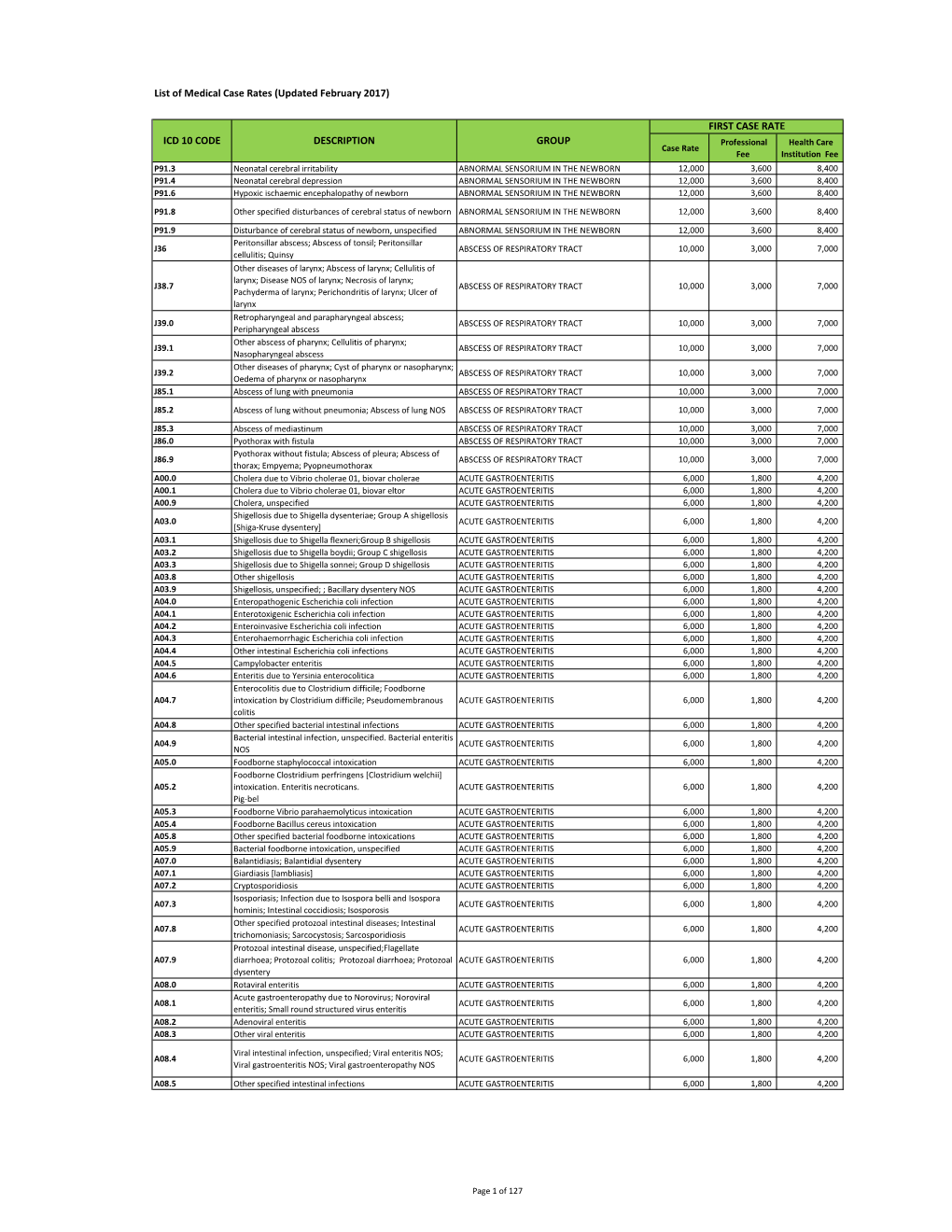
Annexa-Medicalcaserates
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peptic Ulcer Disease
Peptic Ulcer Disease orking with you as a partner in health care, your gastroenterologist Wat GI Associates will determine the best diagnostic and treatment measures for your unique needs. Albert F. Chiemprabha, M.D. Pierce D. Dotherow, M.D. Reed B. Hogan, M.D. James H. Johnston, III, M.D. Ronald P. Kotfila, M.D. Billy W. Long, M.D. Paul B. Milner, M.D. Michelle A. Petro, M.D. Vonda Reeves-Darby, M.D. Matt Runnels, M.D. James Q. Sones, II, M.D. April Ulmer, M.D., Pediatric GI James A. Underwood, Jr., M.D. Chad Wigington, D.O. Mark E. Wilson, M.D. Cindy Haden Wright, M.D. Keith Brown, M.D., Pathologist Samuel Hensley, M.D., Pathologist Jackson Madison Vicksburg 1421 N. State Street, Ste 203 104 Highland Way 1815 Mission 66 Jackson, MS 39202 Madison, MS 39110 Vicksburg, MS 39180 Telephone 601/355-1234 • Fax 601/352-4882 • 800/880-1231 www.msgastrodocs.com ©2010 GI Associates & Endoscopy Center. All rights reserved. A discovery that Table of contents brought relief to millions of ulcer What Is Peptic Ulcer Disease............... 2 patients...... Three Major Types Of Peptic Ulcer Disease .. 6 The bacterium now implicated as a cause of some ulcers How Are Ulcers Treated................... 9 was not noticed in the stomach until 1981. Before that, it was thought that bacteria couldn’t survive in the stomach because Questions & Answers About Peptic Ulcers .. 11 of the presence of acid. Australian pathologists, Drs. Warren and Marshall found differently when they noticed bacteria Ulcers Can Be Stubborn................... 13 while microscopically inspecting biopsies from stomach tissue. -

An Unusual Case of Amoebic Liver Abscess Presenting with Hepatic Encephalopathy: a Case Report
Case Report An Unusual Case of Amoebic Liver Abscess Presenting with Hepatic Encephalopathy: A Case Report Anil Kumar SARDA, Rakesh MITTAL Submitted: 16 Sep 2010 Department of Surgery, Maulana Azad Medical College and Lok Nayak Accepted: 3 Jan 2011 Hospital, New Delhi 110 002, India Abstract Amoebic liver abscess (ALA) with jaundice and encephalopathy is a rare occurrence and has been recognised and studied more frequently in recent years. We present a case of massive ALA presenting with jaundice, hepatic encephalopathy, and septicaemia that was treated successfully with percutaneous drainage of the abscess, right-sided chest tube insertion, and anti-amoebic therapy. Keywords: amoebiasis, hepatic encephalopathy, hepatology, jaundice, liver abscess Introduction On chest examination, there was bilateral equal air entry. Upon investigation, haemoglobin was Amoebic liver abscess (ALA) is the most 11 g/dL, with a total leukocyte count of frequent extra-intestinal manifestation of 13 000 cells/mm3 (normal range is 4000– Entamoeba histolytica infection. It has been 11 000 cells/mm3). Liver function tests revealed reported that jaundice is uncommon and mild total serum bilirubin of 20 mg/dL, with direct in liver abscess, and some even consider the bilirubin of 15 mg/dL, serum glutamic-oxaloacetic presence of jaundice as a feature against the transaminase (SGOT) of 324 IU/L (normal level diagnosis of hepatic amoebiasis (1). The cause of is less than 40 IU/L), serum glutamic–pyruvic jaundice in a case of ALA has been hypothesised transaminase (SGPT) of 340 IU/L (normal level to result from either hepatocellular dysfunction or is less than 40 IU/L), and alkaline phosphatase intrahepatic biliary obstruction (2). -

Cholestasis Inamoebic Liver Abscess
Gut: first published as 10.1136/gut.26.2.140 on 1 February 1985. Downloaded from Gut, 1985, 26, 140-145 Cholestasis in amoebic liver abscess P NIGAM, A K GUPTA, K K KAPOOR, G R SHARAN, B M GOYAL, AND L D JOSHI From the Department ofMedicine, BRD Medical College, Gorakhpur, India, the Department of Tubercolosis and Chest Diseases, and the Department ofBiochemistry, MLB Medical College, Jhansi, India SUMMARY Two hundred and thirty six patients with amoebic liver abscess were investigated for cholestasis, its mechanism and the natural course of the disease. Cholestasis was seen in 29% of cases and it presented with some unusual features: it was frequently seen in young men (mean age 38-6±6-3 years) (87%) with acute onset (69%) and was associated with signs of peritonism, or peritonitis (28%), splenomegaly (12%) and hepatic encephalopathy (coma 13%). Raised diaphragm was seen only in 37% of cases. Alcoholism may have contributed to the cholestasis in 37% of cases. Multiple (43%) and single (32%) large liver abscesses, especially on the inferior surface of the liver (25%), were common in jaundiced patients with amoebic liver abscess, while size and number of abscesses were directly related to the raised serum bilirubin concentrations. Bromsulphalein excretion (BSP) was found to be significantly reduced (p<001) in patients with jaundice (60%). Retrograde injection of contrast media into the common bile duct during six necropsies showed compression by amoebic liver abscess on the hepatic ducts. The mortality (43%) and the complications were significantly higher (p<0.001) in patients with jaundice. The aspiration/surgical drainage of amoebic liver abscess together with a combination of metronidazole and di-iodohydroxyquinoline was more effective than either metronidazole alone, or dehydroemetine with chloroquine. -

Original Article
Tropical Gastroenterology 2013;34(2):83–86 Original Colonic perforation with peritonitis in amoebiasis: A Article tropical disease with high mortality Bhupendra Kumar Jain1, Pankaj Kumar Garg1, Anjay Kumar1, Kiran Mishra2, Debajyoti Mohanty1, Vivek Agrawal1 ABSTRACT Department of Surgery1 and Background: Invasive colonic amoebiasis presents primarily with dysentery; colonic Pathology2, University College of perforation occurs rarely. Cases of amoebic colonic perforations have been reported Medical Sciences and Guru Teg sporadically over the past 20 years. Bahadur Hospital, University of Delhi, India Methods: A retrospective study was done in the surgical unit of a tertiary care hospital in North India. The case records of those patients were reviewed who underwent exploratory Correspondence: laparotomy from January 2011 to September 2012 and were diagnosed with amoebic colonic Dr. Bhupendra Kumar Jain perforation on histopathological examination. Details concerning the clinical presentation, Email [email protected] investigations, intraoperative findings, operative procedures, and postoperative outcomes were retrieved. Results: Amongst, a total of 186 emergency exploratory laparotomies carried out during the study , 15 patients of amoebic colonic perforation were identified. The median age of the patients was 42 years (IQR 32.0–58.0) and the male to female ratio was 13:2. Previous history of colitis was present in only 1 patient. The preoperative diagnosis was perforation peritonitis in 12 patients; and intussusception, intestinal obstruction and ruptured liver abscess in 1 patient each. Ten patients had single perforation while 5 had multiple colonic perforations. All the patients except one had perforations in the right colon. Bowel resection was performed depending upon the site and extent of the colon involved—right hemicolectomy (8), limited ileocolic resection (6) and sigmoidectomy (1). -

Eosinophilic Cellulitis (Wells Syndrome): a Case Report
International Journal of Research in Dermatology Baabdullah AM et al. Int J Res Dermatol. 2021 May;7(3):450-453 http://www.ijord.com DOI: https://dx.doi.org/10.18203/issn.2455-4529.IntJResDermatol20211708 Case Report Eosinophilic cellulitis (wells syndrome): a case report Ahmad Mohammad Baabdullah1, Khalid Ali Al Hawsawi2, Bashayr Saad Alhubayshi3*, Marwa Rashed Gammash4 1Department of Dermatology, King Abdulaziz University Hospital, Jeddah, Saudi Arabia 2 Department of Dermatology, King Faisal Specialist Hospital and Research Centre, Jeddah, Saudi Arabia 3Taibah College of Medicine, Taibah University, Almadinah Almunawwarah, Saudi Arabia 4Collage of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia Received: 14 January 2021 Accepted: 08 February 2021 *Correspondence: Dr. Bashayr Saad Alhubayshi, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Eosinophilic Cellulitis is also known as Wells syndrome is uncommon dermatitis, characterized by the infiltration of eosinophils in the dermis. The exact etiology of the disease is unknown. Clinically, it is highly varied but commonly the presentation is pruritic erythematous plaque. We report a case of one and half years old healthy boy who developed itchy bullae on the dorsum of his hand with multiple erythematous papules over his extremities that started immediately after his vaccines. Histopathological examination of the lesion showed infiltrate eosinophils with typical flame figures. The case was successfully treated with corticosteroid course. -

Acral Manifestations of Soft Tissue Tumors Kristen M
Clinics in Dermatology (2017) 35,85–98 Acral manifestations of soft tissue tumors Kristen M. Paral, MD, Vesna Petronic-Rosic, MD, MSc⁎ Section of Dermatology, University of Chicago Pritzker School of Medicine, Chicago, IL Abstract This group of biologically diverse entities is united by topographic localization to the hands and feet. Categorizing tumors by body site narrows the differential into a short list of possibilities that can facil- itate accurate and rapid diagnosis. The goal of this review is to provide a practical approach to soft tissue tumors of acral locations for clinicians, pathologists, and researchers alike. What ensues in the following text is that tight coupling of the clinical picture and histopathologic findings should produce the correct diagno- sis, or at least an abbreviated differential. The salient clinicopathologic, immunohistochemical, and molec- ular features are presented alongside current treatment recommendations for each entity. © 2017 Elsevier Inc. All rights reserved. Introduction actin (SMA) and are deemed “myofibroblasts.”1 The tumors under this heading express combinations of CD34, FXIIIa, fi The entities presented herein are categorized on the basis of and SMA. The synthesis of collagen by broblasts translates fi fi morphogenesis (where possible) and by biologic potential as to a brous consistency that clinically imparts a rm texture benign, intermediate, and malignant neoplasms. on palpation, and, macroscopically, a gray-white or white-tan cut surface. The entities discussed next have no metastatic po- tential; that is, simple excision is adequate. Fibrous and related tissues: Benign lesions Fibroma of tendon sheath fi fl The ontogenetic classi cation of benign lesions re ects appar- Also known as tenosynovial fibroma, compared with other fi fi fi ent broblastic or broblast-like morphogenesis. -

Ultrasound of Tropical Medicine Parasitic Diseases of the Liver
Ultrasound of the liver …. 20.11.2012 11:05 1 EFSUMB – European Course Book Editor: Christoph F. Dietrich Ultrasound of Tropical Medicine Parasitic diseases of the liver Enrico Brunetti1, Tom Heller2, Francesca Tamarozzi3, Adnan Kabaalioglu4, Maria Teresa Giordani5, Joachim Richter6, Roberto Chiavaroli7, Sam Goblirsch8, Carmen Cretu9, Christoph F Dietrich10 1 Department of Infectious Diseases, San Matteo Hospital Foundation- University of Pavia, Pavia, Italy 2 Department of Internal Medicine, Klinikum Muenchen Perlach, Munich, Germany 3 Department of Infectious Diseases, San Matteo Hospital Foundation- University of Pavia, Pavia, Italy 4 Department of Radiology, Akdeniz University, Antalya, Turkey 5 Infectious and Tropical Diseases Unit, San Bortolo Hospital, Vicenza, Italy 6 Tropenmedizinische Ambulanz, Klinik für Gastroenterologie, Hepatologie und Infektiologie, Heinrich-Heine-Universität, Düsseldorf, Germany 7 Infectious Diseases Unit, Santa Caterina Novella Hospital, Galatina, Italy 8 Department of Medicine and Pediatrics, University of Minnesota, Minneapolis, MN, USA 9 University of Medicine and Pharmacy "Carol Davila" Parasitology Department Colentina Teaching Hospital, Bucharest, Romania 10 Caritas-Krankenhaus Bad Mergentheim, Germany Ultrasound of parasitic disease …. 20.11.2012 11:05 2 Content Content ....................................................................................................................................... 2 Amoebiasis ................................................................................................................................ -

Learning Points from a Case of Severe Amoebic Colitis
Le Infezioni in Medicina, n. 3, 281-284, 2017 CASE REPORT 281 Learning points from a case of severe amoebic colitis Christina Petridou1, Adnan Al-Badri2, Anjana Dua1, Matthew Dryden1, Kordo Saeed1 1Microbiology Department, Hampshire Hospitals NHS Foundation Trust, Royal Hampshire County Hospital, Winchester, United Kingdom; 2Pathology Department, Hampshire Hospitals NHS Foundation Trust, Royal Hampshire County Hospital, United Kingdom SUMMARY A case of amoebic colitis and liver abscess is described learning points including the importance of taking a in a previously fit 59-year old man who had been given lifelong travel history, the difficulties in telling ulcer- the incorrect diagnosis of ulcerative colitis. His symp- ative colitis and amoebic colitis apart both clinically toms were so severe that a colectomy was being con- and histopathologically, and the importance of send- sidered. The patient had a significant travel history in- ing multiple stool samples for parasitological micros- cluding trips to Morocco, the Gambia and Cape Verde, copy analysis in patients being investigated for inflam- putting him at risk of acquiring amoebic disease. How- matory bowel disease. ever, this history was not ascertained until much later on in the disease process. The case highlighted crucial Keywords: amoebic colitis, liver abscess. n CASE REPORT 8 times a day, his inflammatory markers were markedly raised and he had deranged liver func- 59-year-old man was admitted to Royal tion tests with a C-reactive protein of 263 mg/L, a white cell count of 25.6 109/L, an ALT of 102 U/L A Hampshire County Hospital, a district gener- al hospital in the United Kingdom, directly from and an ALP of 336 U/L. -

Active Peptic Ulcer Disease in Patients with Hepatitis C Virus-Related Cirrhosis: the Role of Helicobacter Pylori Infection and Portal Hypertensive Gastropathy
dore.qxd 7/19/2004 11:24 AM Page 521 View metadata, citation and similar papers at core.ac.uk ORIGINAL ARTICLE brought to you by CORE provided by Crossref Active peptic ulcer disease in patients with hepatitis C virus-related cirrhosis: The role of Helicobacter pylori infection and portal hypertensive gastropathy Maria Pina Dore MD PhD, Daniela Mura MD, Stefania Deledda MD, Emmanouil Maragkoudakis MD, Antonella Pironti MD, Giuseppe Realdi MD MP Dore, D Mura, S Deledda, E Maragkoudakis, Ulcère gastroduodénal évolutif chez les A Pironti, G Realdi. Active peptic ulcer disease in patients patients atteints de cirrhose liée au HCV : Le with hepatitis C virus-related cirrhosis: The role of Helicobacter pylori infection and portal hypertensive rôle de l’infection à Helicobacter pylori et de la gastropathy. Can J Gastroenterol 2004;18(8):521-524. gastropathie liée à l’hypertension portale BACKGROUND & AIM: The relationship between Helicobacter HISTORIQUE ET BUT : Le lien entre l’infection à Helicobacter pylori pylori infection and peptic ulcer disease in cirrhosis remains contro- et l’ulcère gastroduodénal dans la cirrhose reste controversé. Le but de la versial. The purpose of the present study was to investigate the role of présente étude est de vérifier le rôle de l’infection à H. pylori et de la gas- H pylori infection and portal hypertension gastropathy in the preva- tropathie liée à l’hypertension portale dans la prévalence de l’ulcère gas- lence of active peptic ulcer among dyspeptic patients with compen- troduodénal évolutif chez les patients dyspeptiques souffrant d’une sated hepatitis C virus (HCV)-related cirrhosis. -
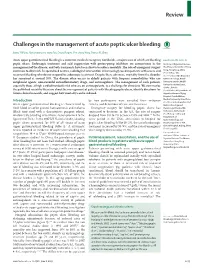
Challenges in the Management of Acute Peptic Ulcer Bleeding
Review Challenges in the management of acute peptic ulcer bleeding James Y W Lau, Alan Barkun, Dai-ming Fan, Ernst J Kuipers, Yun-sheng Yang, Francis K L Chan Acute upper gastrointestinal bleeding is a common medical emergency worldwide, a major cause of which are bleeding Lancet 2013; 381: 2033–43 peptic ulcers. Endoscopic treatment and acid suppression with proton-pump inhibitors are cornerstones in the Institute of Digestive Diseases, management of the disease, and both treatments have been shown to reduce mortality. The role of emergency surgery The Chinese University of Hong continues to diminish. In specialised centres, radiological intervention is increasingly used in patients with severe and Kong, Hong Kong, China (Prof J Y W Lau MD, recurrent bleeding who do not respond to endoscopic treatment. Despite these advances, mortality from the disorder Prof F K L Chan MD); Division of has remained at around 10%. The disease often occurs in elderly patients with frequent comorbidities who use Gastroenterology, McGill antiplatelet agents, non-steroidal anti-infl ammatory drugs, and anticoagulants. The management of such patients, University and the McGill especially those at high cardiothrombotic risk who are on anticoagulants, is a challenge for clinicians. We summarise University Health Centre, Quebec, Canada the published scientifi c literature about the management of patients with bleeding peptic ulcers, identify directions for (Prof A Barkun MD); Institute of future clinical research, and suggest how mortality can be reduced. Digestive Diseases, Xijing Hospital, Fourth Military Introduction by how participants were sampled, their inclusion Medical University, Xian, China (Prof D Fan MD); Department of Acute upper gastrointestinal bleeding is characterised by criteria, and defi nitions of case ascertainment. -

Pathology and Genetics of Tumours of Soft Tissue and Bone
bb5_1.qxd 13.9.2006 14:05 Page 3 World Health Organization Classification of Tumours WHO OMS International Agency for Research on Cancer (IARC) Pathology and Genetics of Tumours of Soft Tissue and Bone Edited by Christopher D.M. Fletcher K. Krishnan Unni Fredrik Mertens IARCPress Lyon, 2002 bb5_1.qxd 13.9.2006 14:05 Page 4 World Health Organization Classification of Tumours Series Editors Paul Kleihues, M.D. Leslie H. Sobin, M.D. Pathology and Genetics of Tumours of Soft Tissue and Bone Editors Christopher D.M. Fletcher, M.D. K. Krishnan Unni, M.D. Fredrik Mertens, M.D. Coordinating Editor Wojciech Biernat, M.D. Layout Lauren A. Hunter Illustrations Lauren A. Hunter Georges Mollon Printed by LIPS 69009 Lyon, France Publisher IARCPress International Agency for Research on Cancer (IARC) 69008 Lyon, France bb5_1.qxd 13.9.2006 14:05 Page 5 This volume was produced in collaboration with the International Academy of Pathology (IAP) The WHO Classification of Tumours of Soft Tissue and Bone presented in this book reflects the views of a Working Group that convened for an Editorial and Consensus Conference in Lyon, France, April 24-28, 2002. Members of the Working Group are indicated in the List of Contributors on page 369. bb5_1.qxd 22.9.2006 9:03 Page 6 Published by IARC Press, International Agency for Research on Cancer, 150 cours Albert Thomas, F-69008 Lyon, France © International Agency for Research on Cancer, 2002, reprinted 2006 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. -

An Overview: Current Clinical Guidelines for the Evaluation, Diagnosis, Treatment, and Management of Dyspepsia$
Osteopathic Family Physician (2013) 5, 79–85 An overview: Current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia$ Peter Zajac, DO, FACOFP, Abigail Holbrook, OMS IV, Maria E. Super, OMS IV, Manuel Vogt, OMS IV From University of Pikeville-Kentucky College of Osteopathic Medicine (UP-KYCOM), Pikeville, KY. KEYWORDS: Dyspeptic symptoms are very common in the general population. Expert consensus has proposed to Dyspepsia; define dyspepsia as pain or discomfort centered in the upper abdomen. The more common causes of Functional dyspepsia dyspepsia include peptic ulcer disease, gastritis, and gastroesophageal reflux disease.4 At some point in (FD); life most individuals will experience some sort of transient epigastric pain. This paper will provide an Gastritis; overview of the current guidelines for the evaluation, diagnosis, treatment, and management of Gastroesophageal dyspepsia in a clinical setting. reflux disease (GERD); r 2013 Elsevier Ltd All rights reserved. Nonulcer dyspepsia (NUD); Osteopathic manipulative medicine (OMM); Peptic ulcer disease (PUD); Somatic dysfunction Dyspeptic symptoms are very common in the general common causes of dyspepsia include peptic ulcer disease population, affecting an estimated 20% of persons in the (PUD), gastritis, and gastroesophageal reflux disease United States.1 While a good number of these individuals (GERD).4 However, it is not unusual for a complete may never seek medical care, a significant proportion will investigation to fail to reveal significant organic findings, eventually proceed to see their family physician. Several and the patient is then considered to have “functional reports exist on the prevalence and impact of dyspepsia in the dyspepsia.”5,6 The term “functional” is usually applied to general population.2,3 However, the results of these studies disorders or syndromes where the body’s normal activities in are strongly influenced by criteria used to define dyspepsia.