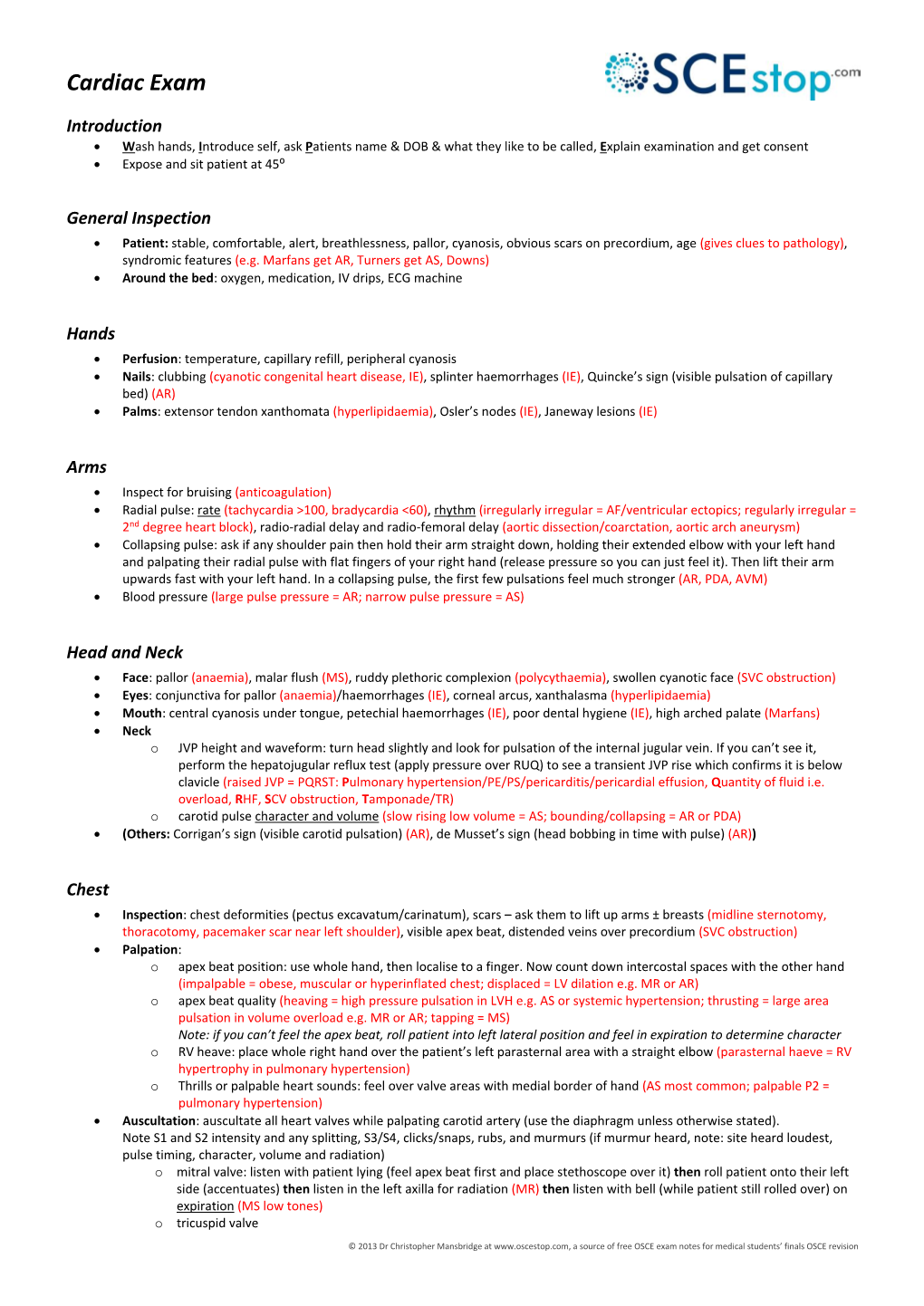
Cardiac Exam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1. Intermittent Chest Pain: Angina: • Stable: (Caused By
CVS: 1. Intermittent chest pain: Angina: • Stable: (caused by chronic narrowing in one or more coronary arteries), episodes of pain are precipitated by exertion and may occur more readily when walking in cold or windy weather, after a large meal or while carrying a heavy load; the pain is promptly relieved by rest and/or sublingual glyceryl nitrate (GTN) spray, and typically lasts for less than 10 minutes. • unstable angina (caused by a sudden severe narrowing in a coronary artery), there is usually an abrupt onset or worsening of chest pain episodes that may occur on minimal exertion or at rest. • Retrosternal/ Progressive onset/ increase in intensity over 1–2 minutes/ Constricting, heavy/ Sometimes arm(s), neck, epigastrium/ Associated with breathlessness/ Intermittent, with episodes lasting 2–10 minutes/ Triggered by emotion, exertion, especially if cold, windy/ Relieved by rest, nitrates Mild to moderate. • Aggravated by thyroxine or drug-induced anemia, e.g. aspirin or NSAIDs Esophageal: • Retrosternal or epigastric/ Over 1–2 minutes; can be sudden (spasm)/ C: Gripping, tight or burning/ R: Often to back, sometimes to arms/ A: Heartburn, acid reflux/ T: Intermittent, often at night-time; variable duration/ Lying flat/some foods may trigger/ Not relieved by rest; nitrates sometimes relieve/ Usually mild but esophageal spasm can mimic myocardial infarction. 2. Acute chest pain: MI: • SOCRATES: Retrosternal/ Rapid over a few minutes/ Constricting, heavy/ Often to arm(s), neck, jaw, sometimes epigastrium/ Sweating, nausea, vomiting, breathlessness, feeling of impending death (angor animi)/ Acute presentation; prolonged duration/ ’Stress’ and exercise rare triggers, usually spontaneous/ Not relieved by rest or nitrates/ Usually severe. -

Scoliosis, Alters the Position of the Beat
Br Heart J: first published as 10.1136/hrt.8.3.162 on 1 July 1946. Downloaded from THE HEART IN STERNAL DEPRESSION BY WILLIAM EVANS From the Cardiac Department ofthe London Hospital Received June 25, 1946 The place where the apex beat appears on the chest wall depends as much on the symmetry of the thorax as on the size of the heart. A change in the alignment of the spine, the posterior fulcrum of the thoracic cage, in the form of scoliosis, alters the position of the beat. Local deformity of the ribs which form the walls of the cage will do the same thing. Deformity of the sternum, the anterior fulcrum of the thorax, as a cause of displacement of the apex beat has received less attention. The effects of depression of the sternum (pectus excavatum) on the shape and position of the heart have been studied in sixteen adults examined during the past year. DESCRIPTION OF CASES All sixteen patients had been referred for an explanation of certain signs connected with the heart, with the knowledge that deformity of the chest was present, but without appreciating that the two conditions might be related. In many of them suspicion of heart disease had led to restriction of their physical activities and to a change of design for their future livelihood. The symptoms that had caused the patients to seek medical advice in the first place were http://heart.bmj.com/ TABLE I SUMMARY OF FINDNGS IN 16 HEALTHY SUBJECTS WITH DEPRESSED STERNUM Antero-posterior Radiological findings in anterior view chest measurement _ _ Case Age Sternal in inches No. -

5 Precordial Pulsations
Chapter 5 / Precordial Pulsations 113 5 Precordial Pulsations CONTENTS MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE PHYSICAL PRINCIPLES GOVERNING THE FORMATION OF THE APICAL IMPULSE NORMAL APICAL IMPULSE AND ITS DETERMINANTS ASSESSMENT OF THE APICAL IMPULSE LEFT PARASTERNAL AND STERNAL MOVEMENTS RIGHT PARASTERNAL MOVEMENT PULSATIONS OVER THE CLAVICULAR HEADS PULSATIONS OVER THE SECOND AND/OR THIRD LEFT INTERCOSTAL SPACES SUBXIPHOID IMPULSE PRACTICAL POINTS IN THE CLINICAL ASSESSMENT OF PRECORDIAL PULSATIONS REFERENCES In this chapter the pulsations of the precordium will be discussed in relation to their identification, the mechanisms of their origin, and their pathophysiological and clinical significance. Precordial pulsations include the “apical impulse,” left parasternal movement, right parasternal movement, pulsations of the clavicular heads, pulsations over the second left intercostal space, and subxiphoid impulses. MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE Since during systole the heart contracts, becoming smaller and therefore moving away from the chest wall, why should one feel a systolic outward movement (the apical impulse) at all? Logically speaking there should not be an apical impulse. Several different methods of recording the precordial motion have been used to study the apical impulse going back to the late 19th century (1,2). Among the more modern methods, the notable ones are the recordings of the apexcardiogram (3–17), the impulse cardiogram (18), and the kinetocardiogram (19–21). While apexcardiography records the relative displacement of the chest wall under the transducer pickup device, which is often held by the examiner’s hands, the proponents of the impulse cardiography and kinetocardiography point out that these methods allow the recording of the absolute movement of the chest wall because the pickup device is anchored to a fixed point held 113 114 Cardiac Physical Examination in space away from the chest. -

CARDIOLOGY Section Editors: Dr
2 CARDIOLOGY Section Editors: Dr. Mustafa Toma and Dr. Jason Andrade Aortic Dissection DIFFERENTIAL DIAGNOSIS PATHOPHYSIOLOGY (CONT’D) CARDIAC DEBAKEY—I ¼ ascending and at least aortic arch, MYOCARDIAL—myocardial infarction, angina II ¼ ascending only, III ¼ originates in descending VALVULAR—aortic stenosis, aortic regurgitation and extends proximally or distally PERICARDIAL—pericarditis RISK FACTORS VASCULAR—aortic dissection COMMON—hypertension, age, male RESPIRATORY VASCULITIS—Takayasu arteritis, giant cell arteritis, PARENCHYMAL—pneumonia, cancer rheumatoid arthritis, syphilitic aortitis PLEURAL—pneumothorax, pneumomediasti- COLLAGEN DISORDERS—Marfan syndrome, Ehlers– num, pleural effusion, pleuritis Danlos syndrome, cystic medial necrosis VASCULAR—pulmonary embolism, pulmonary VALVULAR—bicuspid aortic valve, aortic coarcta- hypertension tion, Turner syndrome, aortic valve replacement GI—esophagitis, esophageal cancer, GERD, peptic OTHERS—cocaine, trauma ulcer disease, Boerhaave’s, cholecystitis, pancreatitis CLINICAL FEATURES OTHERS—musculoskeletal, shingles, anxiety RATIONAL CLINICAL EXAMINATION SERIES: DOES THIS PATIENT HAVE AN ACUTE THORACIC PATHOPHYSIOLOGY AORTIC DISSECTION? ANATOMY—layers of aorta include intima, media, LR+ LRÀ and adventitia. Majority of tears found in ascending History aorta right lateral wall where the greatest shear force Hypertension 1.6 0.5 upon the artery wall is produced Sudden chest pain 1.6 0.3 AORTIC TEAR AND EXTENSION—aortic tear may Tearing or ripping pain 1.2–10.8 0.4–0.99 produce -

Cardiology 1
Cardiology 1 SINGLE BEST ANSWER (SBA) a. Sick sinus syndrome b. First-degree AV block QUESTIONS c. Mobitz type 1 block d. Mobitz type 2 block 1. A 19-year-old university rower presents for the pre- e. Complete heart block Oxford–Cambridge boat race medical evaluation. He is healthy and has no significant medical history. 5. A 28-year-old man with no past medical history However, his brother died suddenly during football and not on medications presents to the emergency practice at age 15. Which one of the following is the department with palpitations for several hours and most likely cause of the brother’s death? was found to have supraventricular tachycardia. a. Aortic stenosis Carotid massage was attempted without success. b. Congenital long QT syndrome What is the treatment of choice to stop the attack? c. Congenital short QT syndrome a. Intravenous (IV) lignocaine d. Hypertrophic cardiomyopathy (HCM) b. IV digoxin e. Wolff–Parkinson–White syndrome c. IV amiodarone d. IV adenosine 2. A 65-year-old man presents to the heart failure e. IV quinidine outpatient clinic with increased shortness of breath and swollen ankles. On examination his pulse was 6. A 75-year-old cigarette smoker with known ischaemic 100 beats/min, blood pressure 100/60 mmHg heart disease and a history of cardiac failure presents and jugular venous pressure (JVP) 10 cm water. + to the emergency department with a 6-hour history of The patient currently takes furosemide 40 mg BD, increasing dyspnoea. His ECG shows a narrow complex spironolactone 12.5 mg, bisoprolol 2.5 mg OD and regular tachycardia with a rate of 160 beats/min. -

Ministry of Health of Ukraine Kharkiv National Medical University
Ministry of Health of Ukraine Kharkiv National Medical University PHYSICAL METHODS OF CARDIOVASCULAR SYSTEM EXAMINATION. INQUIRY AND GENERAL INSPECTION OF THE PATIENTS WITH CARDIOVASCULAR PATHOLOGY. INSPECTION AND PALPATION OF PRECORDIAL AREA Methodical instructions for students Рекомендовано Ученым советом ХНМУ Протокол №__от_______2017 г. Kharkiv KhNMU 2017 Physical methods of cardiovascular system examination. Inquiry and general inspection of the patients with cardiovascular pathology. Inspection and palpation of precordial area / Authors: Т.V. Ashcheulova, O.M. Kovalyova, O.V. Honchar. – Kharkiv: KhNMU, 2016. – 16 с. Authors: Т.V. Ashcheulova O.M. Kovalyova O.V. Honchar INQUIRY OF A PATIENT WITH CARDIOVASCULAR PATHOLOGY The main complaints in patients with cardiovascular disease include: 1. Dyspnea, asthma attacks 2. Pain in the heart region 3. Palpitations 4. Intermissions of heart beats 5. Swelling of the lower extremities and accumulation of fluid in cavities 6. Cough, hemoptysis 7. Dyspepsia 8. Asthenovegetative disorders: weakness, fatigue, decline in performance Dyspnea is a painful feeling of lack of air, one of the symptoms of heart failure, predominantly is of inspiratory type and can be associated with physical activity (in the early stages of compensation) or occur at rest (a sign of severe cardiac decompensation). It is a compensatory responsive activation of the respiratory center in case of congestion and decreased blood flow in larger and small circulation due to reduced myocardial contractility. Dyspnea is typical for heart failure on the background of valvular heart disease (especially mitral valve pathology), ischemic heart disease (angina pectoris, myocardial infarction, cardiosclerosis, arrhythmias and heart blockages), essential and symptomatic hypertension (due to chronic kidney disease, pheochromocytoma, Cushing's disease, primary aldosteronism etc.). -

The Cardiovascular Examination
CHAPTER 1 The Cardiovascular Examination KEY POINTS • The cardiovascular examination lends itself to a systematic approach. • The examination should be thorough but should be directed by the history to areas likely to be relevant. • Certain cardiovascular signs are quite sensitive and specific. • When the examination is well performed, many unnecessary investigations can be avoided. CASE 1 SCENARIO: TARA WITH 3. Pick up the patient’s hand. Feel the radial pulse. DYSPNOEA Inspect the patient’s hands for clubbing. Demon- strate Schamroth’s sign (Fig. 1.1). If there is no 34-year-old Tara was referred to the hospital by her general clubbing, opposition of the index finger (nail to practitioner. She presented with increasing dyspnoea for the nail) demonstrates a diamond shape; in clubbing last 2 weeks. She has found it difficult to lie flat in bed and this space is lost. Also look for the peripheral has been waking up frequently feeling breathless. She also stigmata of infective endocarditis. Splinter haemor- has a dry cough and has felt extremely tired for weeks. She rhages are common (and are usually caused by also has high fever with a shake. She is an intravenous drug trauma), whereas Osler’s nodes and Janeway lesions user and her general practitioner (GP) found a loud murmur (Fig. 1.2) are rare. Look quickly, but carefully, at on auscultation. each nail bed, otherwise it is easy to miss key signs. Please examine the cardiovascular system. Note the presence of an intravenous cannula and, if an infusion is running, look at the bag to see The cardiovascular system should be examined in what it is. -
Guide to History Taking and Examination
MBBS Year 4 GUIDE TO HISTORY TAKING AND EXAMINATION 2015-16 Copyright University College London Medical School University College London 1 Contents The Medical History ................................................................................ 3 How to take a Respiratory History ..................................................... 12 How to take a Cardiovascular History ............................................... 13 How to take a Locomotor History ....................................................... 14 How to take a history of pain ............................................................... 14 Presenting patients Workshop ............................................................. 15 General Tips on How to Perform an Examination ........................... 16 Dress and Behaviour Expected in Clinical Area ............................... 18 Cardiovascular Examination ................................................................ 19 Respiratory Examination ...................................................................... 24 Abdominal Examination ....................................................................... 26 Musculoskeletal Examination- GALS Screen ................................... 30 Motor Examination of Lower Limbs ................................................... 32 Examination of the Upper Limbs ........................................................ 35 Sensory Examination of Lower Limbs ................................................ 38 Cranial Nerve Examination ................................................................. -

MB Chb Clinical History and Examination Manual
MB ChB Clinical History and Examination Manual This is derived from the “Green Book”, a typewritten aide memoire for clinical examination well known to all Glasgow graduates. It is intended as an aid to learning clinical history taking and examination, specifically in Phase 3 of the MB ChB curriculum - the first 15 weeks of Year 3. During that time, students will spend one full day per week in hospital or in General Practice. The hospital session should involve: (a) a session of bedside teaching, involving history taking and examination; (b) a case (either alone or in pairs) which should then be hand-written in the format at the end of this booklet; (c) presentation and discussion of the cases as a group. For the first few sessions it is expected that only parts of the history and examination will be covered but by the end of Year 3 all students should be proficient. Additional sections cover history-taking in psychiatry, obstetrics and gynaecology that are relevant later in the MB ChB programme. 3 Index Introduction 5 The Abdominal Systems (GIS, 33 The Patient’s problem 5 GUS and Haematological) The Doctor’s problem 6 The Nervous System 37 History 8 History & Examination in 43 Joint Disease History of Presenting 9 Complaint (HPC) Examination of the Patient 45 with a Skin Complaint Cardiovascular System 10 Summary Plan for Taking 46 Respiratory System 11 History and Physical Examination in the Adult Gastrointestinal System 12 Physical Examination:- 48 Genitourinary System:- 15 Cardiovascular System For Females Respiratory System For Males -

Three-Dimensional Apex-Seismocardiography
Three-Dimensional Apex-Seismocardiography Samuel E Schmidt, Ask S Jensen, Jacob Melgaard, Claus Graff, John Hansen, Tanveer A Bhuiyan, Johannes J Struijk Department of Health Science and Technology Aalborg University, Aalborg, Denmark Abstract family of cardiac vibration quantification technologies like phonocardiography and Ballistocardiography, which Traditional apex-cardiography measures chest wall all had their golden age before the emergence of vibrations at the apex beat using an air-coupled echocardiography. However, modern electronics as microphone. To provide additional insight in apex- microprocessors, tablets and advanced signal cardiography and chest vibrations we estimated the three processing/classification might make these technologies dimensional displacement of the apex beat. very low cost and easy to use, which might spur new A 3-axis accelerometer was placed at the location of applications and revitalise these technologies [2-4]. the apex beat in 5 healthy subjects in left lateral Specific advantages of apex-cardiography compared to decubitus position. ECG, echo Doppler of the carotid phonocardiography include its relation to left ventricular artery and phonocardiography were recorded pressure and the possibility to identify the timing of aortic simultaneous. The 3D displacements of the apex beat and mitral valve openings [5-6]. Modern applications of were estimated by twofold integration of the apex-cardiography might include screening for heart accelerometer signal. The most dominating displacement failure or quantification of ventricular synchrony. direction was estimated as the largest eigen vector in a To provide additional insight in the apex beat and principal component analysis (PCA). apex-cardiography we estimated the three dimensional The peak-to-peak displacements in the longitudinal, displacement of the apex beat using a 3-axis transverse and perpendicular dimensions were 0.39±0.35 accelerometer. -

Triple Heart Rhythm*
TRIPLE HEART RHYTHM * BY WILLIAM EVANS From the Cardiac Department of The London Hospital Received August 28, 1943 Triple heart rhythm stands for the cadence produced when three sounds recur in successive cardiac cycles, just as two sounds compose the familiar dual rhythm of cardiac auscultation, and more rarely, four sounds a quadruple rhythm. The conflicting views on the subject have long served to discourage attempts at a clinical perception of the problem. Disagreement is perhaps best illustrated by recounting the varied terminology employed to describe it. Thus we have gallop rhythm, canter rhythm, and trot rhythm; presystolic gallop, systolic gallop, protodiastolic gallop, and mesodiastolic gallop; complete summation gallop and incomplete summation gallop; auricular gallop, ventricular gallop, and auriculo-ventricular gallop; true gallop; left-sided gallop and right-sided gallop; rapid-filling gallop; diastolic echo; mitral opening snap; reduplication of first sound and reduplication of second sound; Potain's murmur; third heart sound and fourth heart sound. Others may have escaped my notice. This muddled nomenclature, as long as it stands, will frustrate any attempt to unify the many views held on triple rhythm. There is need of a simplified terminology based on clinical findings. It is indeed clear that a neglect of the clinical aspect on the one hand, and a persistence on the part ofmany to explain the mechanism of the supernumerary sound on the other hand, and to classify triple rhythm in accordance with sound records, have been largely responsible for obscuring this common form of cardiac rhythm. Phonocardiography need not become a routine test in clinical cardiology; when it has helped to establish a classification of triple rhythm it will have achieved its main purpose, though it will still serve in other auscultatory problems. -

Internal Diseases Propedeutics. Part II. Diagnostics of Cardiovascular
Federal budgetary educational establishment of higher education Ulyanovsk State University The Institute of medicine, ecology and physical culture Smirnova A.Yu., Gnoevykh V.V. INTERNAL DISEASES PROPEDEUTICS PART II DIAGNOSTICS OF CARDIOVASCULAR DISEASES Textbook of Medicine for medicine faculty students Ulyanovsk, 2016 1 УДК 811.11(075.8) БКК 81.432.1-9я73 С50 Reviewers: Savonenkova L.N. – MD, professor of Department of faculty therapy Smirnova A.Yu., Gnoevykh V.V. Internal diseases propedeutics (Part II). Diagnostics of cardiovascular diseases: Textbook of Medicine for medicine faculty students/Ulyanovsk: Ulyanovsk State University, 2017.-96 This publication is the second part of “ Internal diseases propedeutics”, which main goal is the practical assistance for students in the development of the fundamentals of clinical diagnosis of diseases of the cardiovascular system. It contains a description of the main methods of laboratory and instrumental diagnostic tests of diseases of the cardiovascular system. The publication is illustrated with charts, drawings and tables . The textbook is intended for students of medical universities. Smirnova A.Yu., Gnoevykh V.V., 2017 Ulyanovsk State University, 2017 2 THE CONTENTS OF A TEXT BOOK QUESTIONING OF PATIENTS WITH WITH CARDIOVASCULAR 5 DISEASES . Main complains of patients with with cardiovascular diseases . 5 EXAMINATION OF PATIENTS WITH WITH CARDIOVASCULAR 9 DISEASES . General inspection 9 Heart palpation 10 Palpation of vessels 14 Heart percussion 15 Defining of relative cardiac dullness borders. 15 Measurement of heart diameter. 18 Defining of vascular bundle borders 18 Defining of heart configuration. 19 Auscultation of the heart and blood vessels. 28 The heart auscultation: heart sounds abnormalities 31 The heart auscultation: heart murmurs 36 Intracardiac murmurs.