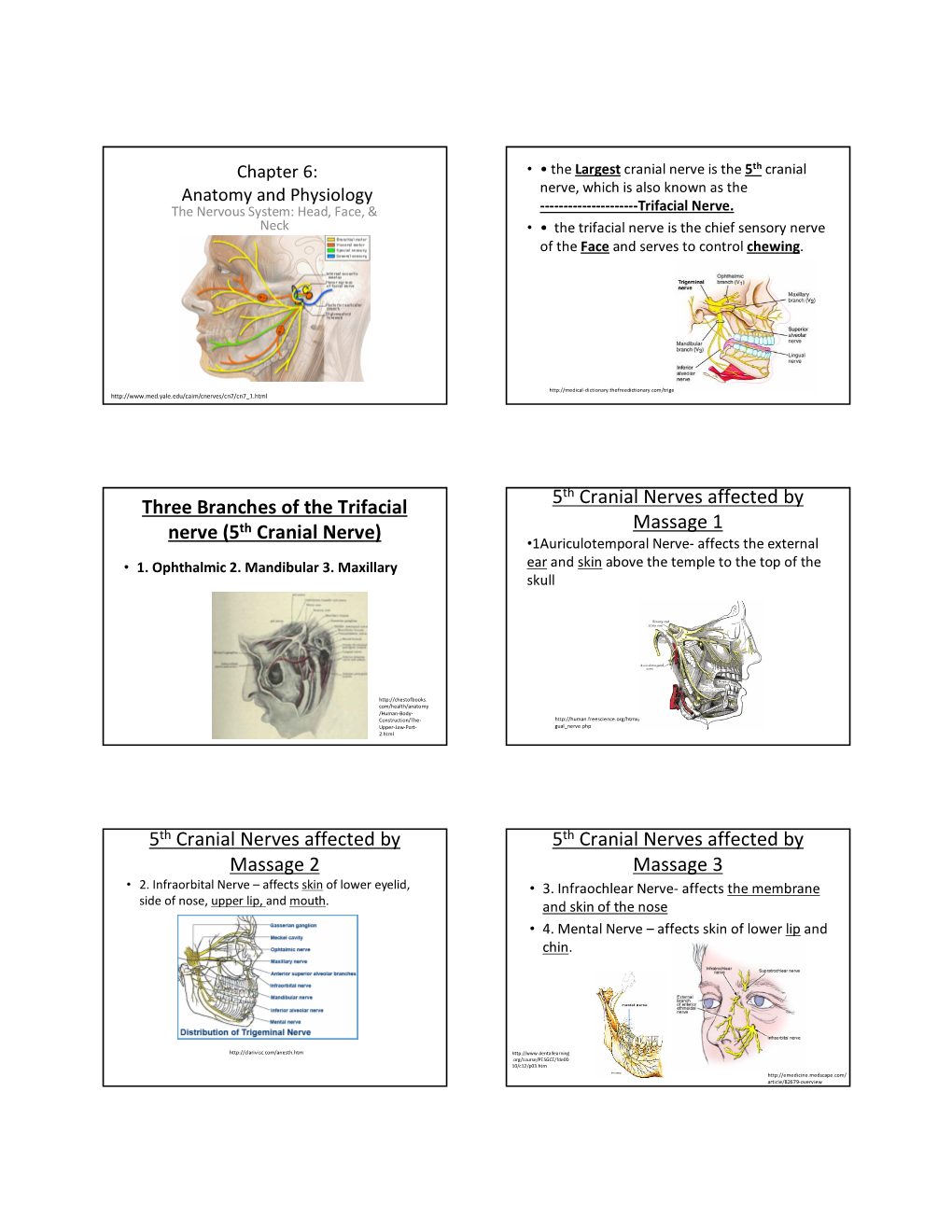
Three Branches of the Trifacial Nerve (5Th Cranial Nerve)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Numb Tongue, Numb Lip, Numb Chin: What to Do When?
NUMB TONGUE, NUMB LIP, NUMB CHIN: WHAT TO DO WHEN? Ramzey Tursun, DDS, FACS Marshall Green, DDS Andre Ledoux, DMD Arshad Kaleem, DMD, MD Assistant Professor, Associate Fellowship Director of Oral, Head & Neck Oncologic and Microvascular Reconstructive Surgery, DeWitt Daughtry Family Department of Surgery, Division of Oral Maxillofacial Surgery, Leonard M. Miller School of Medicine, University of Miami INTRODUCTION MECHANISM OF NERVE Microneurosurgery of the trigeminal nerve INJURIES has been in the spotlight over the last few years. The introduction of cone-beam When attempting to classify the various scanning, three-dimensional imaging, mechanisms of nerve injury in the magnetic resonance neurography, maxillofacial region, it becomes clear that endoscopic-assisted surgery, and use of the overwhelming majority are iatrogenic allogenic nerve grafts have improved the in nature. The nerves that are most often techniques that can be used for affected in dento-alveolar procedures are assessment and treatment of patients with the branches of the mandibular division of nerve injuries. Injury to the terminal cranial nerve V, i.e., the trigeminal nerve. branches of the trigeminal nerve is a well- The lingual nerve and inferior alveolar known risk associated with a wide range of nerve are most often affected, and third dental and surgical procedures. These molar surgery is the most common cause 1 injuries often heal spontaneously without of injury. medical or surgical intervention. However, they sometimes can cause a variety of None of these nerves provide motor symptoms, including lost or altered innervation. However, damage to these sensation, pain, or a combination of these, nerves can cause a significant loss of and may have an impact on speech, sensation and/or taste in affected patients. -

Anatomy of Maxillary and Mandibular Local Anesthesia
Anatomy of Mandibular and Maxillary Local Anesthesia Patricia L. Blanton, Ph.D., D.D.S. Professor Emeritus, Department of Anatomy, Baylor College of Dentistry – TAMUS and Private Practice in Periodontics Dallas, Texas Anatomy of Mandibular and Maxillary Local Anesthesia I. Introduction A. The anatomical basis of local anesthesia 1. Infiltration anesthesia 2. Block or trunk anesthesia II. Review of the Trigeminal Nerve (Cranial n. V) – the major sensory nerve of the head A. Ophthalmic Division 1. Course a. Superior orbital fissure – root of orbit – supraorbital foramen 2. Branches – sensory B. Maxillary Division 1. Course a. Foramen rotundum – pterygopalatine fossa – inferior orbital fissure – floor of orbit – infraorbital 2. Branches - sensory a. Zygomatic nerve b. Pterygopalatine nerves [nasal (nasopalatine), orbital, palatal (greater and lesser palatine), pharyngeal] c. Posterior superior alveolar nerves d. Infraorbital nerve (middle superior alveolar nerve, anterior superior nerve) C. Mandibular Division 1. Course a. Foramen ovale – infratemporal fossa – mandibular foramen, Canal -> mental foramen 2. Branches a. Sensory (1) Long buccal nerve (2) Lingual nerve (3) Inferior alveolar nerve -> mental nerve (4) Auriculotemporal nerve b. Motor (1) Pterygoid nerves (2) Temporal nerves (3) Masseteric nerves (4) Nerve to tensor tympani (5) Nerve to tensor veli palatine (6) Nerve to mylohyoid (7) Nerve to anterior belly of digastric c. Both motor and sensory (1) Mylohyoid nerve III. Usual Routes of innervation A. Maxilla 1. Teeth a. Molars – Posterior superior alveolar nerve b. Premolars – Middle superior alveolar nerve c. Incisors and cuspids – Anterior superior alveolar nerve 2. Gingiva a. Facial/buccal – Superior alveolar nerves b. Palatal – Anterior – Nasopalatine nerve; Posterior – Greater palatine nerves B. -

Numb Chin Sydrome : a Subtle Clinical Condition with Varied Etiology
OLGU SUNUMU / CASE REPORT Gülhane Tıp Derg 2015;57: 324 - 327 © Gülhane Askeri Tıp Akademisi 2015 doi: 10.5455/gulhane.44276 Numb chin sydrome : A subtle clinical condition with varied etiology Devika SHETTY (*), Prashanth SHENAI (**), Laxmikanth CHATRA (**), KM VEENA (**), Prasanna Kumar RAO (**), Rachana V PRABHU (**), Tashika KUSHRAJ (**) SUMMARY Introduction One of the rare neurologic symptoms characterized by hypoesthesia or Numb Chin Syndrome (NCS) is a sensory neuropathy cha- paresthesia of the chin and the lower lip, limited to the region served by the mental nerve is known as Numb chin syndrome. Vast etiologic factors have been racterized by altered sensation and numbness in the distribu- implicated in the genesis of numb chin syndrome. Dental, systemic and malignant tion of the mental nerve, a terminal branch of the mandibular etiologies have been well documented. We present a case of a 59 year old female patient who reported with all the classical features of numb chin syndrome. On division of trigeminal nerve. Any dysfunction along the course magnetic resonance imaging, the vascular compression of the trigeminal nerve of trigeminal nerve and its branches, intracranially and ext- root was evident which has been infrequently documented to be associated with racranially either by direct injury or compression of the nerve the condition. We have also briefly reviewed the etiology and pathogenesis of 1 numb chin syndrome and also stressed on the importance of magnetic resonance can predispose to NCS. Various etiologic factors have been imaging as an investigative modality in diagnosing the condition. considered of which dental procedures and dental pathologies Key Words: Numb Chin Syndrome, Mental nerve neuropathy, trigeminal nerve root, are the most common benign causes. -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery. -

PERFORATION of INFERIOR ALVEOLAR NERVE by MAXILLARY ARTERY Prakash Billakanti Babu, Ramachandra Bhat K, Vanishree S Nayak
Inferior alveolar nerve Rev Arg de Anat Clin; 2011, 3 (3): 124-129 __________________________________________________________________________________________ Case report PERFORATION OF INFERIOR ALVEOLAR NERVE BY MAXILLARY ARTERY Prakash Billakanti Babu, Ramachandra Bhat K, Vanishree S Nayak Kasturba Medical College, Manipal University, Manipal, Karnataka, India RESUMEN La fosa infratemporal es un área anatómica inferior alveolar nerve originated from the clínicamente importante para la administración de mandibular nerve by two roots and the first part agentes anestésicos locales en odontología y cirugía of the maxillary artery was incorporated between maxilofacial. Fueron estudiadas variaciones en la them. An embryologic origin of this variation and anatomía del nervio alveolar inferior y la arteria maxilar its clinical implications is discussed. Because the en la disección infratemporal. Durante la disección rutinaria de la cabeza en el cadáver de un varón maxillary artery runs between the two roots of the adulto, fue observada una variación excepcional en el inferior alveolar nerve, and the nerve was fixed origen del nervio alveolar inferior y su relación con las between the foramen ovale and mandibular estructuras circundantes. El nervio alveolar inferior se foramen, neurovascular entrapment may cause originaba en el nervio mandibular por dos raíces y la pain numbness or headache and may interfere primera parte de la arteria maxilar estaba incorporada with the injection of local anesthetics into the entre ambas. El origen embriológico de esta variación infratemporal fossa. Anatomical variations in this y sus implicaciones clínicas es debatido. Dado que la region should be kept in mind, particularly in arteria maxilar transcurría entre las dos raíces del cases of failed treatment of trigeminal neuralgia. -

Anatomy Respect in Implant Dentistry. Assortment, Location, Clinical Importance (Review Article)
ISSN: 2394-8418 DOI: https://doi.org/10.17352/jdps CLINICAL GROUP Received: 19 August, 2020 Review Article Accepted: 31 August, 2020 Published: 01 September, 2020 *Corresponding author: Dr. Rawaa Y Al-Rawee, BDS, Anatomy Respect in Implant M Sc OS, MOMS MFDS RCPS Glasgow, PhD, MaxFacs, Department of Oral and Maxillofacial Surgery, Al-Salam Dentistry. Assortment, Teaching Hospital, Mosul, Iraq, Tel: 009647726438648; E-mail: Location, Clinical Importance ORCID: https://orcid.org/0000-0003-2554-1121 Keywords: Anatomical structures; Dental implants; (Review Article) Basic implant protocol; Success criteria; Clinical anatomy Rawaa Y Al-Rawee1* and Mohammed Mikdad Abdalfattah2 https://www.peertechz.com 1Department of Oral and Maxillofacial Surgery, Al-Salam Teaching Hospital. Mosul, Iraq 2Post Graduate Student in School of Dentistry, University of Leeds. United Kingdom, Ministry of Health, Iraq Abstract Aims: In this article; we will reviews critically important basic structures routinely encountered in implant therapy. It can be a brief anatomical reference for beginners in the fi eld of dental implant surgeries. Highlighting the clinical importance of each anatomical structure can be benefi cial for fast informations refreshing. Also it can be used as clinical anatomical guide for implantologist and professionals in advanced surgical procedures. Background: Basic anatomy understanding prior to implant therapy; it's an important fi rst step in dental implant surgery protocol specifi cally with technology advances and the popularity of dental implantation as a primary choice for replacement loosed teeth. A thorough perception of anatomy provides the implant surgeon with the confi dence to deal with hard or soft tissues in efforts to restore the exact aim of implantation whether function or esthetics and end with improving health and quality of life. -

Anatomy of the Periorbital Region Review Article Anatomia Da Região Periorbital
RevSurgicalV5N3Inglês_RevistaSurgical&CosmeticDermatol 21/01/14 17:54 Página 245 245 Anatomy of the periorbital region Review article Anatomia da região periorbital Authors: Eliandre Costa Palermo1 ABSTRACT A careful study of the anatomy of the orbit is very important for dermatologists, even for those who do not perform major surgical procedures. This is due to the high complexity of the structures involved in the dermatological procedures performed in this region. A 1 Dermatologist Physician, Lato sensu post- detailed knowledge of facial anatomy is what differentiates a qualified professional— graduate diploma in Dermatologic Surgery from the Faculdade de Medician whether in performing minimally invasive procedures (such as botulinum toxin and der- do ABC - Santo André (SP), Brazil mal fillings) or in conducting excisions of skin lesions—thereby avoiding complications and ensuring the best results, both aesthetically and correctively. The present review article focuses on the anatomy of the orbit and palpebral region and on the important structures related to the execution of dermatological procedures. Keywords: eyelids; anatomy; skin. RESU MO Um estudo cuidadoso da anatomia da órbita é muito importante para os dermatologistas, mesmo para os que não realizam grandes procedimentos cirúrgicos, devido à elevada complexidade de estruturas envolvidas nos procedimentos dermatológicos realizados nesta região. O conhecimento detalhado da anatomia facial é o que diferencia o profissional qualificado, seja na realização de procedimentos mini- mamente invasivos, como toxina botulínica e preenchimentos, seja nas exéreses de lesões dermatoló- Correspondence: Dr. Eliandre Costa Palermo gicas, evitando complicações e assegurando os melhores resultados, tanto estéticos quanto corretivos. Av. São Gualter, 615 Trataremos neste artigo da revisão da anatomia da região órbito-palpebral e das estruturas importan- Cep: 05455 000 Alto de Pinheiros—São tes correlacionadas à realização dos procedimentos dermatológicos. -

A Review of the Mandibular and Maxillary Nerve Supplies and Their Clinical Relevance
AOB-2674; No. of Pages 12 a r c h i v e s o f o r a l b i o l o g y x x x ( 2 0 1 1 ) x x x – x x x Available online at www.sciencedirect.com journal homepage: http://www.elsevier.com/locate/aob Review A review of the mandibular and maxillary nerve supplies and their clinical relevance L.F. Rodella *, B. Buffoli, M. Labanca, R. Rezzani Division of Human Anatomy, Department of Biomedical Sciences and Biotechnologies, University of Brescia, V.le Europa 11, 25123 Brescia, Italy a r t i c l e i n f o a b s t r a c t Article history: Mandibular and maxillary nerve supplies are described in most anatomy textbooks. Accepted 20 September 2011 Nevertheless, several anatomical variations can be found and some of them are clinically relevant. Keywords: Several studies have described the anatomical variations of the branching pattern of the trigeminal nerve in great detail. The aim of this review is to collect data from the literature Mandibular nerve and gives a detailed description of the innervation of the mandible and maxilla. Maxillary nerve We carried out a search of studies published in PubMed up to 2011, including clinical, Anatomical variations anatomical and radiological studies. This paper gives an overview of the main anatomical variations of the maxillary and mandibular nerve supplies, describing the anatomical variations that should be considered by the clinicians to understand pathological situations better and to avoid complications associated with anaesthesia and surgical procedures. # 2011 Elsevier Ltd. -

The Mandibular Nerve: the Anatomy of Nerve Injury and Entrapment
5 The Mandibular Nerve: The Anatomy of Nerve Injury and Entrapment M. Piagkou1, T. Demesticha2, G. Piagkos3, Chrysanthou Ioannis4, P. Skandalakis5 and E.O. Johnson6 1,3,4,5,6Department of Anatomy, 2Department of Anesthesiology, Metropolitan Hospital Medical School, University of Athens Greece 1. Introduction The trigeminal nerve (TN) is a mixed cranial nerve that consists primarily of sensory neurons. It exists the brain on the lateral surface of the pons, entering the trigeminal ganglion (TGG) after a few millimeters, followed by an extensive series of divisions. Of the three major branches that emerge from the TGG, the mandibular nerve (MN) comprises the 3rd and largest of the three divisions. The MN also has an additional motor component, which may run in a separate facial compartment. Thus, unlike the other two TN divisions, which convey afferent fibers, the MN also contains motor or efferent fibers to innervate the muscles that are attached to mandible (muscles of mastication, the mylohyoid, the anterior belly of the digastric muscle, the tensor veli palatini, and tensor tympani muscle). Most of these fibers travel directly to their target tissues. Sensory axons innervate skin on the lateral side of the head, tongue, and mucosal wall of the oral cavity. Some sensory axons enter the mandible to innervate the teeth and emerge from the mental foramen to innervate the skin of the lower jaw. An entrapment neuropathy is a nerve lesion caused by pressure or mechanical irritation from some anatomic structures next to the nerve. This occurs frequently where the nerve passes through a fibro-osseous canal, or because of impingement by an anatomic structure (bone, muscle or a fibrous band), or because of the combined influences on the nerve entrapment between soft and hard tissues. -

The Course of the Buccal Nerve: Relationships with the Temporalis Muscle During the Prenatal Period
J. Anat. (2001) 198, pp. 423–429, with 8 figures Printed in the United Kingdom 423 The course of the buccal nerve: relationships with the temporalis muscle during the prenatal period ! ! ! 1 1 1 J. R. ME! RIDA-VELASCO , J. F. RODRI! GUEZ-VAZQUEZ , C. DE LA CUADRA , J. A. MERIDA-VELASCO2 AND J. JIMENEZ-COLLADO1 " Departamento de Ciencias MorfoloT gicas II, Facultad de Medicina, Universidad Complutense, Madrid, # and Departamento de Ciencias MorfoloT gicas, Facultad de Medicina, Universidad de Granada, Granada, Spain (Accepted 17 October 2000) The aim of this study was to describe the course of the buccal nerve and its relationships with the temporalis muscle during the prenatal period. Serial sections of 90 human fetal specimens ranging from 9 to 17 wk development were studied by light microscopy. Each fetal specimen was studied on both right and left sides, making a total of 180 cases for study. A 3-D reconstruction of the region analysed in one of the specimens was made. In 89 cases the buccal nerve was located medial to the temporalis muscle; in 73 cases it penetrated the muscle; in 15 cases it lay in a canal formed by the muscle fibres and was covered by fascia, and finally, in 3 cases it was a branch of the inferior alveolar nerve. The study has revealed that in a large number of cases the buccal nerve maintains an intimate association with the temporalis muscle. Key words: Buccal nerve; temporalis muscle. in relation to anaesthesia of the oral region through which it extends (Jablonski et al. 1985; Hendy & The buccal nerve, a branch of the mandibular division Robinson, 1994) whereas others studied the surgical of the trigeminal nerve, carries sensory fibres which anatomy of the nerve (Bozola et al. -

Trigeminal Nerve Anatomy
Trigeminal Nerve Anatomy Dr. Mohamed Rahil Ali Trigeminal nerve Largest cranial nerve Mixed nerve Small motor root and large sensory root Motor root • Nucleus of motor root present in the pons and medulla oblongata . • Motor fiber run with sensory fibers but its completely separated from it . • Motor fiber run under the gasserian ganglion and leave the middle cranial fossa through foramen ovale in association with the third division of the sensory root • Just after formen ovale it unit with the sensory root to form single nerve trunk which is mandibular branch of trigeminal nerve Motor fibers supply : 1. Masticatory muscles • Masseter • Temporalis Motor fibers supply : 1. Masticatory muscles • Masseter • Temporalis • medial and lateral pterygoid Motor fibers supply : 1. Masticatory muscles • Masseter • Temporalis • medial and lateral pterygoid 2. Mylohoid Motor fibers supply : 1. Masticatory muscles • Masseter • Temporalis • medial and lateral pterygoid 2. Mylohoid 3. Anterior belly of diagastric 4.Tensor tympani 5. Tensor palatini Motor fibers supply : 1. Masticatory muscles • Masseter • Temporalis • medial and lateral pterygoid 2. Mylohoid 3. Anterior belly of diagastric 4.Tensor tympani Sensory root • Sensory fibers meets in the trigeminal ganglia (gasserian ganglia) • There are two ganglia ( one in each side of cranial fossa) • These ganglia located in the meckels cavity in the petrous part of temporal bone • sensory nerve divided into threee branches Ophthalmic , maxillary , mandibular Ophthalmic branch • Travel through lateral wall of cavernous sinus Ophthalmic branch • Travel through lateral wall of cavernous sinus • Leave the cranial cavity through superior orbital fissure in to the orbit Ophthalmic branch • Supplies : eye ball , conjunctiva, lacrimal gland ,part of mucous membrane of nose and paranasal sinuses , skin of the forehead ,eyelids ,nose Ophthalmic branch Branches : 1. -

Mental Nerve Neuropathy: Case Report and Review
CASE REPORT • OBSERVATIONS DE CAS Mental nerve neuropathy: case report and review Amy Turner-Iannacci, DDS;* Eisa Mozaffari, DMD;† Eric T. Stoopler, DMD‡ ABSTRACT Mental nerve neuropathy (MNN) or “numb chin syndrome” is a rare neurologic symptom most of- ten associated with malignancy. Patients typically develop paresthesia or numbness localized to the chin and lower lip and will often seek care at their local emergency department. Pain and ex- pansion of the lower jaw may also be present. We report a case of MNN associated with a metastatic lesion in the mandible. The purpose of this article is to highlight the importance of rec- ognizing MNN, a potentially life-threatening symptom of metastatic carcinoma, and enable clini- cians to properly diagnose MNN, which may mimic other conditions that affect the mandible. Key words: mental nerve neuropathy, metastatic carcinoma RÉSUMÉ La neuropathie du nerf mentonnier est un symptôme neurologique rare le plus souvent associé aux tumeurs malignes. Les patients manifestent une paresthésie ou un engourdissement dans la région du menton et de la lèvre inférieure et rechercheront souvent des soins au département d’urgence local. On pourra noter également une douleur et une expansion de la mâchoire in- férieure. Nous présentons un cas de neuropathie du nerf mentonnier associée à des lésions métas- tatiques au niveau de la maxillaire inférieure. Le présent article a comme objectif de souligner l’importance de l’identification de la neuropathie du nerf mentonnier, un symptôme potentielle- ment fatal du cancer métastatique et d’aider le clinicien à diagnostiquer avec exactitude ce type de neuropathie pouvant être confondu avec d’autres atteintes de la maxillaire inférieure.