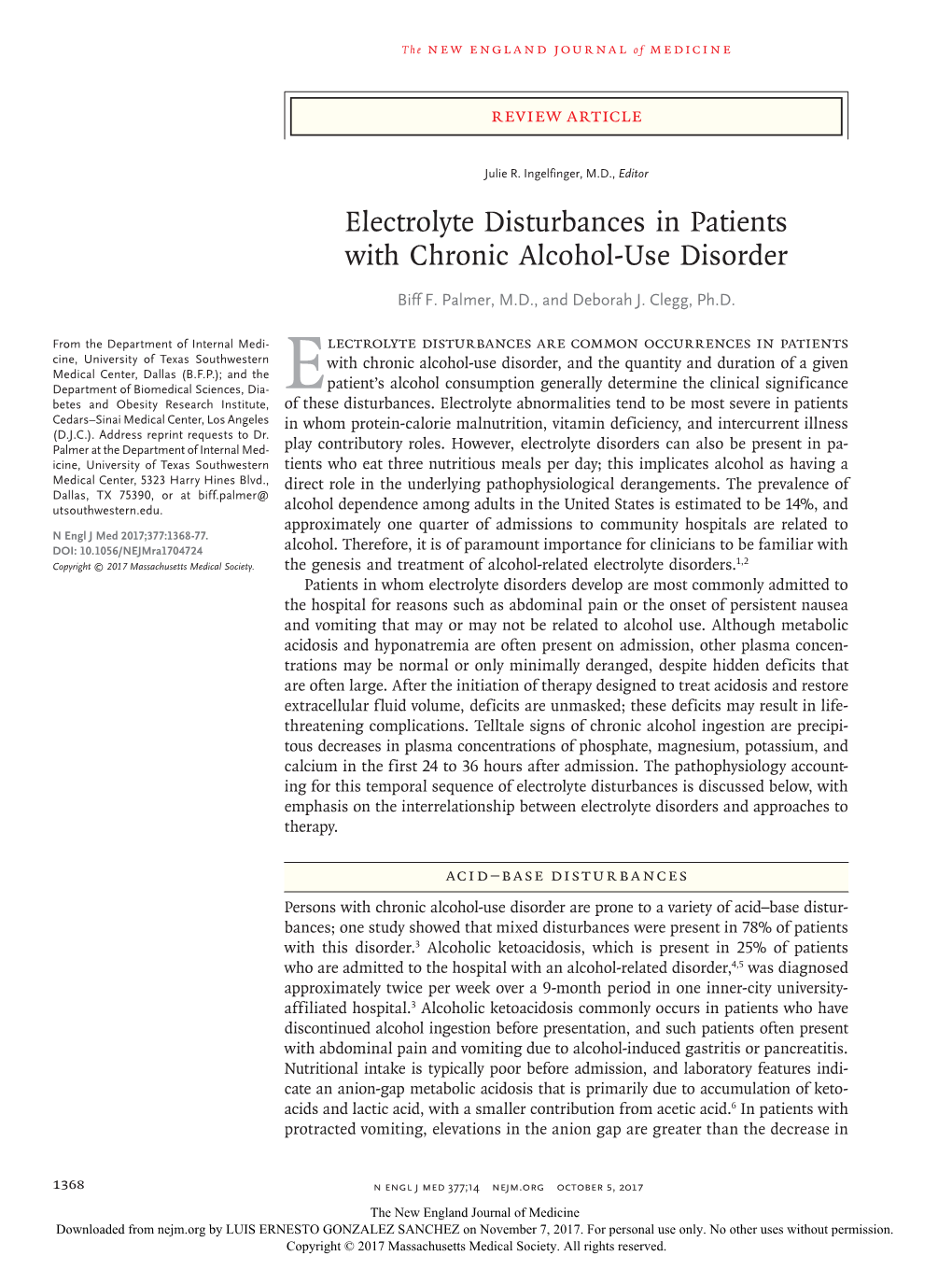
Electrolyte Disturbances in Patients with Chronic Alcohol-Use Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Magnesium Causes Nitric Oxide Independent Coronary Artery Vasodilation in Humans Heart: First Published As 10.1136/Hrt.86.2.212 on 1 August 2001
212 Heart 2001;86:212–216 Magnesium causes nitric oxide independent coronary artery vasodilation in humans Heart: first published as 10.1136/hrt.86.2.212 on 1 August 2001. Downloaded from H Teragawa, M Kato, T Yamagata, H Matsuura, G Kajiyama Abstract Objective—To determine how magnesium aVects human coronary arteries and whether endothe- lium derived nitric oxide (EDNO) is involved in the coronary arterial response to magnesium. Design—Quantitative coronary angiography and Doppler flow velocity measurements were used to determine the eVects of the nitric oxide synthase inhibitor NG-monomethyl-L-arginine (L-NMMA) on magnesium induced dilation of the epicardial and resistance coronary arteries. Setting—Hiroshima University Hospital a tertiary cardiology centre. Patients—17 patients with angiographically normal coronary arteries. Interventions—Magnesium sulfate (MgSO4) (0.02 mmol/min and 0.2 mmol/min) was infused for two minutes into the left coronary ostium before and after intracoronary infusion of L-NMMA. Main outcome measures—Diameter of the proximal and distal segments of the epicardial cor- onary arteries and coronary blood flow. Results—At a dose of 0.02 mmol/min, MgSO4 did not aVect the coronary arteries. At a dose of 0.2 mmol/min, MgSO4 caused coronary artery dilation (mean (SEM) proximal diameter 3.00 (0.09) to 3.11 (0.09) mm; distal 1.64 (0.06) to 1.77 (0.07) mm) and increased coronary blood flow (79.3 (7.5) to 101.4 (9.9) ml/min, p < 0.001 v baseline for all). MgSO4 increased the changes in these parameters after the infusion of L-NMMA (p < 0.001 v baseline). -

Risk Factors and Outcomes of Rapid Correction of Severe Hyponatremia
Article Risk Factors and Outcomes of Rapid Correction of Severe Hyponatremia Jason C. George ,1 Waleed Zafar,2 Ion Dan Bucaloiu,1 and Alex R. Chang 1,2 Abstract Background and objectives Rapid correction of severe hyponatremia can result in serious neurologic complications, including osmotic demyelination. Few data exist on incidence and risk factors of rapid 1Department of correction or osmotic demyelination. Nephrology, Geisinger Medical Center, Design, setting, participants, & measurements In a retrospective cohort of 1490 patients admitted with serum Danville, , Pennsylvania; and sodium 120 mEq/L to seven hospitals in the Geisinger Health System from 2001 to 2017, we examined the 2 incidence and risk factors of rapid correction and osmotic demyelination. Rapid correction was defined as serum Kidney Health . Research Institute, sodium increase of 8 mEq/L at 24 hours. Osmotic demyelination was determined by manual chart review of Geisinger, Danville, all available brain magnetic resonance imaging reports. Pennsylvania Results Mean age was 66 years old (SD=15), 55% were women, and 67% had prior hyponatremia (last outpatient Correspondence: sodium ,135 mEq/L). Median change in serum sodium at 24 hours was 6.8 mEq/L (interquartile range, 3.4–10.2), Dr. Alexander R. Chang, and 606 patients (41%) had rapid correction at 24 hours. Younger age, being a woman, schizophrenia, lower Geisinger Medical , Center, 100 North Charlson comorbidity index, lower presentation serum sodium, and urine sodium 30 mEq/L were associated Academy Avenue, with greater risk of rapid correction. Prior hyponatremia, outpatient aldosterone antagonist use, and treatment at an Danville, PA 17822. academic center were associated with lower risk of rapid correction. -

THE ACCUMULATION and DISTRIBUTION of EVANS BLUE in the KIDNEY of RATS FED NORMAL OR LOW MAGNESIUM DIETS by George Williams Seign
THE ACCUMULATION AND DISTRIBUTION OF EVANS BLUE IN THE KIDNEY OF RATS FED NORMAL OR LOW MAGNESIUM DIETS by George Williams Seignious, IV Thesis submitted to the Graduate Faculty of the Virginia Polytechnic Institute and State University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in ! Biochemistry and Nutrition APPROVED: G. E. Bunce, Chairman R. E. Webb ______ fl" ________ M;O. ......... ..;:;...; ___'"";:,....:; __.;..,. ___ _ _.. ''-.::;,,/ ___ , _______ ,_.._~_ M. H. Samli R. G. Saacke August, 1973 Blacksburg, Virginia . l\CKNOWLEDGMEN',rS The author of this thesis would like to e~press his deepest thanks and gra'titU;de to for his.continued help, advice, and . ·. .. : .. - understanding which made this thesis possible •. A special note of ·"· thanks is expressed.to whos_e invaluable help, advice arid suggestions aided greatly the author's efforts. The author would also like to thank for his. help and advice in the lab and all the other graduate students who made the author's stay at Virginia.Tech i{ very pleasant _one. Thanks is expressed to the author's wife, , for .her love, understanding, encouragement, and typing which· enabled the completion of this thesis. Also the author would like.to thank his parents for their lc;rving support and financial assistance. ii 'TABLE OF CONTENTS ACKNOWLEDGMENTS ii. TABLE OF CONTENTS . iii I,.IST OF TABLES iv LIST OF FIGURES Vi LIST OF SELECTED CHEMICAL STRUCTURES vii LIST OF·ABBREVIATIONS viii INTRODUCTION 1 LITERATURE REVIEW 5 EXPERIMENTAL PROCEDURES RESULTS 33 DISCUSSION 74 SUMMARY 82 REFERENCES 85 VITA 88 iii ~· ,,;. -

Alcohol Intoxication Withdrawal Adult
Provincial Clinical Knowledge Topic Alcohol Intoxication Withdrawal, Adult Emergency Department V 1.5 © 2018, Alberta Health Services. This work is licensed under the Creative Commons Attribution-Non-Commercial-No Derivatives 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/. Disclaimer: This material is intended for use by clinicians only and is provided on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness for a particular purpose of such information. This material is not a substitute for the advice of a qualified health professional. Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions, demands or suits arising from such use. Document History Version Date Description of Revision Completed By / Revised By 1.1 July 2015 Completed document (2013) reformatted into Dr. Bullard / Carla new topic template Milligan 1.2 January Minor edits in the Rationale section and form 1 Dr. Bullard / Sarah 2016 info in general care section as well as addition Searle of CIWA-Ar Scoring Reference tool to appendix 1.3 May 2016 Minor edits made to working group Sarah Searle membership list 1.4 June Removed link to Center for Addiction and Dr. Bullard / Sarah 2017 Mental Health assessment and documentation Searle form on pg. 35. Documentation requirements will continue as per local practice at this time. -
Drink Choices
Who is in the Tavern? - Drink Choices A bottle curiously labeled "DO NOT DRINK THIS EVER" A cherry cordial A Drake's Tongue. A little dab of Wyvern poison gives it it's zing! a dry mead with vanilla beans and cinnamon a dry red-brown ale a medium-bodied red wine with a smooth, dry finish A pale, watery ale A Polite Serving of Almond Milk Absynthe Abyssal Crimson Ale Aged Honey Mead Albis Shinehouse's Carrot Schnapps Ale All-or-Nothing Ale Alpine Herbal Soda Apple and Blackberry Cider Applejack Applejack Assassin Vine Wine Balik Stonefist's Mushroom Vodka Batmilk Stout beer Black Stout Blackberry Moonshine Blackwish Brewing Co. Pale Ale Blood Wine Bloody Mary Blue Dragon Wine Blue Moon Mist Blue Phoenix Elixir Blue Snow Water Butter Beer Chocolate Whiskey with Marshmallows Cloudberry Wine Cloudberry wine Cold almond milk Corpse Reviver #2 Critical Hit Dark Rum Deep Dwarf Dark Ale Demons Spit Stout Double Chocolate Stout Dragon Blood Tequila Dragon Sweat Dragon's Breath Ginger Beer Dragon's Breath Liquer Drambuie Dry red wine with sugared fruit slices. Dry white wine, aged in oak Dwarven Ale Dwarven Stout Elderblossom Wine Eleven Pear Cider from Imratheon Elorian Sprite Wine Elven Honey Mead Elven Pale Ale Elverquist (rare elven wine) Elvish Mint Tea Elvish Pale Ale Emerald Dream (absinthe) Fermented Owlbear Blood Firefly Ale -- For when you want to have a healthy glow about you. Firewine Five Foot's Frothingslosh Flametongue-Hellfire Pepper Porter fragrant mug of hot chamomile tea Ghost pepper pineapple juice Gimlet Ginger Scald Gnoll Booger -

A Temperate and Wholesome Beverage: the Defense of the American Beer Industry, 1880-1920
Portland State University PDXScholar Dissertations and Theses Dissertations and Theses Spring 7-3-2018 A Temperate and Wholesome Beverage: the Defense of the American Beer Industry, 1880-1920 Lyndsay Danielle Smith Portland State University Follow this and additional works at: https://pdxscholar.library.pdx.edu/open_access_etds Part of the United States History Commons Let us know how access to this document benefits ou.y Recommended Citation Smith, Lyndsay Danielle, "A Temperate and Wholesome Beverage: the Defense of the American Beer Industry, 1880-1920" (2018). Dissertations and Theses. Paper 4497. https://doi.org/10.15760/etd.6381 This Thesis is brought to you for free and open access. It has been accepted for inclusion in Dissertations and Theses by an authorized administrator of PDXScholar. Please contact us if we can make this document more accessible: [email protected]. A Temperate and Wholesome Beverage: The Defense of the American Beer Industry, 1880-1920 by Lyndsay Danielle Smith A thesis submitted in partial fulfillment of the requirements for the degree of Master of Arts in History Thesis Committee: Catherine McNeur, Chair Katrine Barber Joseph Bohling Nathan McClintock Portland State University 2018 © 2018 Lyndsay Danielle Smith i Abstract For decades prior to National Prohibition, the “liquor question” received attention from various temperance, prohibition, and liquor interest groups. Between 1880 and 1920, these groups gained public interest in their own way. The liquor interests defended their industries against politicians, religious leaders, and social reformers, but ultimately failed. While current historical scholarship links the different liquor industries together, the beer industry constantly worked to distinguish itself from other alcoholic beverages. -
Beer and Malt Handbook: Beer Types (PDF)
1. BEER TYPES The world is full of different beers, divided into a vast array of different types. Many classifications and precise definitions of beers having been formulated over the years, ours are not the most rigid, since we seek simply to review some of the most important beer types. In addition, we present a few options for the malt used for each type-hints for brewers considering different choices of malt when planning a new beer. The following beer types are given a short introduction to our Viking Malt malts. TOP FERMENTED BEERS: • Ales • Stouts and Porters • Wheat beers BOTTOM FERMENTED BEERS: • Lager • Dark lager • Pilsner • Bocks • Märzen 4 BEER & MALT HANDBOOK. BACKGROUND Known as the ‘mother’ of all pale lagers, pilsner originated in Bohemia, in the city of Pilsen. Pilsner is said to have been the first golden, clear lager beer, and is well known for its very soft brewing water, which PILSNER contributes to its smooth taste. Nowadays, for example, over half of the beer drunk in Germany is pilsner. DESCRIPTION Pilsner was originally famous for its fine hop aroma and strong bitterness. Its golden color and moderate alcohol content, and its slightly lower final attenuation, give it a smooth malty taste. Nowadays, the range of pilsner beers has extended in such a way that the less hopped and lighter versions are now considered ordinary lagers. TYPICAL ANALYSIS OF PILSNER Original gravity 11-12 °Plato Alcohol content 4.5-5.2 % volume C olor6 -12 °EBC Bitterness 2 5-40 BU COMMON MALT BASIS Pale Pilsner Malt is used according to the required specifications. -

Magnesium Production
Magnesium Production Subpart T, Greenhouse Gas Reporting Program Under the Greenhouse Gas Reporting Program (GHGRP), owners or operators of facilities that contain magnesium production processes must report emissions from use of cover and carrier gases as well as for all other source categories located at the facility for which methods are defined in the rule. Owners and operators are required to collect emission data, calculate greenhouse gas (GHG) emissions and follow the specified procedures for quality assurance, missing data, recordkeeping, and reporting per the requirements of 40 CFR Part 98 Subpart T – Magnesium Production. How Is This Source Category Defined? The magnesium production source category is defined as consisting of any process where magnesium metal is produced through smelting (including electrolytic smelting), refining, or remelting operations (including primary production facilities that extract magnesium from its ore and secondary production facilities that recover magnesium from scrap), or any process where molten magnesium is used in alloying, casting, drawing, extruding, forming, or rolling operations. Who Must Report? Magnesium production facilities that emit more than 25,000 metric tons CO2e per year. What Greenhouse Gases Must Be Reported? Each facility must report total annual emissions for each of the following greenhouse gases used in magnesium production facilities: ● Sulfur hexafluoride (SF6) ● HFC-134a ● The fluorinated ketone FK 5-1-12 ● Carbon dioxide (CO2) ● Any other GHG as defined in 40 CFR part 98, subpart A (General Provisions) of the rule In addition, the facility must report greenhouse gas emissions for any other source categories for which calculation methods are provided in the rule, as applicable. -

Diagnosis and Management of Hyponatremia Melinda Johnson, MD, FHM, FACP, FPHM Associate Professor, Internal Medicine University of Iowa Hospitals and Clinics
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Iowa Research Online UPDATED Diagnosis and Management of Hyponatremia Melinda Johnson, MD, FHM, FACP, FPHM Associate Professor, Internal Medicine University of Iowa Hospitals and Clinics Hyponatremia Low serum Normal or high osmolality serum <280 mOsm/kg osmolality Pseudo- Euvolemic Hypervolemic Redistributive Hypovolemic hyponatremia Una <20 mEq/L Una >20 mEq/L Una >20, Uosm Una >20, Uosm Una<20 mEq/L Una>20 mEq/L Uosm >300 Uosm <100 Hyperlipidemia Hyperglycemia <100 mOsm/kg >300 mOsm/kg mOsm/kg mOsm/kg Mannitol, Drug effect maltose, Advanced renal Hyper- Dehydration (thiazides, ACE- Beer potomania SIADH CHF sucrose, glycine, failure proteinemia I) or sorbitol administration Salt-wasting Psychogenic Diarrhea Postoperative Liver disease Biliary Azotemia nephropathies polydipsia Mineralocorti- Hypo- Nephrotic Alcohol Vomiting coid deficiency thyroidism syndrome intoxication Drug effect Cerebral (thiazides, ACE- sodium-wasting I) Adrenocorticotr opin deficiency Hyponatremia Serum sodium concentration <135 mEq/L Severe hyponatremia <120 mEq/L Disorder of water, not salt Occurs in ~15% of all hospital inpatients Increased morbidity and mortality Symptoms depend on rate of fall 1 Total Body Water Intracellular Interstitial Intravascular •Water load, causing decreased serum Sosm osmolality •Leading to suppressed ADH ADH (vasopressin) •Leading to water excretion in dilute Uosm urine (decreased Uosm) Impaired Renal Water Excretion 1. Inability to -

Development Laboratories for Alcoholic Beverages
Asahi Breweries, Ltd. Development Laboratories for Alcoholic Beverages Striving to create products that are sure to delight customers We are engaged in the development of new products across prod- uct lines including beer and related products (beer, happoshu [low-malt beer], new genre, etc.), ready-to-drink (RTD) alcoholic beverages (chuhai, cocktails, etc.), shochu, wine, and non-alcohol beverages (beer-taste and cocktail-taste beverages, etc.). From small-scale production of prototypes to follow-up for mass pro- duction at breweries and distilleries, we are always striving to create products that are sure to delight customers. Development of brewed alcoholic Development of RTD alcoholic Development of distilled beverages beverages alcoholic beverages When developing beer, wine and other For the development of canned chuhai and In the development of distilled alcoholic li- brewed alcoholic beverages, we produce cocktails, referred to as RTD alcoholic bev- quors such as shochu and spirits, a variety small batches of prototypes in a small-scale erages, we study techniques for preparing of factors and conditions need to be deter- plant to determine the flavor profile for the and blending ingredients such as fruit juice mined, from ingredient selection and pro- new product. Through this process, various and other flavoring agents to propose new cessing, yeast selection, as well as condi- factors and conditions will be determined flavors and meet the ever diversifying tions for wort preparation, fermentation, including the type and quantity of ingredi- tastes of consumers. We also explore and distillation, filtration, and maturation. New ents (malt, hop, grapes, etc.) to use, selec- evaluate new ingredients to create innova- product development entails the optimiza- tion of fermenting yeast, fermentation tem- tive flavors. -

Analytical Records Three Qualities
1265 130 is the conclusion of a story about a man who sold matter, 4’7 ° 58 per cent. The total nitrogen amounted to 4’00 an idea with money in it for a glass of beer. The astute per cent. Primox is a highly concentrated preparation and buyer of the idea, which was that of a zinc collar-pad should be useful as an emergency food. We attach little to prevent horses getting sore necks, argued "that the importance on dietetic grounds to the addition of vegetables matter oozing from the sores on the horses’ necks would in this preserved state. corrode the zinc pad and produce sulphate of zinc- LAUREL CAMPHOR SOAP (MILNE). thus the disease would provide its own remedy." It may be (THE GALEN MANUFACTURING Co., LIMITED. WiMON-STBEET, said that this was only the idea of the buyer, but the authors NEW CROSS-ROAD, LONDON, S.E.) of the book let it pass without a word of comment. Some This soap proved to be well made, containing a minimum salts of zinc would undoubtedly be produced, but surely not of moisture and giving absolutely no indication of alkaline the sulphate. However, as a whole the book puts the argu- excess. It is soft and agreeable to the skin and possesses an of ments for temperance in a forcible manner, but we do attractive odour. The soap is said to contain the oil think that in a book specially intended for schools such the camphor laurel, tar phenols and cymene. It yields a is suitable for errors as we have indicated should have no place. -

The Effects of Ethanol on Ketone Body Metabolism of Fasted Rats Henry S
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1975 The effects of ethanol on ketone body metabolism of fasted rats Henry S. Cabin Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Cabin, Henry S., "The effects of ethanol on ketone body metabolism of fasted rats" (1975). Yale Medicine Thesis Digital Library. 2432. http://elischolar.library.yale.edu/ymtdl/2432 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. YALE MEDICAL LIBRARY YALE MEDICAL LIBRARY Digitized by the Internet Archive in 2017 with funding from The National Endowment for the Humanities and the Arcadia Fund https://archive.org/details/effectsofethanolOOcabi The Effects of Ethanol on Ketone Body Metabolism of Fasted Rats by Henry S, Cabin B.A. University of Pennsylvania, 1971 Presented in partial fulfillment of the requirements for the degree of Doctor of Medicine, Yale University School of Medicine -March, 1975- ACKNOWLEDGEMENTS To Dr. Felig- who.has guided me through this research project from its inception, and for whom I have the highest esteem as a teacher, physician and human being. To Rosa, Bill and Andrea- without whose support and assistance this project would never have come to fruition.