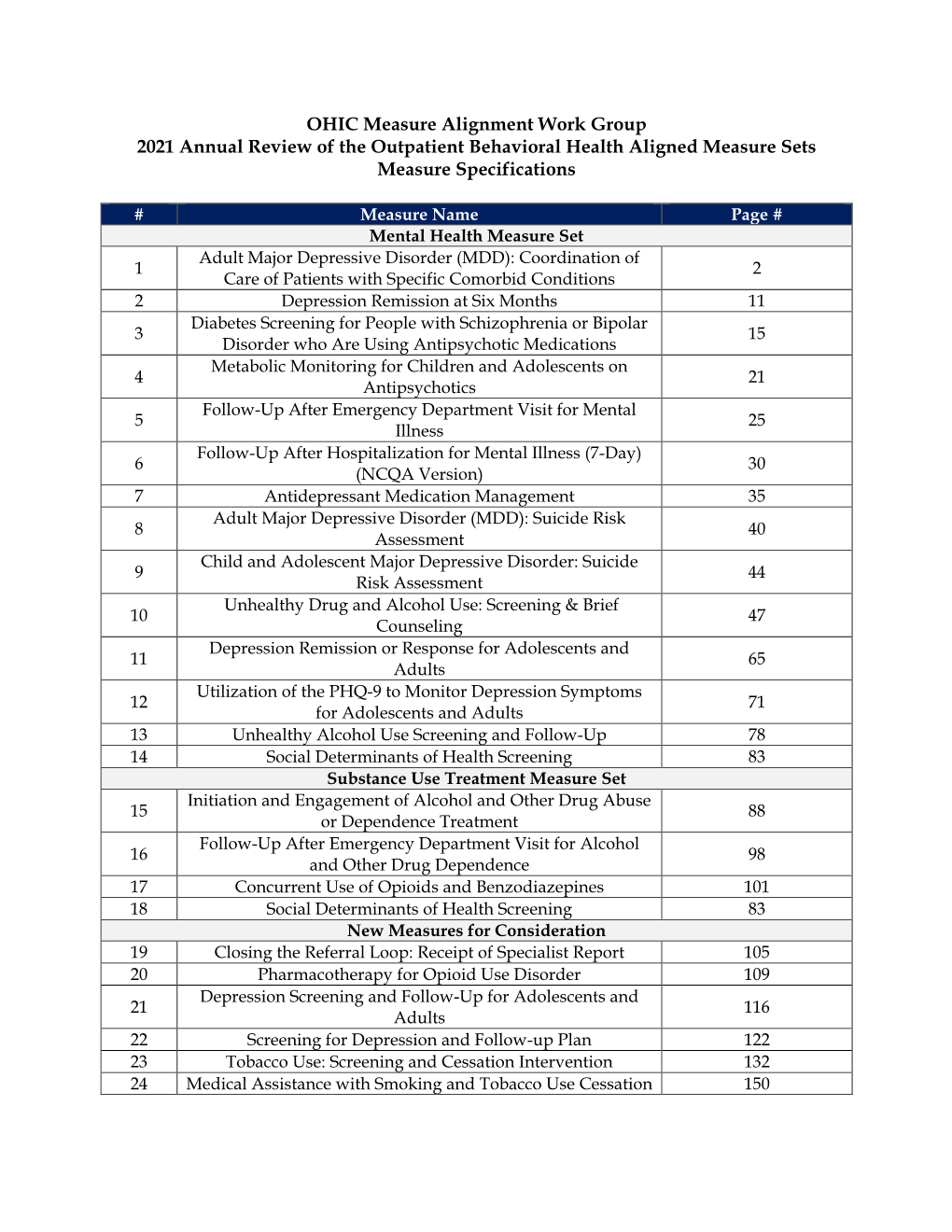
Outpatient BH Aligned Measure Set Specifications 2021 8-12
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologyonline 2: 252-260 (2006) Colovic Et Al
Pharmacologyonline 2: 252-260 (2006) Colovic et al. THE 1-(2,3-DICHLOROPHENYL)-PIPERAZINE-TO-ARIPIPRAZOLE RATIO AT STEADY STATE IN RATS AND SCHIZOPHRENIC PATIENTS Milena Colovica, Giuseppe Campianib, Stefania Butinib, Alberto Parabiaghia and Silvio Cacciaa aIstituto di Ricerche Farmacologiche “Mario Negri”, Milan, Italy bDipartimento Farmaco Chimico Tecnologico and European Research Centre for Drug Discovery and Development, Universita` di Siena, Siena, Italy Summary Aripiprazole metabolism includes N-dealkylation to 1-(2,3-dichlorophenyl)-piperazine which was present as a minor metabolite in serum of eight schizophrenic outpatients taking 5-15 mg/day. As phenylpiperazines concentrate in the brain, causing serotonin receptor-related effects, the authors examined the compounds’ concentrations in brain of rats given 10 mg/kg aripiprazole dihydrochloride orally, approximately every half-life for five half-lives, and evaluated the metabolite-to-parent drug ratio at steady state. The metabolite had higher brain uptake (about 26) than aripiprazole (about 5) and therefore the metabolite-to-parent drug ratio was higher in brain (0.43 ± 0.07, on molar basis) than in blood (0.08 ± 0.01). However, assuming that the compounds concentrate in human brain to the same extent as in the rat, one can conclude that at the site of action the metabolite represents only about 6% of aripiprazole. It is therefore conceivable that the metabolite contributes to the central effects of aripiprazole for rats, but this is unlikely for patients taking therapeutic doses. Key Words: Aripiprazole; 1-(2,3-dichlorophenyl)-piperazine; brain-to-blood distribution; metabolite-to-parent drug ratio With a pharmacological profile that differs from currently marketed antipsychotics for the treatment of schizophrenia and schizoaffective disorders, aripiprazole is a first-in-class drug. -

A Straightforward Route to Enantiopure Pyrrolizidines And
Molecules 2001, 6, 784-795 molecules ISSN 1420-3049 http://www.mdpi.org Biologically Active 1-Arylpiperazines. Synthesis of New N-(4- Aryl-1-piperazinyl)alkyl Derivatives of Quinazolidin-4(3H)-one, 2,3-Dihydrophthalazine-1,4-dione and 1,2-Dihydropyridazine- 3,6-dione as Potential Serotonin Receptor Ligands Piotr Kowalski1,*, Teresa Kowalska1, Maria J. Mokrosz2, Andrzej J. Bojarski2 and Sijka Charakchieva-Minol2 1 Institute of Organic Chemistry and Technology, Cracow University of Technology, 24 Warszawska str., 31-155 Cracow, Poland; 2 Department of Medicinal Chemistry, Institute of Pharmacology, Polish Academy of Sciences, 12 Smetna str., 31-343 Cracow, Poland * Author to whom correspondence should be addressed; e-mail: [email protected] Received: 26 February 2001; in revised form: 28 August 2001 / Accepted: 28 August 2001 / Published: 31 August 2001 Abstract: The synthesis of a series of new n-propyl and n-butyl chain containing 1-aryl- piperazine derivatives of quinazolidin-4(3H)-one (7) 2-phenyl-2,3-dihydrophthalazine-1,4- dione (8) and 1-phenyl-1,2-dihydropyridazine-3,6-dione (9) as potential serotonin receptor ligands is described. Keywords: Arylpiperazines, lactams, serotonin receptor ligands. Introduction Early studies by Hibert et al. have shown that there are two basic pharmacophore groups common to all five classes of 5-HT1A receptor ligands: a basic nitrogen atom and an aromatic ring with its centre positioned at a distance of 5.2-5.7 Å [1]. Since then several attempts have been made to extend that model, but the large diversity of ligand structures made definition of general interaction modes Molecules 2001, 6 785 impossible. -
2021 Unitedhealthcare PATH Reference Guide
UnitedHealthcare® Quality Reference Guide 2020/21 HEDIS,® CMS Part D, CAHPS® and HOS Measures HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). CAHPS® is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ). Information contained in this guide is based on NCQA HEDIS® technical specifications. For more details, please visit ncqa.org. ©2021 United HealthCare Services, Inc. We have the same goal: To help improve your patients’ health outcomes by identifying and addressing open care opportunities. Like you, we want your patients, who are UnitedHealthcare plan members, to be as healthy as possible. And a big part of that is making sure they get the preventive care and chronic care management they need. To help identify care opportunities, our PATH program gives you information specific to UnitedHealthcare members who are due or overdue for specific services. This reference guide can help you better understand the specifications for many of the quality measurement programs and tools used to address care opportunities, as well as how to report data and what billing codes to use. For additional PATH resources or to access this guide online, please visit UHCprovider.com/path. Insurance coverage provided by or through UnitedHealthcare Insurance Company or its affiliates. Health plan coverage provided by UnitedHealthcare of Arizona, Inc., UHC of California DBA UnitedHealthcare of California, UnitedHealthcare Benefits Plan of California, UnitedHealthcare of Colorado, Inc., UnitedHealthcare -

European Journal of Pharmacology 753 (2015) 2–18
European Journal of Pharmacology 753 (2015) 2–18 Contents lists available at ScienceDirect European Journal of Pharmacology journal homepage: www.elsevier.com/locate/ejphar Review Serotonin: A never-ending story Berend Olivier a,b,n a Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences & Brain Center Rudolf Magnus, Utrecht University, Universiteitsweg 99, 3584CG Utrecht, The Netherlands b Department of Psychiatry, Yale University School of Medicine, New Haven, USA article info abstract Article history: The neurotransmitter serotonin is an evolutionary ancient molecule that has remarkable modulatory Accepted 16 October 2014 effects in almost all central nervous system integrative functions, such as mood, anxiety, stress, aggression, Available online 7 November 2014 feeding, cognition and sexual behavior. After giving a short outline of the serotonergic system (anatomy, Keywords: receptors, transporter) the author's contributions over the last 40 years in the role of serotonin in Serotonin depression, aggression, anxiety, stress and sexual behavior is outlined. Each area delineates the work Depression performed on animal model development, drug discovery and development. Most of the research work Anxiety described has started from an industrial perspective, aimed at developing animals models for psychiatric Aggression diseases and leading to putative new innovative psychotropic drugs, like in the cases of the SSRI SSRI fluvoxamine, the serenic eltoprazine and the anxiolytic flesinoxan. Later this research work mainly focused Fluvoxamine on developing translational animal models for psychiatric diseases and implicating them in the search for mechanisms involved in normal and diseased brains and finding new concepts for appropriate drugs. & 2014 Elsevier B.V. All rights reserved. Contents 1. Serotonin, history, drugs . -

Download Product Insert (PDF)
PRODUCT INFORMATION Eltoprazine (hydrochloride) Item No. 18428 CAS Registry No.: 98206-09-8 H Formal Name: 1-(2,3-dihydro-1,4-benzodioxin-5-yl)- N piperazine, monohydrochloride Synonyms: DU-28,853, DU-28,893 MF: C H N O • HCl 12 16 2 2 N • HCl FW: 256.7 Purity: ≥98% O Stability: ≥2 years at -20°C Supplied as: A crystalline solid UV/Vis.: λmax: 216 nm O Laboratory Procedures For long term storage, we suggest that eltoprazine (hydrochloride) be stored as supplied at -20°C. It should be stable for at least two years. Eltoprazine (hydrochloride) is supplied as a crystalline solid. A stock solution may be made by dissolving the eltoprazine (hydrochloride) in the solvent of choice. Eltoprazine (hydrochloride) is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide, which should be purged with an inert gas. The solubility of eltoprazine (hydrochloride) in these solvents is approximately 25, 20, and 30 mg/ml, respectively. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of eltoprazine (hydrochloride) can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of eltoprazine (hydrochloride) in PBS, pH 7.2, is approximately 1 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Eltoprazine is a phenylpiperazine compound that acts as a partial agonist at serotonin 5-HT1A, 5-HT1B, and 1 5-HT2B receptors (Kis = 40, 52, and 81 nM, respectively). -

( 19 ) United States
USOORE48059E (19 ) United States ( 12 ) Reissued Patent (10 ) Patent Number : US RE48,059 E Yamashita et al. ( 45 ) Date of Reissued Patent: * Jun . 23 , 2020 (54 ) PIPERAZINE -SUBSTITUTED 4,734,416 A 3/1988 Banno et al . BENZOTHIOPHENES FOR TREATMENT OF 4,824,840 A 4/1989 Banno et al. 4,831,031 A 5/1989 Lowe, III et al . MENTAL DISORDERS 4,847,254 A 7/1989 Boegesoe et al . 4,883,795 A 11/1989 Lowe, III et al . ( 71) Applicant: Otsuka Pharmaceutical Co., Ltd., 5,006,528 A 4/1991 Oshiro et al . Tokyo (JP ) 5,424,313 A 6/1995 Hartog et al . 5,436,246 A * 7/1995 Bernotas et al . 514 / 252.13 5,506,248 A 4/1996 Nikfar et al . ( 72 ) Inventors : Hiroshi Yamashita , Tokushima ( JP ) ; 5,753,661 A 5/1998 Moltzen et al. Nobuaki Ito , Tokushima ( JP ) ; Shin 5,846,982 A 12/1998 Audia et al. Miyamura , Tokushima (JP ) ; Kunio 5,919,485 A 7/1999 Cochran et al. Oshima, Tokushima (JP ) ; Jun 5,958,924 A 9/1999 McCort et al . 5,977,110 A 11/1999 Belliotti et al . Matsubara , Tokushima ( JP ) ; Hideaki 6,140,331 A 10/2000 Moltzen et al . Kuroda , Tokushima (JP ) ; Haruka 6,187,340 B1 2/2001 Fukuta et al . Takahashi, Tokushima ( JP ) ; Satoshi 6,214,829 B1 4/2001 Feenstra et al. Shimizu , Tokushima ( JP ) ; Tatsuyoshi 6,225,312 B1 5/2001 Feenstra et al. Tanaka , Tokushima ( JP ) ; Yasuo 6,262,056 B1 7/2001 Monge Vega et al . 6,562,375 B1 5/2003 Sako et al. -

Evaluation of Substituted N-Phenylpiperazine Analogs As D3 Vs
molecules Article Evaluation of Substituted N-Phenylpiperazine Analogs as D3 vs. D2 Dopamine Receptor Subtype Selective Ligands Boeun Lee 1 , Michelle Taylor 2, Suzy A. Griffin 2, Tamara McInnis 2, Nathalie Sumien 2 , Robert H. Mach 1 and Robert R. Luedtke 2,* 1 Department of Radiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104, USA; [email protected] (B.L.); [email protected] (R.H.M.) 2 Department of Pharmacology and Neuroscience, University of North Texas Health Science Center-Fort Worth, Fort Worth, TX 76107, USA; [email protected] (M.T.); suzy.griffi[email protected] (S.A.G.); [email protected] (T.M.); [email protected] (N.S.) * Correspondence: [email protected] Abstract: N-phenylpiperazine analogs can bind selectively to the D3 versus the D2 dopamine receptor subtype despite the fact that these two D2-like dopamine receptor subtypes exhibit substantial amino acid sequence homology. The binding for a number of these receptor subtype selective compounds was found to be consistent with their ability to bind at the D3 dopamine receptor subtype in a bitopic manner. In this study, a series of the 3-thiophenephenyl and 4-thiazolylphenyl fluoride substituted N-phenylpiperazine analogs were evaluated. Compound 6a was found to bind at the human D3 receptor with nanomolar affinity with substantial D3 vs. D2 binding selectivity (approximately 500-fold). Compound 6a was also tested for activity in two in-vivo assays: (1) a hallucinogenic-dependent head twitch response inhibition assay using DBA/2J mice and (2) an Citation: Lee, B.; Taylor, M.; Griffin, L-dopa-dependent abnormal involuntary movement (AIM) inhibition assay using unilateral 6- S.A.; McInnis, T.; Sumien, N.; Mach, 6a R.H.; Luedtke, R.R. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

(12) United States Patent (10) Patent No.: US 9.415,047 B2 Zhou Et Al
US0094.15047B2 (12) United States Patent (10) Patent No.: US 9.415,047 B2 Zhou et al. (45) Date of Patent: Aug. 16, 2016 (54) USE OF BENZO FIVE-MEMBERED 31/4545; A61K 31/506; C07D 209/08; C07D NITROGEN HETEROCYCLIC PPERAZINE 231/56; C07D 235/08; C07D 235/14: CO7D OR PIPERDINEDERVATIVES 235/22; C07D401/06; C07D 401/12 (71) Applicants: Liaoning Emmy Biological USPC ............................................. 514/252.13, 254 Pharmaceutical Co., Ltd., Liaoning See application file for complete search history. (CN); Shenyang Emmy Pharmaceutical Research Institute (56) References Cited Co., Ltd., Liaoning (CN) U.S. PATENT DOCUMENTS (72) Inventors: Yan Zhou, Liaoning (CN): Lirong Zhang, Liaoning (CN); Jie Zhou, 3,362.956 A * 1/1968 Archer ................. CO7D 209/60 Liaoning (CN), Xin Zhou, Liaoning 544,225 3,472,854. A * 10/1969 Archer ................. CO7D 209/60 (CN) 514,906 (73) Assignees: Liaoning Emmy Biological (Continued) Pharmaceutical Co., Ltd., Liaoning (CN); Shenyang Emmy FOREIGN PATENT DOCUMENTS Pharmaceutical Research Institute Co., Ltd., Liaoning (CN) CN 1154693. A 7/1997 CN 1944404 A 4/2007 (*) Notice: Subject to any disclaimer, the term of this CN 101759693. A 6, 2010 patent is extended or adjusted under 35 U.S.C. 154(b) by 0 days. OTHER PUBLICATIONS (21) Appl. No.: 14/647,408 Alessandro Boido et al., “Synthesis and pharmacological evaluation (22) PCT Fled: Nov. 25, 2013 of aryl/heteroaryl piperazinyl alkyl benzotriazoles as ligands for some serotonin and dopamine receptor subtypes.” IL FARMACO, (86) PCT NO.: PCT/CN2O13/OO1442 2001, vol. 56, pp. 263-275.* S371 (c)(1), (Continued) (2) Date: May 26, 2015 (87) PCT Pub. -

Dopamine D3 Receptor Ligands—Recent Advances in the Control of Subtype Selectivity and Intrinsic Activity ⁎ Frank Boeckler A,B, , Peter Gmeiner A
Biochimica et Biophysica Acta 1768 (2007) 871–887 www.elsevier.com/locate/bbamem Review Dopamine D3 receptor ligands—Recent advances in the control of subtype selectivity and intrinsic activity ⁎ Frank Boeckler a,b, , Peter Gmeiner a a Department of Medicinal Chemistry, Emil Fischer Center, Friedrich-Alexander University Erlangen-Nürnberg, Schuhstrasse 19, 91052 Erlangen, Germany b MRC Centre for Protein Engineering, Medical Research Council Centre, Hills Road, Cambridge, CB2 0QH, UK Received 18 July 2006; accepted 4 December 2006 Available online 15 December 2006 Abstract Various pharmacological studies have implicated the dopamine D3 receptor as an interesting therapeutic target in the treatment of different neurological disorders. Because of these putative therapeutic applications, D3 receptor ligands with diverse intrinsic activities have been an active field of research in recent years. Separation of purely D3-mediated drug effects from effects produced by interactions with similar biogenic amine receptors allows to verify the therapeutic impact of D3 receptors and to reduce possible side-effects caused by “promiscuous” receptor interactions. The requirement to gain control of receptor selectivity and in particular subtype selectivity has been a challenging task in rational drug discovery for quite a few years. In this review, recently developed structural classes of D3 ligands are discussed, which cover a broad spectrum of intrinsic activities and show interesting selectivities. © 2006 Elsevier B.V. All rights reserved. Keywords: Dopamine D3 receptor; Agonist; Antagonist; Structure activity relationship; Rational drug discovery; G protein-coupled receptor Contents 1. Introduction.............................................................. 871 2. Homology-based difficulty to gain selectivity among D2-like receptors . ............................ 872 3. Recent progress in controlling subtype selectivity and intrinsic activity of D3 ligands ....................... -

( 12 ) United States Patent
US010493080B2 (12 ) United States Patent (10 ) Patent No.: US 10,493,080 B2 Schultz et al. (45 ) Date of Patent : Dec. 3 , 2019 ( 54 ) DIRECTED DIFFERENTIATION OF (56 ) References Cited OLIGODENDROCYTE PRECURSOR CELLS TO A MYELINATING CELL FATE U.S. PATENT DOCUMENTS 7,301,071 B2 11/2007 Zheng (71 ) Applicants : The Scripps Research Institute , La 7,304,071 B2 12/2007 Cochran et al. Jolla , CA (US ) ; Novartis AG , Basel 9,592,288 B2 3/2017 Schultz et al. 2003/0225072 A1 12/2003 Welsh et al. ( CH ) 2006/0258735 Al 11/2006 Meng et al. 2009/0155207 Al 6/2009 Hariri et al . (72 ) Inventors : Peter Schultz , La Jolla , CA (US ) ; Luke 2010/0189698 A1 7/2010 Willis Lairson , San Diego , CA (US ) ; Vishal 2012/0264719 Al 10/2012 Boulton Deshmukh , La Jolla , CA (US ) ; Costas 2016/0166687 Al 6/2016 Schultz et al. Lyssiotis , Boston , MA (US ) FOREIGN PATENT DOCUMENTS (73 ) Assignees : The Scripps Research Institute , La JP 10-218867 8/1998 Jolla , CA (US ) ; Novartis AG , Basel JP 2008-518896 5/2008 (CH ) JP 2010-533656 A 10/2010 WO 2008/143913 A1 11/2008 WO 2009/068668 Al 6/2009 ( * ) Notice : Subject to any disclaimer , the term of this WO 2009/153291 A1 12/2009 patent is extended or adjusted under 35 WO 2010/075239 Al 7/2010 U.S.C. 154 ( b ) by 0 days . (21 ) Appl. No .: 15 /418,572 OTHER PUBLICATIONS Molin - Holgado et al . “ Regulation of muscarinic receptor function in ( 22 ) Filed : Jan. 27 , 2017 developing oligodendrocytes by agonist exposure ” British Journal of Pharmacology, 2003 , 138 , pp . -

Drug/Substance Trade Name(S)
A B C D E F G H I J K 1 Drug/Substance Trade Name(s) Drug Class Existing Penalty Class Special Notation T1:Doping/Endangerment Level T2: Mismanagement Level Comments Methylenedioxypyrovalerone is a stimulant of the cathinone class which acts as a 3,4-methylenedioxypyprovaleroneMDPV, “bath salts” norepinephrine-dopamine reuptake inhibitor. It was first developed in the 1960s by a team at 1 A Yes A A 2 Boehringer Ingelheim. No 3 Alfentanil Alfenta Narcotic used to control pain and keep patients asleep during surgery. 1 A Yes A No A Aminoxafen, Aminorex is a weight loss stimulant drug. It was withdrawn from the market after it was found Aminorex Aminoxaphen, Apiquel, to cause pulmonary hypertension. 1 A Yes A A 4 McN-742, Menocil No Amphetamine is a potent central nervous system stimulant that is used in the treatment of Amphetamine Speed, Upper 1 A Yes A A 5 attention deficit hyperactivity disorder, narcolepsy, and obesity. No Anileridine is a synthetic analgesic drug and is a member of the piperidine class of analgesic Anileridine Leritine 1 A Yes A A 6 agents developed by Merck & Co. in the 1950s. No Dopamine promoter used to treat loss of muscle movement control caused by Parkinson's Apomorphine Apokyn, Ixense 1 A Yes A A 7 disease. No Recreational drug with euphoriant and stimulant properties. The effects produced by BZP are comparable to those produced by amphetamine. It is often claimed that BZP was originally Benzylpiperazine BZP 1 A Yes A A synthesized as a potential antihelminthic (anti-parasitic) agent for use in farm animals.