Askern Medical Practice Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

For Enquiries on This Agenda Please Contact
DONCASTER METROPOLITAN BOROUGH COUNCIL REGENERATION & HOUSING OVERVIEW & SCRUTINY PANEL MONDAY, 15TH OCTOBER, 2018 A MEETING of the REGENERATION & HOUSING OVERVIEW & SCRUTINY PANEL was held at the COUNCIL CHAMBER - CIVIC OFFICE, DONCASTER on MONDAY, 15TH OCTOBER, 2018 at 1.00 PM PRESENT: Chair - Councillor Paul Wray Councillors Duncan Anderson, Iris Beech and Steve Cox ALSO IN ATTENDANCE: Other Councillors; Councillor Richard A Jones Councillor Bill Mordue – Cabinet Member for Business, Skills and Economic Development DMBC; Jonathan Bucknall - Senior Strategy and Performance Manager Peter Lowe - Strategy and Performance Improvement Manager Drew Oxley - Head of Trading Services Richard Gibbons - Market Manager External; Dan Fell - Chief Executive Officer (Doncaster Chamber) Rebecca Leam - Policy & Communications Executive – (Doncaster Chamber) ACTION 1 APOLOGIES FOR ABSENCE. Apologies for absence were received from Councillors David Nevett, Charlie Hogarth and Eva Hughes. 2 TO CONSIDER THE EXTENT, IF ANY, TO WHICH THE PUBLIC AND PRESS ARE TO BE EXCLUDED FROM THE MEETING. There were no items on the agenda that contained exempt information. 3 DECLARATIONS OF INTEREST, IF ANY. There were no declarations of interest made. 4 PUBLIC STATEMENTS There were no public statements were made. 5 DONCASTER INCLUSIVE GROWTH STRATEGY 2018-21 A report was presented to the Panel on the latest Inclusive Growth Strategy. Members were provided with the draft document which detailed the level and type of reforms recommended for driving inclusive growth; why -

Breastfeeding Booklet
DONCASTER FAMILY HUBS Breastfeeding Support Information and Support for pregnant and breastfeeding women and their families. Take a look inside to see what Family Hubs can offer you and your new baby… Family Hubs can offer you information and support about breastfeeding during your pregnancy and when your baby is born. Midwives and health teams; our trained Hub Staff, and our Breastfeeding Peer Supporters will be happy to help. You will meet your Midwife and Health Team during your pregnancy and will also be invited to sessions at the Family Hub at various times during your pregnancy to meet with our staff and volunteer Peer Supporters. We then offer Breast Start and a range of groups for mums and babies where breastfeeding information and support is available. What is a Breastfeeding Peer Supporter? A woman who has breastfed a baby herself and; Lives locally Has undertaken training in breastfeeding and supporting women and can offer information, tips and hints to help you on your breastfeeding journey. Is able to listen to and support pregnant and breastfeeding women who may have questions, concerns or challenges. Someone who will befriend and support breastfeeding women in groups and other community settings, home visits, or on the telephone. Promotes breastfeeding in the community. What we want to do; Give women and their partners support when deciding how they will feed their baby. Support women to continue to breastfeed for as long as they want to. Talk to all family members e.g. partners and grandparents who would like to know more about breastfeeding and how they can support a breastfeeding mother. -

Publications List
Doncaster & District Family History Society Publications List August 2020 Parishes & Townships in the Archdeaconry of Doncaster in 1914 Notes The Anglican Diocese of Sheffield was formed in 1914 and is divided into two Archdeaconries. The map shows the Parishes within the Archdeaconry of Doncaster at that time. This publication list shows Parishes and other Collections that Doncaster & District Family History Society has transcribed and published in the form of Portable Document Files (pdf). Downloads Each Parish file etc with a reference number can be downloaded from the Internet using: www.genfair.co.uk (look for the Society under suppliers) at a cost of £6 each. Postal Sales The files can also be supplied by post on a USB memory stick. The cost is £10 each. The price includes the memory stick, one file and postage & packing. (The memory stick can be reused once you have loaded the files onto your own computer). Orders and payment by cheque through: D&DFHS Postal Sales, 18 Newbury Way, Cusworth, Doncaster, DN5 8PY Additional files at £6 each can be included on a single USB memory stick (up to a total of 4 files depending on file sizes). Example: One USB memory stick with “Adlingfleet” Parish file Ref: 1091 = £10. 1st Additional file at £6: the above plus “Adwick le Street” Ref: 1112 = Total £16. 2nd Additional file at £6: “The Poor & the Law” Ref: 1125 = Total £22 Postage included. We can also arrange payment by BACs, but for card and non-sterling purchases use Genfair While our limited stocks last we will also supply files in the form of a CD at £6 each plus postage. -

To Registers of General Admission South Yorkshire Lunatic Asylum (Later Middlewood Hospital), 1872 - 1910 : Surnames L-R
Index to Registers of General Admission South Yorkshire Lunatic Asylum (Later Middlewood Hospital), 1872 - 1910 : Surnames L-R To order a copy of an entry (which will include more information than is in this index) please complete an order form (www.sheffield.gov.uk/libraries/archives‐and‐local‐studies/copying‐ services) and send with a sterling cheque for £8.00. Please quote the name of the patient, their number and the reference number. Surname First names Date of admission Age Occupation Abode Cause of insanity Date of discharge, death, etc No. Ref No. Laceby John 01 July 1879 39 None Killingholme Weak intellect 08 February 1882 1257 NHS3/5/1/3 Lacey James 23 July 1901 26 Labourer Handsworth Epilepsy 07 November 1918 5840 NHS3/5/1/14 Lack Frances Emily 06 May 1910 24 Sheffield 30 September 1910 8714 NHS3/5/1/21 Ladlow James 14 February 1894 25 Pit Laborer Barnsley Not known 10 December 1913 4203 NHS3/5/1/10 Laidler Emily 31 December 1879 36 Housewife Sheffield Religion 30 June 1887 1489 NHS3/5/1/3 Laines Sarah 01 July 1879 42 Servant Willingham Not known 07 February 1880 1375 NHS3/5/1/3 Laister Ethel Beatrice 30 September 1910 21 Sheffield 05 July 1911 8827 NHS3/5/1/21 Laister William 18 September 1899 40 Horsekeeper Sheffield Influenza 21 December 1899 5375 NHS3/5/1/13 Laister William 28 March 1905 43 Horse keeper Sheffield Not known 14 June 1905 6732 NHS3/5/1/17 Laister William 28 April 1906 44 Carter Sheffield Not known 03 November 1906 6968 NHS3/5/1/18 Laitner Sarah 04 April 1898 29 Furniture travellers wife Worksop Death of two -

Kingfishers Walk at Rotherham
TAYLOR WIMPEY Kingfishers Walk Kingfishers Walk is found just a short drive from Junction 36 of the M1, and offers a range of stylish homes to suit the first time buyer and those moving up to their dream detached property. The development offers a choice of 2, 3, 4 & 5 The Wath Festival, held every May bank holiday, is bedroom homes, and also features some designs the biggest folk festival of its kind in the region. from our new Distinctive Collection which has It is very much a community event with traditional dancing, been created to perfectly blend traditional styles Kingfishers Walk street performances, workshops, a children’s festival and with modern quality and specification. the famous throwing of bread buns from the Parish tower. Wath, traditionally a rural location, is undergoing huge at Rotherham Wath-upon-Dearne gives you that strong community redevelopment at Manvers with plans for a new leisure feel as well as great commuter links, making it the complex, consisting of a bowling alley and restaurants. perfect base for anyone looking for a new home. Work on the shopping park has already started and is sure to give the town the urban feel it desires. A contemporary mix of 2, 3, 4 & 5 bedroom homes Homes you’ll love, in a carefully chosen location. Look inside for development layout. TAYLOR WIMPEY Kingfishers Walk at Rotherham Current build area 227-238 YOU ARE HERE BINS Persimmon development CS Sales Information Centre 239 240 Existing development & Showhomes El El 241 24 25 26 22 23 27 242 Wh Ed Cr Cr 243 Footpath Cr Al Al -

Doncaster Metropolitan Borough Council
DONCASTER METROPOLITAN BOROUGH COUNCIL COUNCIL THURSDAY, 15TH SEPTEMBER, 2016 A MEETING of the COUNCIL was held at the CIVIC OFFICE on THURSDAY, 15TH SEPTEMBER, 2016, at 6.00 pm. PRESENT: Chair - Councillor David Nevett Vice-Chair - Councillor George Derx Mayor - Ros Jones Deputy Mayor - Councillor Glyn Jones Councillors Nick Allen, Nigel Ball, Iris Beech, Elsie Butler, Bev Chapman, Phil Cole, John Cooke, Tony Corden, Jane Cox, Steve Cox, Jessie Credland, Linda Curran, Susan Durant, Nuala Fennelly, Neil Gethin, Sean Gibbons, Pat Haith, John Healy, Rachel Hodson, Charlie Hogarth, Mark Houlbrook, Eva Hughes, Glyn Jones, Richard A Jones, Ros Jones, Majid Khan, Ted Kitchen, Pat Knight, Sue Knowles, Chris McGuinness, Sue McGuinness, John McHale, Bill Mordue, John Mounsey, Jane Nightingale, Andy Pickering, Cynthia Ransome, Andrea Robinson, Kevin Rodgers, Craig Sahman, Dave Shaw, Alan Smith, Clive Stone, Austen White, Sue Wilkinson, Jonathan Wood and Paul Wray. APOLOGIES: Apologies for absence were received from Councillors Joe Blackham, Rachael Blake, James Hart, Sandra Holland, Kenneth Keegan and Jane Kidd 30 Recent Death of Councillor Alan Jones, Ward Member for Norton and Askern Prior to the commencement of formal business, Elected Members, Officers and members of the public, observed a minute’s silence as a mark of respect and remembrance in relation to the death of Councillor Alan Jones, Ward Member for Norton and Askern on 16th August, who had passed away after a short illness. Members noted that Councillor Jones had been an Askern Spa Ward Member from May 2011 to 2015, and more recently, a Ward Member for Norton and Askern. During his time as a Councillor, he had sat on the Planning Committee since his election in 2011, and had served on all four Overview and Scrutiny Panels as well as the Audit Committee, and additionally represented the Council on the Scrutiny Panel for the Police and Crime Commissioner. -

Landscape Character and Capacity Study Doncaster Metropolitan Borough Council Further Investigations - Employment and Housing Sites June 2010
Landscape Character and Capacity Study Doncaster Metropolitan Borough Council Further Investigations - Employment and Housing Sites June 2010 Golder Associates (UK) Ltd Landscape Planning Golder House 2nd Floor Danum House Tadcaster Enterprise Park St Sepulchre Gate Station Road Doncaster Tadcaster DN1 1UB LS24 9JF LANDSCAPE CHARACTER AND CAPACITY STUDY Table of Contents 1.0 INTRODUCTION ........................................................................................................................................................ 1 1.1 Method .......................................................................................................................................................... 1 1.2 Stages of Assessment .................................................................................................................................. 2 2.0 EMP 1 – INLAND PORT .......................................................................................................................................... 10 2.1 Site Context ................................................................................................................................................ 10 2.2 Site Description ........................................................................................................................................... 10 2.3 Visual Sensitivity ......................................................................................................................................... 12 2.4 Landscape Sensitivity ................................................................................................................................ -
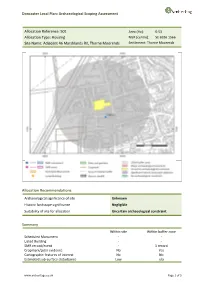
Doncaster Local Plan: Archaeological Scoping Assessment
Doncaster Local Plan: Archaeological Scoping Assessment Allocation Reference: 501 Area (Ha): 0.53 Allocation Type: Housing NGR (centre): SE 6936 1566 Site Name: Adjacent 46 Marshlands Rd, Thorne Moorends Settlement: Thorne Moorends Allocation Recommendations Archaeological significance of site Unknown Historic landscape significance Negligible Suitability of site for allocation Uncertain archaeological constraint Summary Within site Within buffer zone Scheduled Monument - - Listed Building - - SMR record/event - 1 record Cropmark/Lidar evidence No Yes Cartographic features of interest No No Estimated sub-surface disturbance Low n/a www.archeritage.co.uk Page 1 of 3 Doncaster Local Plan: Archaeological Scoping Assessment Allocation Reference: 501 Area (Ha): 0.53 Allocation Type: Housing NGR (centre): SE 6936 1566 Site Name: Adjacent 46 Marshlands Rd, Thorne Moorends Settlement: Thorne Moorends Site assessment Known assets/character: The SMR does not record any features within the site. One findspot is recorded within the buffer zone, a Bronze Age flint arrowhead. No listed buildings or Scheduled Monuments are recorded within the site or buffer zone. The Magnesian Limestone in South and West Yorkshire Aerial Photographic Mapping Project records levelled ridge and furrow remains within the buffer zone. The Historic Environment Characterisation records the present character of the site as modern commercial core- suburban, probably associated with the construction of Moorends mining village in the first half of the 20th century. There is no legibility of the former parliamentary enclosure in this area. In the western part of the buffer, the landscape character comprises land enclosed from commons and drained in 1825, with changes to the layout between 1851 and 1891 in association with the construction of a new warping system. -

Thorne and Moorends / Stainforth / Hatfield / Edenthorpe and Kirk Sandall / Armthorpe / Askern and Norton
Doncaster East Neighbourhood Newsletter - Thorne and Moorends / Stainforth / Hatfield / Edenthorpe and Kirk Sandall / Armthorpe / Askern and Norton April 2021 You said, we did Here are the issues you’ve talked to us about in the last month: Thorne and Moorends Speeding vehicles, antisocial behaviour, and parking Stainforth Antisocial behaviour and nuisance vehicles Hatfield Burglary, Nuisance motorbikes /quad bikes and speeding vehicles Edenthorpe and Kirk Sandall Nuisance vehicles, antisocial behaviour, and burglary Armthorpe Drugs, burglary, nuisance vehicles, antisocial behaviour Askern and Norton Antisocial behaviour, theft of vehicles and speeding vehicles In our crime and antisocial behaviour update, read about how your local officers are work alongside partner agencies and the community to address your key concerns. Crime and antisocial behaviour update Thorne and Moorends On Tuesday 13 April two warrants were carried out in Thorne during which, several knives were seized from an address on the Willow Estate. This warrant was part of ongoing work with partner agencies to tackle several issues, including antisocial behaviour on the Willow Estate. This picture was taken of a very large cannabis set up at an industrial estate on Coulman Street. There were over 1700 plants with an estimated value of £1 million. Three people were arrested and have since been charged in connection with the production of cannabis and remanded in custody. Stainforth and Barnby Dun On 31 March we held a day of action in the area. These photographs were taken during a warrant at the Transit Centre on Hall Road. We identified parts from 15 stolen vans and all the vehicle parts in the premises were recovered. -
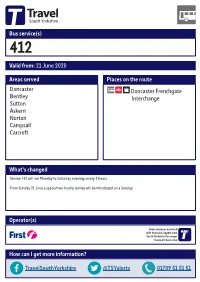
Valid From: 21 June 2020 Bus Service(S) What's Changed Areas
Bus service(s) 412 Valid from: 21 June 2020 Areas served Places on the route Doncaster Doncaster Frenchgate Bentley Interchange Sutton Askern Norton Campsall Carcroft What’s changed Service 412 will run Monday to Saturday evenings every 2 hours. From Sunday 21 June a special two hourly service will be introduced on a Sunday. Operator(s) Some journeys operated with financial support from South Yorkshire Passenger Transport Executive How can I get more information? TravelSouthYorkshire @TSYalerts 01709 51 51 51 Bus route map for service 412 19/07/2016# Norton, West End Rd/Broc-O-Bank Fenwick Ñ Norton Kirk Smeaton 412 Campsall, High St/ Campsall, Old Bells/High St Church View Moss Barnsdale Bar Campsall 412 Ñ Askern, Selby Rd/ Ð Campsall Rd Askern, Norbreck Rd/Plantation Cl Ô Askern Askern, Station Rd/High St Ò Sutton Sutton, Sutton Rd/Manor Farm Cl Burghwallis Braithwaite Owston Skellow Toll Bar, Doncaster Rd/Askern Rd Carcroft Barnby Dun Hampole Carcroft, High St/Park Av 412 Carcroft, High St/Queens Rd Toll Bar Adwick Le Street Toll Bar, Doncaster Rd/Bentley Moor Ln Woodlands Kirk Sandall Arksey Pickburn Highfields Scawthorpe Bentley Bentley, High St/Central Av Marr Scawsby database right 2016 and Wheatley yright Cusworth p o c own r C Intake data © y e v Sur e Sprotbrough c Doncaster, Frenchgate Interchange 412 dnan r O High Melton ontains Belle Vue C 6 = Terminus point = Public transport = Shopping area = Bus route & stops = Rail line & station = Tram route & stop Stopping points for service 412 Doncaster, Frenchgate Interchange North -

Hilton Park Askern, Doncaster a Little Bit About Us
Hilton Park Askern, Doncaster A little bit about us. We’re Gleeson and we specialise in building affordable, quality homes. We build homes where they are needed, for those who need them the most. We understand how Hilton Park is situated in the former colliery town of Askern. life-changing home ownership can be, which is why our friendly sales team is here to help you every step of the This exclusive development is ideally located within walking way. We’ll help find the right home for you, offer advice distance of the town centre where you’ll find plenty of local on the wide range of options to personalise your space and be there to hand over the keys to your new home. shops, a boating lake and pubs and takeaways. It’s also At Gleeson, we not only build homes, but we create an easy commute to Doncaster, Leeds and York. communities that you’ll love to be a part of. Building Homes. Changing Lives. welcome home • Excellent location for commuters, the • Nearby Doncaster has a wide variety development is close to the A19 with of bars, restaurants and shops as well easy access to the M62, M18 and A1 as direct train services into London • Great transport links with Adwick train • There is a selection of theatres and station less than four miles away with museums in Doncaster and the popular regular services to Leeds and Doncaster Yorkshire Wildlife Park which is just and a local bus stop with routes to 13 miles away Pontefract and Doncaster your home The Cork The Kerry The Tyrone The Galway The Kildare The Liffey The Longford The Carlow 2 bedroom semi-detached home 2 bedroom semi-detached home 3 bedroom semi-detached home 3 bedroom semi-detached home 3 bedroom detached home 3 bedroom detached home 4 bedroom detached home 4 bedroom detached home The Fergus The Lisburn The Woodford The Kilkenny The Cavan 3 bedroom semi-detached home 3 bedroom semi-detached home 3 bedroom semi-detached home 3 bedroom detached home 4 bedroom detached home Hilton Par k. -

South Yorkshire
INDUSTRIAL HISTORY of SOUTH RKSHI E Association for Industrial Archaeology CONTENTS 1 INTRODUCTION 6 STEEL 26 10 TEXTILE 2 FARMING, FOOD AND The cementation process 26 Wool 53 DRINK, WOODLANDS Crucible steel 27 Cotton 54 Land drainage 4 Wire 29 Linen weaving 54 Farm Engine houses 4 The 19thC steel revolution 31 Artificial fibres 55 Corn milling 5 Alloy steels 32 Clothing 55 Water Corn Mills 5 Forging and rolling 33 11 OTHER MANUFACTUR- Windmills 6 Magnets 34 ING INDUSTRIES Steam corn mills 6 Don Valley & Sheffield maps 35 Chemicals 56 Other foods 6 South Yorkshire map 36-7 Upholstery 57 Maltings 7 7 ENGINEERING AND Tanning 57 Breweries 7 VEHICLES 38 Paper 57 Snuff 8 Engineering 38 Printing 58 Woodlands and timber 8 Ships and boats 40 12 GAS, ELECTRICITY, 3 COAL 9 Railway vehicles 40 SEWERAGE Coal settlements 14 Road vehicles 41 Gas 59 4 OTHER MINERALS AND 8 CUTLERY AND Electricity 59 MINERAL PRODUCTS 15 SILVERWARE 42 Water 60 Lime 15 Cutlery 42 Sewerage 61 Ruddle 16 Hand forges 42 13 TRANSPORT Bricks 16 Water power 43 Roads 62 Fireclay 16 Workshops 44 Canals 64 Pottery 17 Silverware 45 Tramroads 65 Glass 17 Other products 48 Railways 66 5 IRON 19 Handles and scales 48 Town Trams 68 Iron mining 19 9 EDGE TOOLS Other road transport 68 Foundries 22 Agricultural tools 49 14 MUSEUMS 69 Wrought iron and water power 23 Other Edge Tools and Files 50 Index 70 Further reading 71 USING THIS BOOK South Yorkshire has a long history of industry including water power, iron, steel, engineering, coal, textiles, and glass.