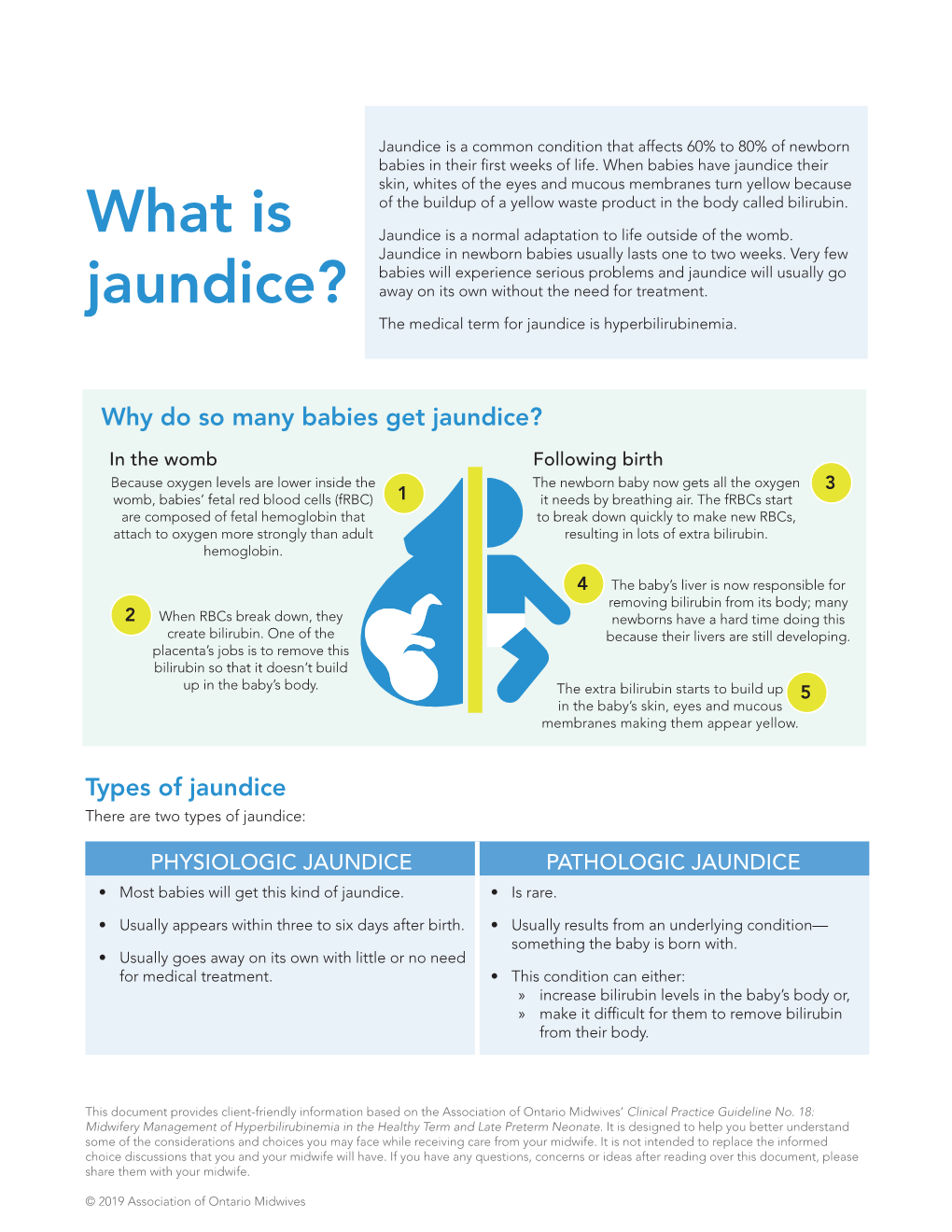
What Is Jaundice?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Successful Conservative Treatment of Pneumatosis Intestinalis and Portomesenteric Venous Gas in a Patient with Septic Shock
SUCCESSFUL CONSERVATIVE TREATMENT OF PNEUMATOSIS INTESTINALIS AND PORTOMESENTERIC VENOUS GAS IN A PATIENT WITH SEPTIC SHOCK Chen-Te Chou,1,3 Wei-Wen Su,2 and Ran-Chou Chen3,4 1Department of Radiology, Changhua Christian Hospital, Er-Lin branch, 2Department of Gastroenterology, Changhua Christian Hospital, 3Department of Biomedical Imaging and Radiological Science, National Yang-Ming University, and 4Department of Radiology, Taipei City Hospital, Taipei, Taiwan. Pneumatosis intestinalis (PI) and portomesenteric venous gas (PMVG) are alarming radiological findings that signify bowel ischemia. The management of PI and PMVG remain a challenging task because clinicians must balance the potential morbidity associated with unnecessary sur- gery with inevitable mortality if the necrotic bowel is not resected. The combination of PI, portal venous gas, and acidosis typically indicates bowel ischemia and, inevitably, necrosis. We report a patient with PI and PMVG caused by septic shock who completely recovered after conservative treatment. Key Words: bowel ischemia, computed tomography, pneumatosis intestinalis, portal venous gas, portomesenteric venous gas (Kaohsiung J Med Sci 2010;26:105–8) Pneumatosis intestinalis (PI) and portomesenteric CASE PRESENTATION venous gas (PMVG) are alarming radiologic findings that signify bowel ischemia [1]. PI and PMVG are A 78-year-old woman who presented with intermittent often described as an advanced sign of bowel injury, fever for 3 days was referred to the emergency depart- indicating irreversible injury caused by transmural ment of our hospital. The patient had a history of ischemia [2]. Bowel ischemia may be associated with type 2 diabetes mellitus, congestive heart failure, and perforation and has a high mortality rate. Many au- prior cerebral infarct. -

GASTROINTESTINAL COMPLAINT Nausea, Vomiting, Or Diarrhea (For Abdominal Pain – Refer to SO-501) I
DESCHUTES COUNTY ADULT JAIL SO-559 L. Shane Nelson, Sheriff Standing Order Facility Provider: October 17, 2018 STANDING ORDER GASTROINTESTINAL COMPLAINT Nausea, Vomiting, or Diarrhea (for Abdominal Pain – refer to SO-501) I. ASSESSMENT a. History i. Onset and duration ii. Frequency of vomiting, nausea, or diarrhea iii. Blood in stool or black stools? Blood in emesis or coffee-ground appearance? If yes, refer to SO-510 iv. Medications taken – do they help? v. Do they have abdominal pain? If yes, refer to SO-501 Abdominal Pain. vi. Do they have other symptoms – dysuria, urinary frequency, urinary urgency, urinary incontinence, vaginal/penile discharge, hematuria, fever, chills, flank pain, abdominal/pelvic pain in females or testicular pain in males, vaginal or penile lesions/sores? (if yes to any of the above – refer to Dysuria SO-522) vii. LMP in female inmates – if unknown, obtain HCG viii. History of substance abuse? Are they withdrawing? Refer to appropriate SO based on substance history and withdrawal concerns. ix. History of IBS or other known medical causes of chronic diarrhea, nausea, or vomiting? Have prescriptions been used for this in the past? x. History of abdominal surgeries? xi. Recent exposure to others with same symptoms? b. Exam i. Obtain Vital signs, including temperature ii. If complaints of dizziness or lightheadedness with standing, obtain orthostatic VS. iii. Is there jaundice present? iv. Are there signs of dehydration – tachycardia, tachypnea, lethargy, changes in mental status, dry mucous membranes, pale skin color, decreased skin turgor? v. Are you concerned for an Acute Gastroenteritis? Supersedes: March 20, 2018 Review Date: October 2020 Total Pages: 3 1 SO-559 October 17, 2018 Symptoms Exam Viruses cause 75-90% of acute gastroenteritis here in the US. -

Fever, Abdominal Pain, and Jaundice in a 43-Year-Old Woman
INTERNAL MEDICINE BOARD REVIEW DAVID L. LONGWORTH, MD, EDITOR JAMES K. STOLLER, MD, EDITOR KSRTI SHETTY, MD Dr. Shetty is a resident in internal medicine at the Cleveland Clinic. WILLIAM D. CAREY, MD Dr. Carey is head of the Section of Hepatology and director of the liver transplantation pro- gram at the Cleveland Clinic. He was recently president of the American College of Gastroenterology. Fever, abdominal pain, and jaundice in a 43-year-old woman WHAT IS THE DIAGNOSIS? 4 3-year-old Caucasian woman comes to the emergency room because of right On the basis of the clinical picture and upper abdominal pain that has lasted 2 1 laboratory data, what is the most likely days. The pain is dull and aching, is diagnosis? unrelated to food, and does not radiate. • Acute viral hepatitis AShe notes that her skin tone has become more • Acute cholecystitis yellowish lately, and her urine is dark. • Alcoholic hepatitis The patient says she has drunk three to • Acetaminophen toxicity four beers every day since the age of 18, and • Acute hepatic venous occlusion occasional drinks of vodka or gin on weekends. She abused intravenous drugs in her 20s, but This woman has the classic clinical triad of quit after successful drug rehabilitation. She alcoholic hepatitis: fever, jaundice, and tender has no history erf jaundice, hematemesis, mele- hepatomegaly.1 However, it is imperative to na, ascites, or encephalopathy. She has lost exclude other causes of abdominal pain, such approximately 15 lb over the past 6 months, as biliary tract obstruction, impaired hepatic and her appetite is poor. -

A Case of Pneumatosis Cytoides Intestinalis Successfully Treated by Inhalation of High Concentration Oxygen
Case Report A Case of Pneumatosis Cytoides Intestinalis Successfully Treated by Inhalation of High Concentration Oxygen JMAJ 48(10): 513–517, 2005 Toshihito Fujii,*1 Makoto Takaoka,*1 Yoshihiro Tagawa,*1 Takahiro Kitano,*1 Mika Ohmiya,*1 Yoshinari Hashimoto,*2 Kazuichi Okazaki*3 Abstract A 44-year-old man was referred to our hospital because of a positive fecal occult blood test. A barium enema study revealed numerous oval-shaped, elevated lesions with smooth surfaces in the region including the ascending colon. He was admitted to our hospital for investigation and therapy. Based on colonoscopic examination, we /5hoursןdiagnosed him as having pneumatosis cytoides intestinalis (PCI). He was treated with oxygen (5L/min day for 14 days) via a nasal cannula. Most of the multiple cysts diminished and some changed into white scars. The simplicity of oxygen therapy supports its use as a first-line treatment. Key words Pneumatosis cystoides interstinalis, High-concentration oxygen inhalation Family history: Not remarkable. Introduction Past exposure: No past exposure to trichloro- ethylene. Pneumatosis cystoides intestinalis (PCI) is a Present illness: The patient was found to be relatively rare condition in which numerous positive for fecal occult blood on a health screen- gas-filled cysts mainly containing nitrogen are ing, and was referred to our hospital for detailed formed within the intestinal wall. While idio- examination. An outpatient barium enema study pathic and secondary cases are known, the latter revealed numerous oval-shaped, elevated lesions may result from exposure to trichloroethylene, with smooth surfaces in the region from the chronic respiratory diseases such as pulmonary hepatic flexure to the ascending colon. -

Newborn Jaundice and Phototherapy
Newborn Jaundice/Phototherapy Jaundice is the yellow color seen in the skin of many newborns, and is usually harmless. Jaundice is caused by an excess of bilirubin in the blood. Bilirubin is made by the normal breakdown of red blood cells. Bilirubin is processed through the liver. Before the baby is born the mothers liver does this for the baby. After the baby is born, it might take a few days for the baby’s liver to get better at removing bilirubin. If the bilirubin becomes too high, it will need to be treated to prevent serious complications such as hearing loss, intellectual impairment and brain damage. A small instrument called a Bilimeter is used assess bilirubin levels. This is a non-invasive method and gives results in a matter of seconds. A graph is used to assess the age of an infant to the bilirubin level. If the level is moderate to high, a blood test is done to determine the exact level. Treatment for high bilirubin levels is done by phototherapy. Phototherapy is the use of special lights to help your baby break down the bilirubin. Treatment Expose as much of your baby’s skin to the lights as possible. A blood sample will be drawn on your baby to check the bilirubin level. This may happen more than once a day Keep your baby’s eyes covered with the mask provided while your baby is receiving phototherapy. while the lights are on. The baby can be in the room with you or in the nursery if Keep your baby under the lights as much as possible. -

Primary Biliary Cirrhosis
CASE REPORT Primary Biliary Cirrhosis Irvan Nugraha, Guntur Darmawan, Emmy Hermiyanti Pranggono, Yudi Wahyudi, Nenny Agustanti, Dolvy Girawan, Begawan Bestari Department of Internal Medicine, Faculty of Medicine, Universitas Padjajaran/Hasan Sadikin General Hospital, Bandung Corresponding author: *XQWXU'DUPDZDQ'HSDUWPHQWRI,QWHUQDO0HGLFLQH)DFXOW\RI0HGLFLQH8QLYHUVLWDV3DGMDMDUDQ-O3DVWHXU 1R%DQGXQJ,QGRQHVLD3KRQHIDFVLPLOH(PDLOJXQWXUBG#\DKRRFRP ABSTRACT 3ULPDU\ELOLDU\FLUUKRVLV 3%& LVDQLQÀDPPDWRU\GLVHDVHRUFKURQLFOLYHULQÀDPPDWLRQZLWKVORZSURJUHVVLYH FKDUDFWHULVWLFDQGLVDQXQNQRZQFKROHVWDWLFOLYHUGLVHDVHDQGFRPPRQO\KDSSHQLQPLGGOHDJHGZRPHQ7KH LQFLGHQFHRI3%&LV±SHUSHRSOHSHU\HDUSUHYDOHQFHRISHUSHRSOHDQG FRQWLQXHVWRLQFUHDVH%DVHGRQWKH$PHULFDQ$VVRFLDWLRQIRU6WXG\RI/LYHU'LVHDVHFULWHULDWKHGLDJQRVLVRI 3%&LVPDGHLQWKHSUHVHQFHRIWZRRXWRIWKUHHFULWHULDZKLFKDUHLQFUHDVHRIDONDOLQHSKRVSKDWDVHSRVLWLYH DQWLPLWRFKRQGULDODQWLERGLHV $0$ DQGKLVWRSDWKRORJ\H[DPLQDWLRQ :HUHSRUWHGDFDVHZKLFKLVYHU\UDUHO\IRXQGD\HDUROGZRPHQZLWKWKHFKLHIFRPSODLQWVRIGHFUHDVH FRQVFLRXVQHVVDQGMDXQGLFH,QSK\VLFDOH[DPLQDWLRQWKHUHZHUHDQDHPLFFRQMXQFWLYDLFWHULFVFOHUD KHSDWRVSOHQRPHJDO\SDOPDUHU\WKHPDDQGOLYHUQDLOV,QWKHSDWLHQWWKHUHZDVQRHYLGHQFHRIREVWUXFWLRQLQ LPDJLQJZLWKWZRIROGLQFUHDVHRIDONDOLQHSKRVSKDWDVHDQGSRVLWLYH$0$WHVW3DWLHQWZDVKRVSLWDOLVHGWRVORZ GRZQWKHSURJUHVVLRQRIWKHGLVHDVHDQGWRRYHUFRPHWKHVLJQV HJSUXULWXVRVWHRSRURVLVDQGVLFFDV\QGURPH Keywords:SULPDU\ELOLDU\FLUUKRVLVDONDOLQHSKRVSKDWDVHDQWLPLWRFKRQGULDODQWLERGLHV ABSTRAK 3ULPDU\ELOLDU\FLUUKRVLV 3%& PHUXSDNDQSHQ\DNLWLQÀPDVLDWDXSHUDGDQJDQKDWLNURQLNEHUVLIDWSURJUHVLI -

Hepatitis A, Acute
Hepatitis A, Acute *NOTE-HIGHLIGHTED SECTION HAS BEEN REVISED IMMEDIATELY REPORTABLE DISEASE Per NJAC 8:57, healthcare providers and administrators shall immediately report by telephone confirmed and suspected cases of acute hepatitis A to the health officer of the jurisdiction where the ill or infected person lives, or if unknown, wherein the diagnosis is made. The health officer (or designee) must immediately institute the control measures listed below in section 6, “Controlling Further Spread,” regardless of weekend, holiday, or evening schedules. A directory of local health departments in New Jersey is available at http://www.state.nj.us/health/lh/directory/lhdselectcounty.shtml If the health officer is unavailable, the healthcare provider or administrator shall make the report to the Department by telephone to 609.826.5964, between 8:00 A.M. and 5:00 P.M. on non-holiday weekdays or to 609.392.2020 during all other days and hours. June 2019 Hepatitis A, Acute 1 THE DISEASE AND ITS EPIDEMIOLOGY A. Etiologic Agent Hepatitis A is caused by the hepatitis A virus (HAV), a ribonucleic acid (RNA) agent classified as a Picornavirus. There is only one serotype worldwide; it is slow-growing in living cells and resistant to heat, solvents, and acid. Depending on conditions, HAV can be stable in the environment for months. Heating foods at temperatures greater than 185°F (>85°C) for one minute or disinfecting surfaces with a 1:100 dilution of sodium hypochlorite (i.e., household bleach) in tap water is necessary to inactivate HAV. The major site of viral replication is in the liver. -

A Case of Pneumoperitoneum Secondary to Pneumatosis Intestinalis: Is Surgery Always Indicated?
Bahrain Medical Bulletin, Vol. 39, No. 2, June 2017 A Case of Pneumoperitoneum Secondary to Pneumatosis Intestinalis: Is Surgery Always Indicated? Lulwa Al Mannaei, MD* Essam Mazen Jumaa, Arab Board (Gen Surg)** Pneumatosis intestinalis (PI) is a rare condition, which could be associated with a spectrum of disorders that vary from mild to life-threatening. We report a case of an eighty-five-year-old male who presented with abdominal distension and vomiting. Examination revealed the presence of peritoneal signs, with abdominal and pelvic CT confirming PI of the small bowel, a relatively rare condition. The patient underwent an exploratory laparotomy, during which, a segment of the terminal ileum was resected and an ileostomy was fashioned. The patient, unfortunately, died one month postoperatively due to postoperative complications. This case demonstrates the need for risk stratification guidelines to decide conservative or surgical management in cases of PI in this age group. Bahrain Med Bull 2017; 39(2): 113 - 115 PI is the presence of multiple gas cysts in the walls of the The patient was a known case of hypertension, diabetes small and large intestines1. It could affect all ages and the mellitus type 2 and schizophrenia. He had been confined to bed estimated prevalence is 0.02% to 0.003% worldwide2. It could for some time. He had no past surgical history and no history be primary or secondary1. The latter is usually associated with of previous hospital admissions. higher mortality rates, whereas the former is mostly benign and often considered an incidental finding. Most patients are On examination, the patient was conscious; however, he was asymptomatic. -

FDA Warns About Rare Occurrence of Serious Liver Injury with Use of Hepatitis C Medicines Mavyret, Zepatier, and Vosevi in Some Patients with Advanced Liver Disease
FDA Drug Safety Communication FDA warns about rare occurrence of serious liver injury with use of hepatitis C medicines Mavyret, Zepatier, and Vosevi in some patients with advanced liver disease Safety Announcement [08-28-2019] The Food and Drug Administration (FDA) has received reports that the use of Mavyret, Zepatier, or Vosevi to treat chronic hepatitis C in patients with moderate to severe liver impairment has resulted in rare cases of worsening liver function or liver failure. All these medicines contain a hepatitis C virus (HCV) protease inhibitor and are not indicated for use in patients with moderate to severe liver impairment. In most patients, symptoms resolved or new onset worsening of liver function improved after stopping the medicine. These medicines have been widely used and are safe and effective in patients with no or mild liver impairment. In many of the reported cases, liver failure occurred in patients who had signs and symptoms of moderate to severe liver impairment (Child-Pugh B or C) or other serious liver problems and should not have been treated with these medicines. In some cases, patients were reported to have no cirrhosis or compensated cirrhosis with mild liver impairment (Child-Pugh A) despite having evidence of decreased platelets at baseline or an increase in the pressure within the portal vein that carries blood from the digestive organs to the liver. In addition, some cases had other significant pre-existing risk factors such as liver cancer, alcohol abuse, or serious medical illnesses associated with serious liver problems. These factors may have contributed to clinical worsening of liver function or liver failure during treatment with these hepatitis C medicines. -

ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant 35 Weeks Or More of Gestation—Revised 2017
BREASTFEEDING MEDICINE Volume 12, Number 5, 2017 ABM Protocol ª Mary Ann Liebert, Inc. DOI: 10.1089/bfm.2017.29042.vjf ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant 35 Weeks or More of Gestation—Revised 2017 Valerie J. Flaherman,1 M. Jeffrey Maisels,2 and the Academy of Breastfeeding Medicine A central goal of The Academy of Breastfeeding Medicine is the development of clinical protocols free from commercial interest or influence for managing common medical problems that may impact breastfeeding success. These protocols serve only as guidelines for the care of breastfeeding mothers and infants and do not delineate an exclusive course of treatment or serve as standards of medical care. Variations in treatment may be appropriate according to the needs of an individual patient. Purpose depending on the racial and sociocultural population mix, about 75% have a transcutaneous bilirubin (TcB) of >100– 1. To provide guidance in determining whether and how 8–10 150 lmol/L (>6–9 mg/dL) by 96 hours. Bilirubin is breastfeeding may or may not be contributing to infant antioxidant and may protect infants from the relatively hy- jaundice. peroxygenic environment after birth. The term physiologic 2. To review evidence-based strategies for ameliorating jaundice is often used to describe newborns with a TSB well jaundice in the breastfeeding infant. above normal adult levels, but not attributable to a specific 3. To provide protocols for supporting breastfeeding while cause such as hemolytic disease; however, -
Fate of Patients with Obstructive Jaundice
ORIGINAL RESEARCH Fate of Patients with Obstructive Jaundice Einar Bjo¨rnsson, MD, PhD BACKGROUND/OBJECTIVE: Systematic data are limited on the etiology and progno- Jonas Gustafsson, MD sis of unselected patients with obstructive jaundice (OJ). We aimed to review the Jakob Borkman, MD clinical features, etiology, and prognosis of patients with OJ. Anders Kilander, MD, PhD METHODS: All adult patients with bilirubin Ն 5.85 mg/dL (100 mol/L) at a university hospital in Sweden in 2003-2004 were identified. Medical records from Department of Internal Medicine, Section of Gas- patients with OJ were reviewed. troenterology and Hepatology Sahlgrenska Univer- RESULTS: Seven hundred and forty-nine patients were identified, of whom 241 sity Hospital, Gothenburg Sweden (32%) had OJ (median age 71 years, 129 women). No one was lost to follow-up. The biliary obstruction of 154 patients (64%) was a result of a malignancy: 69 patients (46%) had pancreatic cancer, 44 (29%) had cholangiocarcinoma (CC), 5 (3%) had papilla vateri cancers, and 36 patients (23%) had other malignancies. Of the 87 patients with a benign obstruction, 57 (65%) had choledocholithiasis, 7 (8%) had biliary strictures, 6% had PSC, and the obstruction of 16 patients (20.7%) had other causes. A total of 115 of the 242 patients (48%) had abdominal pain associated with jaundice, whereas 52% had painless jaundice. Thirty-four percent of patients with a malignant obstruction had abdominal pain versus 71% of patients with a benign obstruction (P Ͻ .05). At the end of follow-up, only 5% (8 patients) with a malignant obstruction were alive versus 78% with a benign obstruction.