, the spread of cold viruses can be slowed by frequent hand washing and avoiding close contact with those suffering from a cold. ILLUSTRATION: KRISTEN WIENANDT MARZEJON 2016 MARZEJON WIENANDT KRISTEN ILLUSTRATION: Copyright Jobson Medical Information LLC, 2016 continued MEDICAL PATIENT TEACHING AID Antibiotics Should Not Be Used to Treat a Cold Colds are caused by a variety of viruses, most commonly rhinoviruses. These viruses are highly contagious, and they are spread through the air or when someone is in contact with an infected person or contaminated object. There is no good evidence that exposure to cold or being overheated © Jobson Medical Information LLC, 2016 LLC, Information Medical Jobson © increases the risk of contracting a cold. Although most Wash your hands thoroughly and frequently colds occur in the winter months, some viruses that cause to prevent the spread of cold viruses. colds are more common in the fall or spring. Infants and young children are more prone to colds, as are people with weakened immunity. -

CASE REPORT 48-Year-Old Man
THE PATIENT CASE REPORT 48-year-old man SIGNS & SYMPTOMS – Acute hearing loss, tinnitus, and fullness in the left ear Dennerd Ovando, MD; J. Walter Kutz, MD; Weber test lateralized to the – Sergio Huerta, MD right ear Department of Surgery (Drs. Ovando and Huerta) – Positive Rinne test and and Department of normal tympanometry Otolaryngology (Dr. Kutz), UT Southwestern Medical Center, Dallas; VA North Texas Health Care System, Dallas (Dr. Huerta) Sergio.Huerta@ THE CASE UTSouthwestern.edu The authors reported no A healthy 48-year-old man presented to our otolaryngology clinic with a 2-hour history of potential conflict of interest hearing loss, tinnitus, and fullness in the left ear. He denied any vertigo, nausea, vomiting, relevant to this article. otalgia, or otorrhea. He had noticed signs of a possible upper respiratory infection, including a sore throat and headache, the day before his symptoms started. His medical history was unremarkable. He denied any history of otologic surgery, trauma, or vision problems, and he was not taking any medications. The patient was afebrile on physical examination with a heart rate of 48 beats/min and blood pressure of 117/68 mm Hg. A Weber test performed using a 512-Hz tuning fork lateral- ized to the right ear. A Rinne test showed air conduction was louder than bone conduction in the affected left ear—a normal finding. Tympanometry and otoscopic examination showed the bilateral tympanic membranes were normal. THE DIAGNOSIS Pure tone audiometry showed severe sensorineural hearing loss in the left ear and a poor speech discrimination score. The Weber test confirmed the hearing loss was sensorineu- ral and not conductive, ruling out a middle ear effusion. -

SEPTOPLASTY SURGICAL INFORMED CONSENT the Nasal
.SEPTOPLASTY SURGICAL INFORMED CONSENT The nasal septum is the wall inside your nose that divides it into two separate nasal passages. It is made of cartilage and bone. In a healthy nose, there is usually nearly equal airflow on both sides. Sometimes, the nasal septum is crooked or twisted. This condition is called a deviated nasal septum, and it can be caused by trauma to the nose, or patients can be born this way. The primary problem with a deviated nasal septum is nasal blockage, either on one or both sides. This nasal blockage can also contribute to nosebleeds, sinus infections, and often worsens obstructive sleep apnea. Occasionally, a deviated septum can be associated with a specific type of headache. A deviated septum can be surgically repaired with an operation called a septoplasty. This is typically done through a closed approach, which takes about one hour. More complicated or severely deviated septa may require an open approach, which can take up to 2-3 hours. In either case, septoplasty surgery is done under general anesthesia. It is an outpatient procedure so patients will be discharged home the same day. Some patients have multiple causes of nasal obstruction. Aside from a deviated septum, other reasons for a stuffy nose include chronic sinusitis, turbinate hypertrophy, nasal polyps, or nasal valve collapse. In these cases, septoplasty surgery may be performed in conjunction with other procedures such as endoscopic sinus surgery, turbinate reduction, or insertion of alar batten or spreader grafts. These procedures are discussed in their own individual sections on our website. Your physician will discuss what surgery is most appropriate for you. -

Other Work-Related Respiratory Disease Statistics in Great Britain, 2020 Allergic Alveolitis, Byssinosis and Allergic Rhinitis
Health and Safety Executive Data up to December 2019 Annual Statistics Published 4th November 2019 Other work-related respiratory disease statistics in Great Britain, 2020 Allergic alveolitis, byssinosis and allergic rhinitis Contents Other respiratory diseases 2 Farmer's lung and other allergic alveolitis 2 Byssinosis 3 Allergic rhinitis 3 The document can be found at: www.hse.gov.uk/statistics/causdis/ This document is available from www.hse.gov.uk/statistics/ Page 1 of 4 Other respiratory diseases This document outlines the available statistics for occupational respiratory diseases other than asbestos- related disease, asthma, Chronic Obstructive Pulmonary Disease (COPD) and pneumoconiosis which are covered elsewhere – see https://www.hse.gov.uk/statistics/causdis/index.htm. Farmer's lung and other allergic alveolitis Occupational Extrinsic Allergic Alveolitis (EAA) – also known as Occupational Hypersensitivity Pneumonitis – is inflammation of the alveoli within the lungs caused by an allergic reaction to inhaled material. “Farmer's lung”, which is caused by the inhalation of dust or spores arising from mouldy hay, grain or straw, is a common form of the disease. It is typically characterised by acute flu-like effects but can, in some cases, also lead to serious longer-term effects on lung function. There has been an average of 7 new cases of occupational EAA assessed for Industrial Injuries Disablement Benefit (IIDB) each year over the last decade, with about 15% of total cases being among women (Table IIDB01 www.hse.gov.uk/statistics/tables/iidb01.xlsx). There has also been an average of 7 deaths where farmer's lung (or a similar condition) was recorded as the underlying cause each year over the last decade (Table DC01 www.hse.gov.uk/statistics/tables/dc01.xlsx), with less than 10% of total deaths among women.