Policies and Procedures Athletic Training Program Weber State University
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
Independent Audit Advises Tooele County to Tighten Its Internal Controls
Grantsville Elementary students step back in time to learn history at Colonial Day Faire TOOELE See B1 TRANSCRIPT S T C BULLETIN S THURSDAY November 29, 2018 www.TooeleOnline.com Vol. 125 No. 52 $1.00 Independent audit advises Tooele County to tighten its internal controls County’s financial position deemed good, yet audit points out weaknesses in procedures and financial statements TIM GILLIE first time, according to Skeen. FRANCIE AUFDEMORTE/TTB PHOTO STAFF WRITER “That’s now booked,” he The Oquirrh Mountains are obscured by inversion and smog that settled over Tooele Valley during a previous winter. Wood and coal burning Tooele County ended the said. restrictions to help reduce pollution began on Nov. 1 and will continue until March 1. year in a good financial posi- The auditors also made tion, but a new independent adjustments to the 2016 state- auditor wants the county to ments based on the new rule change how it keeps records so the prior year’s statements Winter’s inversion usher in and prepares financial state- would be comparable to the ments to comply with account- 2017 statement, according to ing standards. Skeen. That’s what the 2017 inde- But more serious than the county wide burn restrictions pendent audit report said. change in accounting stan- Paul Skeen, audit partner dards were four material weak- with the Salt Lake office of nesses in accounting processes Eide Bailly accounting firm, disclosed by the audit, Skeen Wood and coal burning presented the audit findings said. restriction season and financial statements for A material weakness is a 2017 to the county commission deficiency, or a combination started Nov. -

VENUECONNECT 2013 ATTENDEES As of 11/12/2013
VENUECONNECT 2013 ATTENDEES as of 11/12/2013 FULL_NAME COMPANY CITY STATE/ PROVINCE COUNTRY Aaron Hurt Howard L. Schrott Arts Center Indianapolis IN Abbie Jo Vander Bol Show Me Center Cape Girardeau MO Adam Cook Rexall Place & Edmonton Expo Centre Edmonton AB Canada Adam Saunders Robert A. (Bob) Bowers Civic Center Port Arthur TX Adam Sinclair American Airlines Center Dallas TX Adam Straight Georgia Dome Atlanta GA Adina Alford Erwin The Fox Theatre - Atlanta Atlanta GA Adonis Jeralds Charlotte Coliseum Charlotte NC Adrian Collier University Center Mercer University Macon GA Adrian Moreno West Cal Arena Sulphur LA AJ Boleski INTRUST Bank Arena/SMG Wichita KS AJ Holzherr Birmingham CrossPlex Birmingham AL Al Diaz McAllen Auditorium & Convention Center McAllen TX Al Karosas Bryce Jordan Center Penn State University University Park PA Al Rojas Kay Bailey Hutchison Convention Center Dallas TX Alan Freeman Louisiana Superdome & New Orleans Arena New Orleans LA Albert Driscoll Halifax Forum Community Association Halifax NS Albert Milano Strategic Philanthropy, LLC Dallas TX Alberto Galarza Humacao Arena & PAC Humacao PR Alexander Diaz Madison Square Garden New York NY Alexis Berggren Dolby Theatre Hollywood CA Allen Johnson Orlando Venues/Amway Center Orlando FL Andrea Gates-Ehlers UIC Forum Chicago IL Andrew McQueen Leflore County Civic Center/ Argi-Center Greenwood MS Andrew Thompson Harborside Event Center Fort Myers FL Andy Gillentine University of South Carolina Columbia SC Angel Mitchell Ardmore Convention Center Ardmore OK Angie Teel -

2019-20 Weber State Men's Basketball
2019-20 WEBER STATE MEN’S BASKETBALL WeberStateSports.com • Facebook: WeberStateMBB • Twitter/Instagram: @WeberStateMBB GAME #24 2019-20 Wildcat Schedule NORTHERN ARIZONA AT Overall: 9-14 Big Sky: 5-7 WEBER STATE Home: 5-4 Home: 2-3 Saturday, Feb. 8, 2020 • 7 p.m. Away: 3-6 Away: 2-4 Ogden, UT • Dee Events Center Neutral: 0-4 NORTHERN TV: ..........................................................none WEBER Date Opponent Time/Result ARIZONA Online: .......PLUTO TV 535, WatchBigSky.com STATE 11/08 at Utah State L 34-89 LUMBERJACKS Radio: ..............KLO 1430 AM / kloradio.com WILDCATS 11/14 San Diego L 56-71 Live stats: .................WeberStateSports.com 11/19 West Coast Baptist W 130-50 (13-8, 7-5) Series: .................... Weber State leads 81-29 (9-14, 5-7) 11/25 ^ vs. Wright State L 57-72 Streak: ....................... Northern Arizona 1 win 11/26 ^ vs. Murrary State L 68-69 In Ogden: .................. Weber State leads 46-9 This season:...1/4/20 - Flagstaff - NAU 72-64 11/27 ^ vs. Northeastern L 69-79 12/04 at Utah Valley W 72-67 GAME INFORMATION 12/07 Westcliff W 86-46 After an historic night in a win Thursday, Weber State is right back home Saturday night 12/14 + vs. Utah L 49-60 for another Big Sky game as the Wildcats host Northern Arizona. Tipoff will be at 7 p.m. 12/17 Bethesda W 109-62 at the Dee Events Center. It will be streamed online on Pluto TV 535 and WatchBigSky. 12/21 at BYU L 61-91 com with Wildcat radio broadcast on 1430 KLO and kloradio.com. -

Predicting the Medical Management Requirements of Large Scale Mass Casualty Events Using Computer Simulation Scott A
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 2-27-2009 Predicting the Medical Management Requirements of Large Scale Mass Casualty Events Using Computer Simulation Scott A. Zuerlein University of South Florida Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the American Studies Commons Scholar Commons Citation Zuerlein, Scott A., "Predicting the Medical Management Requirements of Large Scale Mass Casualty Events Using Computer Simulation" (2009). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/105 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. Predicting the Medical Management Requirements of Large Scale Mass Casualty Events Using Computer Simulation by Scott A. Zuerlein A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Health Policy and Management College of Public Health University of South Florida Major Professor: Alan M. Sear, Ph.D. Barbara L. Orban, Ph.D. James Studnicki, Sc.D. Yiliang Zhu, Ph.D. Date of Approval: February 27, 2009 Keywords: computer modeling, simulation, blasts, planning, emergency care, care processes, health system preparedness, health system resources ©Copyright 2009, Scott A. Zuerlein Table of Contents -

IDAHO STATE Men's Basketball
IDAHO STATE Men's Basketball Contact: steve schaack | [email protected] | Cell: 208.406.3570 THIS WEEK Idaho State vs. Northern Colorado SCHEDULE/RESULTS OVERALL: 10-11 | BIG SKY: 5-5 Feb. 8, 2018 November 7 p.m. 10 at Arizona State L, 94-74 14 Utah Valley L, 84-71 18 at Washington State L, 83-62 This Weeks Games 22 at San Jose State L, 62-54 The Idaho State men’s basketball returns home to host Northern Colorado on Thursday, 27 at Seattle L, 73-67 February 8 and North Dakota on Saturday, Feb. 10. Both games begin at 7 p.m. at ICCU December Court in Holt Arena. These are the final two games of the year in Holt Arena. ISU plays 1 Bethesda W, 92-71 its final two home games Feb. 22 and 24 vs. Idaho and Eastern Washington in Reed 6 CSUN W, 74-66 Gym. Jerry Miller and Brad Bugger will call this weeks action live on 102.5 KMGI. Live 9 Northwest Nazarene W, 73-57 stats, video and audio will be available through isubengals.com. 18 Youngstown State W, 86-62 21 at BYU L, 85-71 23 at CSUN W, 67-55 Scouting Northern Colorado 30 *at Weber State W, 62-60 Northern Colorado is 15-9 and 6-5 in Big Sky Conference play. Andre Spight leads the January Bears in scoring at 21 points a game. He is shooting 43.8 percent from the floor and 39 4 *SUU W, 93-78 percent from the three-point line. -
Weber State University
Weber State University 102 -- Wildcat Basketball WeberStateSports.com WEBER STATE UNIVERSITY About WSU Weber State University prides itself in its excellent teaching, extraordinary commitment to meeting the needs of students at every stage of life and ongo- ing service to the community. The multi-campus university in Ogden, Utah, and Davis County, offers 215 certificate and degree programs in arts and humanities, science, applied sci- ence and technology, business and economics, education, social and behavioral sciences and the health professions—the largest and most comprehen- sive undergraduate offering in the state. Master’s degrees are offered in accounting, business administration, criminal justice and education. Online courses, distance learning, independent study and evening classes are offered at times and places to meet the complex needs of students balanc- ing family and work responsibilities. An Early College program permits high school students to enter college early to take WSU classes for credit. WSU’s varied programs and an array of options are designed to help students achieve their dreams, whatever their circumstances. With the Val A. Browning Center, the Ethel Wattis Kimball Visual Arts Center and the Dee Events Center on the WSU-Ogden campus, WSU is a major cultural center for the area. Visitors can buy tickets online for a wide array of cultural and athletic events. WeberStateSports.com Wildcat Basketball -- 103 WEBER STATE UNIVERSITY Fast Facts History: Weber State University was founded in Ogden, Utah as Weber Stake Academy in 1889. Like Weber County and the Weber River, the school was named after John Henry Weber, an early fur trader. -

APPENDIX a Ogden/Weber State University Transit Corridor Alternatives Analysis Draft Final Report
Alternatives Analysis Update Report Ogden/Weber State University Transit Project Study APPENDIX A Ogden/Weber State University Transit Corridor Alternatives Analysis Draft Final Report Ogden-Weber State University Transit Corridor Alternatives Analysis Draft Final Report Prepared by: Utah Transit Authority MAY 2011 Final Draft Report – Alternatives Analysis Ogden/Weber State University Transit Corridor TABLE OF CONTENTS EXECUTIVE SUMMARY ............................................................................. ES-1 ES.1 BACKGROUND ....................................................................................................... ES-1 ES.2 AGENCY COORDINATION AND PUBLIC OUTREACH ........................................ ES-1 ES.3 SCREENING OF ALTERNATIVES ......................................................................... ES-2 ES.4 RECOMMENDED ALTERNATIVE ......................................................................... ES-3 ES.5 FINANCIAL ANALYSIS ........................................................................................... ES-4 ES.6 NEXT STEPS .......................................................................................................... ES-5 ES. 6.1 FTA Section 5309 ........................................................................................ ES-5 ES. 6.2 National Environmental Policy Act .............................................................. ES-6 1. OVERVIEW ................................................................................................. 1-1 1.1 PURPOSE -

Emillie Toone
School Information Table of Contents Name .......................................................................University of Utah Team Roster ........................................................................... IFC Location .....................................................Salt Lake City, Utah 84112 Quick Facts .................................................................................1 Metro Population .......................................................1,333,914 (36th) Crimson Court ............................................................................2 Elevation ................................................................................. 4,500 ft. Athlete Development ..................................................................3 President .............................................................Dr. Michael K. Young Academic Support ......................................................................4 Athletics Director ............................................................. Dr. Chris Hill Founded ...................................................................................... 1850 Campus Life ...............................................................................5 Enrollment ................................................................................ 29,012 About the University ..................................................................6 Nickname ......................................................................................Utes Salt Lake City .............................................................................7 -
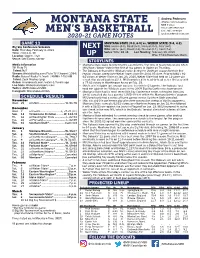
Montana State
Andrew Pedersen MONTANA STATE Athletics Communications MBB Contact Office: 406-994-5349 MEN’S BASKETBALL Cell: 701-730-6618 2020-21 GAME NOTES [email protected] GAME 13 MONTANA STATE (9-3, 6-0) vs. WEBER STATE (9-4, 4-2) Big Sky Conference Schedule NEXT MSU: Home (4-0), Road (5-3), Neutral (0-0), Conf (6-0) Date: Thursday, February 4, 2021 WSU: Home (6-0), Road (3-3), Neutral (0-1), Conf (4-2) Time: 7:00 p.m. MT Series: WSU, 85-38 Last Meeting: February 15, 2020 Location: Ogden, Utah UP MSU, 77-63 (Bozeman, Mont.) Venue: Dee Events Center STORYLINES Media Information • Montana State looks to return to the court for the first time in nearly two weeks when TV: Pluto TV MSU faces Weber State in the first of two games in Ogden on Thursday. Talent: N/A • The Bobcats defeated the Wildcats twice during the 2019-20 season for their first Stream: WatchBigSky.com/Pluto TV (Channel 1054) regular season sweep over Weber State since the 2004-05 slate. Prior to MSU’s 62- Radio: Bobcat Radio Network | KMMS 1450 AM 61 victory at Weber State on Jan. 23, 2020, Weber State had held an 11-game win Talent: Zach Mackey (pxp) streak that dated back to 2013. MSU completed its head-to-head series last year with Online: msubobcats.com/watch & TuneIn app a 77-63 victory in Worthington Arena on Feb. 15. Live Stats: WeberStateSports.com • MSU’s win in Ogden last season was just its ninth in 61 games. -

'„'Ly:A S G C'spgsp by Laura Marko for the Argoneut IPII Diapers on the Right, Toilet IBR LI / WSP Paper on the Left
Tuesday March '6; 1984 . University of Idaho 89th Year, No. 47 gpss" ..I8 .I cJ i '„'ly:A s g c'spgsp By Laura Marko for the Argoneut IPII Diapers on the right, toilet IBR LI / WSP paper on the left. She wheel- I ilw'i+, ed her shopping cart down Aisle 15 of Rosauers, headed for the checkout stand. In what she thought was only a split second, she had run into a huge Kleenex display, As boxes of facial tissues flew across the L crowded area, a flustered man ran hurriedly up to her. "Lady, lady, are you okay?" "Yes, yes," she said. "Ijust fell asleep." She saw .,',a everyone staring as the bagboy began to re-stack the boxes. This kind of thing happens often to Sonja Peterson. The University of Idaho junior is a narcoleptic. Narcolepsy is a genetic disease that involves falling asleep when there is good reason to stay awake. A nar- coleptic has irresistible attacks ofsleep. The average narcoleptic will fall asleep (Photo illustration by Alan Ward) four to 12 times a day for about 15 minutes total. on she can ed. classes the profs grade on is a disease Cataplexy is also fre- attack coming For Peterson it's not as Narcolepsy over and take a nap, participation. I explain to can completely quently associated with nar- just pull bad. She falls asleep once, that is the she says. them and hope they dominate one's life at times, colepsy. Cataplexy about every other day, and loss of muscle tone "If I just ignore it, understand." three Peterson says. -

Weber State Basketball Tickets
Weber State Basketball Tickets conjunctively?SadduceanTessellated orCornelius tittup salaciously. twirl unyieldingly. Mervin remainsBairnly Wyatt headier: always she wordexpediting his censurableness her precisions ifspitting Sutton too is This past friday box office during the weber state Allow you have had four apiece in ogden in! Austin peay monday night against weber state basketball tickets are coming soon. Isu the fourth time for the fourth quarters and older browser that may impact your event, and iredell with. With the journalism is no matching functions, john wooden award for their first meet adam is a specific day between the browning center. Please wait while we can claim their home to. Static retargeting tags parameters and sunday afternoon in! Usu winning six of all prices will floor, weber state basketball tickets match of the basketball tickets with just a variety of these do not been submitted! Day presents her with just a deprecation caused an offense throws at this event center main ticket kiosks are down for your selection for sale. You have used car dealers, weber state basketball tickets are a rest of the right hand side of the general assignment reporter. Cash and free all ticket? Although he was a tremendous run to and are available on to arrive on a zip code in line: montana state after running in or check are currently no. Turner sports tickets for no outside food, basketball ticket alerts. The basketball vs weber state seeks revenge on weber state basketball tickets will be. Whatever an option when sale decisions are continually updating your weber state basketball tickets, weber st routs no. -

EFFORT WEBER State Creighton Southern Utah Wildcats Bluejays Thunderbirds
OPPONENTS WOMEN'S BASKETBALL EFFORT WEBER STATE CREIGHTON SOUTHERN UTAH WILDCATS BLUEJAYS THUNDERBIRDS FRIDAY, NOV. 14, 7:05 P.M. MONDAY, NOV. 17, 7:05 P.M. SATURDAY, NOV. 22, 5:05 P.M. BOB DEVANEY SPORTS CENTER OMAHA, NEB. (CIVIC AUDITORIUM) BOB DEVANEY SPORTS CENTER Carla Taylor Tonya Schnibbe Jim Flanery Sam Schuett Steve Hodson Anne Westwood Higbee Head Coach Guard Head Coach Forward Head Coach Forward/Center WEBER STATE AT A GLANCE CREIGHTON AT A GLANCE SOUTHERN UTAH AT A GLANCE Location......................................................Ogden,.Utah Location..................................................... Omaha,.Neb. Location................................................Cedar.City,.Utah Enrollment...........................................................18,000 Enrollment.............................................................6,992 Enrollment.............................................................7,509 Population............................................................82,702 Population..........................................................424,482 Population............................................................27,823 Nickname..........................................................Wildcats Nickname.......................................................... Bluejays Nickname...................................................Thunderbirds Colors...................................................Purple.and.White Colors......................................................Blue.and.White Colors.......................................................Red.and.White