NEUROLOGY in TABLE (Special Neurology)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Musculoskeletal Upper Limb Anatomy and Assessment
Clinical Musculoskeletal Upper Limb Anatomy and Assessment Dr Matthew Szarko and Jeshni Amblum-Almér www.belmatt.co.uk 0207 692 8709 Email: [email protected] Contents: Shoulder Clinical Shoulder Anatomy Clinical Shoulder Assessment Clinical Case Studies of the Shoulder Elbow Clinical Elbow Anatomy Clinical Elbow Assessment Clinical Case Studies of the Elbow Wrist and Hand Clinical Wrist and Hand Anatomy Clinical Wrist and Hand Assessment Clinical Case Studies of the Wrist and Hand Clinical Shoulder Anatomy: The shoulder is the most mobile joint in the human body. Ranges of Movement - In which two of the following are we most mobile? Flexion, Extension, Abduction, Adduction Internal Rotation, External Rotation Clavicle o S-Shaped, double curved bone o Protects underlying brachial plexus and vascular structures. o Elevates along with upper limb elevation. Most clavicular fractures occur between the lateral 1/3 and medial 2/3. What is the characteristic deformity that results from a fractured clavicle? How does this affect mechanics of the shoulder? Clavicular Joints • Sternoclavicular joint • Acromioclavicular joint • Coracoacromial ligament What is the role of the acromion and coracoacromial ligament in maintaining glenohumeral stability? Scapula • Glenoid fossa • Spine • Acromion • Coracoid process • Supraglenoid tubercle • Infraglenoid tubercle • Supraspinous fossa • Infraspinous fossa • Subscapular fossa • Scapular notch Scapulothoracic Articulation Provides the following movements: Protraction, Retraction, Elevation, Rotation (during shoulder abduction): Proximal Humerus • Head • Anatomical neck • Surgical neck • Greater tubercle • Lesser tubercle • Intertubercular sulcus (bicipital groove) • Deltoid tuberosity • Spiral groove Glenohumeral Joint • Glenoid fossa • Glenoid labrum Extends the depth of the glenoid fossa to confer more stability. SLAP Tear - Detachment of Superior Labrum with Anterior-Posterior extension can occur from repetitive overhead activities or a sudden pull on the arm or compression (fall on outstretched arm). -

Peripheral Nerve Examination Ortho433
433 Orthopedic Team [Date] Peripheral Nerve Examination OSCE Peripheral Nerve Examination Learning Objectives: By the end of the teaching session, Students should be able to identify normality and abnormality by of the peripheral nerve by performing a proper physical examination. [email protected] 1 | P a g e 433 Orthopedic Team [Date] Peripheral Nerve Examination 1- Introduce yourself to the patient. 2- Confirm identity of the patient. ALWAYS 3- Explain and Obtain permission. COMPARE BOTH 4- Wash your hands and Ensure privacy. SIDES!!!! 5- Exposure: chest and arms, from umbilicus downward. 6- Position: standing\sitting - Follow same rule with U.L and L.L: Look Scars, ecchymosis, Muscle wasting/atrophy, dry cold skin, loss of hair, deformities. “Observe from front and behind” Feel Temperature, tenderness, Dermatome (pinprick\fine touch: Ask the patient to close his eyes and tell you if he felt your fine touch). “Check the dermatome next page” Move Active, Passive (motor power test against gravity and resistance). “Check the myotome next page” Special test Pulse, Capillary refill, Allen test “radial and ulnar arteries” 1st: Upper Limbs C4-T2 Radial .n (C5-T1) Median .n (C5-T1) Ulnar .n (C8-T1) Sensory Lateral 3 ½ dorsum of 3 1\2 lateral palm of the Medial 1 ½ fingers. the hand. hand. “test volar aspect of little 1st web space “test volar aspect of finger” index finger” Motor Wrist Dorsiflexion. Thumb Opposition Hypothenar muscles. Metacarpal joints “thumb to little finger” Abduction& Abduction of the extension. Thumb Abduction. fingers. Defect Wrist Drop Ape hand. Claw hand. Loss of sensory of Weak OK sign. -

Brachial Plexus Injuries: an Interactive Teaching and Learning Academic Model
International Journal of ChemTech Research CODEN (USA): IJCRGG, ISSN: 0974-4290, ISSN(Online):2455-9555 Vol.11 No.03, pp 01-08, 2018 Brachial plexus injuries: An interactive teaching and learning academic model Tarek M. El-gohary1,2*, Samiha M. Abdelkader3 1) Biomechanics Department, Faculty of Physical Therapy, Cairo University, Egypt 1) Board Certified Orthopedic Clinical Specialist, USA 1) Mechanical Diagnosis& Therapy, McKenzie Institute, USA 1) Pediatric Physical Therapy Consultant, NY,NY,USA 2) College of Medical Rehabilitation Sciences, Taibah University, Saudi Arabia 3) Physical Therapy Department, College of Applied Medical Science, King Saud University, Saudi Arabia Abstract : The purpose of this educational paper is to report the feedback from academics and students regarding newly introduced interactive teaching- learning model aiming to master brachial plexus injuries. An interactive questions and answers format was presented to number of academics and students at college of medical rehabilitation sciences. All academics and 90% of students reported that the newly introduced interactive teaching- learning model was helpful. It has been concluded that the interactive teaching- learning model is feasible and self- explanatory to be used and adopted by students and academics to facilitate the educational process. Keywords : Brachial plexus, injuries, teaching, learning, educational model. Introduction Brachial plexus is a group of intertwined nerves that emerge from the spinal cord in the cervical region and travel down the -

Clinical Approaches to the Wrist and Hand
Clinical Approaches to the Wrist and Hand Dr. Matthew Szarko [email protected] Clinical Anatomy Wrist Anatomy • Ulna – Styloid process • Styloid process of ulna connected to triquetral and pisiform bones by ulnar carpal ligament. – Triangular fibrocartilage Wrist Anatomy • Radius – Articulating surface for scaphoid and lunate • Radioulnar joint – Head of ulna-ulnar notch on distal radius – Motion: Supination and pronation Wrist Anatomy • Colle’s Fracture – Complete transverse fracture within distal 2 cm of radius. – Distal fragment displaced dorsally. – Results from forced dorsiflexion (fall from outstretched limb) – Dinner fork deformity Wrist Anatomy • Carpals – Proximal Row • Moveable • Scaphoid • Lunate • Triquetrum • Pisiform – Within flexor carpi ulnaris tendon- enhances mechanical advantage. Wrist Anatomy • Carpals – Distal Row • Immobile • Trapezium • Trapezoid • Capitate • Hamate Hand Anatomy • Metacarpals – I-V – Head – Neck • Phalanges – Proximal – Intermediate – Distal Hand Anatomy • Joints – Carpometacarpal (CMC) Joints – Metacarpophalangeal (MCP)Joints – Interphalangeal • Proximal Interphalangeal Joint (PIP) • Distal Interphalangeal Joint (DIP) • Digital articulations all designed to function in flexion. Arches of the Hand • Intrinsic hand muscles maintain arches . Distal Transverse • Proximal Transverse . Head of 3rd metacarpal as – Capitate as keystone keystone – Relatively flexed . Passes through all the – Along immobile distal carpal row metacarpal heads . More mobile Arches of the Hand • Longitudinal – Connects -
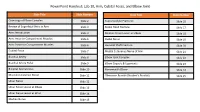
Powerpoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint
PowerPoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint Slide Title Slide Number Slide Title Slide Number Osteology of Elbow Complex Slide 2 Supracondylar Fractures Slide 16 Review of Superficial Veins in Arm Slide 3 Radial Head Fracture Slide 17 Arm: Introduction Slide 4 Median Nerve Lesion at Elbow Slide 18 Arm: Anterior Compartment Muscles Slide 5 Radial Nerve Slide 19 Arm: Posterior Compartment Muscles Slide 6 Humeral Shaft Fracture Slide 20 Cubital Fossa Slide 7 Medial Cutaneous Nerve of Arm Slide 21 Brachial Artery Slide 8 Elbow Joint Complex Slide 22 Brachial Artery Pulse Slide 9 Elbow Capsule & Ligaments Slide 23 Bicipital Aponeurosis Slide 10 Nursemaid’s Elbow Slide 24 Musculocutaneous Nerve Slide 11 Olecranon Bursitis (Student’s Bursitis) Slide 25 Ulnar Nerve Slide 12 Ulnar Nerve Lesion at Elbow Slide 13 Ulnar Nerve Lesion at Wrist Slide 14 Median Nerve Slide 15 Osteology of Elbow Complex To adequately review the learning objectives covering osteology of the distal humerus, radius, and ulna, view the Lower Limb Osteology and Medical Imaging Guide. Review of Superficial Veins in Arm The cephalic and basilic veins are the main superficial veins of the upper limb. They originate from the dorsal venous network on the dorsum of the hand. • The cephalic vein ascends along the anterolateral aspect of the forearm and arm. It then follows the superior border of the pectoralis major muscle to enter the deltopectoral triangle. It ultimately joins the axillary vein after passing through the clavipectoral fascia. • The basilic vein ascends along the medial forearm and the arm. In the arm, it passes deep to the brachial fascia where it courses in close proximity to the brachial artery and medial cutaneous nerve of the forearm along its path into the axilla. -

Nerves of Upper Limb
Examination Methods in Rehabilitation (26.10.2020) Nerves of the Upper Limb Mgr. Veronika Mrkvicová (physiotherapist) Nerves of the Upper Limb 1. Axillary nerve 2. Musculocutaneuous nerve 3. Radial nerve 4. Median nerve 5. Ulnar nerve Brachial plexus • Networking of spinal nerves, formed by ventral (anterior rami) of cervical spinal nerves C5-C8 and thoracic spinal nerves T1 • It is responsible for cutaneous (sensory) and muscular (motor) innervation of the entire upper limb Brachial plexus • 5 main nerves arise from brachial plexus: 1. Axillary nerve 2. Musculocutaneuous nerve 3. Radial nerve 4. Median nerve 5. Ulnar nerve Nerves of the Upper Limb - sensitivity The cutaneous inervation of the right hand Axillary nerve • From root C5-C6 • Arise from posterior cord of brachial plexus at the level of axilla Innervations of the Axillary nerve Muscular innervations: • Anterior branch – anterior and lateral fiber of deltoid muscles • Posterior branch – teres minor and posterior fiber of deltoid Cutaneuos innervation: • Superior lateral brachial cutaneous nerve • Carry information from the shoulder joint • Skin covering inferior region of deltoid muscles Axillary nerve paralysis • Frequently injured due to shoulder dislocation because of the proximity of this joint • Paralysis of the deltoid and teres minor – it results in weakness of the arm abduction Musculocutaneous nerve Innervation of the Musculocutaneous nerve Median nerve • The median nerve is one of the 5 main nerves originating from the brachial plexus • It originates from the lateral -

Abstracts of Paper Presentations During the 57Th National
Abstracts ?f Paper Presentations during the 57111 National Conference of AnatomicaL Society of lnd1a, 2009 held at KLE University's Jawharlal Nehru Medical College, Belgaum. Abstra_cts of Paper Presentations during the 57'h National Conference of Anatomical Society of India, 2009 held at KLE University's Jawharlal Nehru Medical College, Belgaum. 1. Morphometric Analysis Of The Menisci Of The Knee blood vessels was noted. On the right side the common Joint In Human Fetuses carotid ~rtery was absent. The right external carotid artery Murali Manju, Narga Nair", Shaku.ntala R. Pai", Mangala arose directly from the arch of aorta. The brachiocephalic M. Pai, trunk was present on the left side giving left common carotid Chandra Philip·, Chandni Gupta· artery and left subclavian artery. The left common carotid Kasturba Medical College, Manipal University, Bejai, artery had a broad diameter and it divided into external Mangalore, "Kasturba Medical college, Manij)al University, and in~er.nal c~rotid arteries. The left internal carotid artery Manipal, Karnataka. had a w1de diameter and it gave two subdivisions. The The aim of the study: To Analyse the morphometric right subdivision crossed over to the right side aspects of the knee joint menisci such as: external compensating for the absent right internal carotid artery. circumference thickness, the width, the peripheral and inner The left subd.ivision continued as the internal carotid artery border lengths, the distance between anterior and posterior of the left s1de. The embryological, morphological and clinical implications of this unique· anamoly will be horns. Materials and Methods: Human Fetal cadavers discussed at the conference venue. -

Peripheral Nerves Examination.Pdf
Done By: Ahlam AlMutairi (F1) Eman AlBadaie (F1) Team Leader: Khulood AlRaddadi (F1) [email protected] Color Code: Slides Sessions’ Notes Team Notes Important 431 team work Arabic Words Books’ notes Other Sources Orthopedics OSCE (Upper Limb): Quick anatomy review: (for your knowledge and to help you better understand the examination ) Muscles innervated Primary action A) Forearm: - Anterior compartment except 1.5 - Flex wrist and all digits muscles by ulnar n (flexor carpi ulnaris - Pronation and ulnar half of the flexor digitorum Median nerve profundus) (C5-T1) - Opposition of thumb B) Hand: - Flex MP and extend PIP and DIP - Thenar muscles: (Opponens pollicis) of digits 2& 3 - Lumbricals digits (2 & 3) A) Forearm: - Flex wrist (weak) and digits 4 - Flexor carpi ulnaris and ulnar half of the &5 flexor digitorum profundus - Opposition of little finger B) Hand: - Abduction and adduction of the Ulnar nerve - Hypothenar muscles fingers+ flex MP+ extend IP. (C8-T1) - 8 Interossei muscles (palmar &dorsal) Flex MP and extend PIP and DIP - Lumricals (digits 4 & 5) of digits 4& 5 - Adductor pollicis - adduct the thumb Radial nerve Posterior compartment muscles of the - Extend MP, wrist and elbow (C5-T1) arm and forearm Median nerve - Redness, scars - Muscles wasting: Thenar muscle 1- Look: - Deformity: Ape hand deformity Ask the patient to close his eyes and tell you if he felt your fine touch (with cotton ball) in: 2- Feel: The volar aspect of index finger and ask if it is the same sensation on both (test sensory) hands (comment e.g. bilateral symmetrical sensation on both sides) 3-Move: Ask the patient to do the following: Thumb abduction or Thumb opposition to (test motor) little finger (not to index for OK sign) Test the power of opposition by asking him to resist your attempt to break the 4- Power opposition circle. -
Tendon Transfer Rehabilitation
Volume 6, Issue 2 www.exploringhandtherapy.com July 2006 From The Editors Desk In This Issue Hot summer days... we have some great EARN program. You can receive FREE Featured Article .......................................1 What’s Hot ........................................... 16 new releases to cool you off, check them CEU’s for reading this magazine. See In The Spotlight .......................................3 Splinting Tips .........................................16 out on page 8. details on page 14. See you online. In The Web .............................................6 Ask The Expert.......................................17 If your are studying for Certification in Newly released courses ..........................8 Test Answers .........................................21 Hand Therapy, don’t miss the Hand EHT’s magazine is for informational Therapy Certification Package purposes only and is not intended to be a Political Corner.......................................10 Ergo Tips and Tricks ..............................23 Discount PROMO. This package is substitute for professional medical advice, LEARN & EARN.....................................14 Modalities...............................................24 designed to help you study for the big day. diagnosis or treatment. Always consult Check out details on page 8. with your supervisor before implementing POP Quiz ...............................................14 EHT’s hand club is designed for ideas. networking, sharing, and learning Thank you to our sponsors for making this Hand while having fun. All of your posts are ng Th magazine possible. Please click on their ri e o r answered. You can even post photos for ll a ad (if viewing online) to learn more. pp pp y those perplexing cases and the club will xx y E E help you out. So don’t hesitate join today. ENJOY! w w m o w c . e T ® . See page 6 for details. -

Physical Therapy of the Wrist and Hand Functional Anatomy Wrist and Hand
Physical therapy of the wrist and hand Functional anatomy wrist and hand • The wrist includes distal radius, scaphoid, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, and hamate. • The hand includes five metacarpals and 14 phalanges make up the hand and five digits • The wrist is allowed for FL, EXT, radial deviation and ulnar deviation Functional anatomy: the radiocarpal joint • The radiocarpal joint: – The concave distal end of the radius and radioulnar disc connects the convex proximal row of the scaphoid, lunate, and triquetrum. – The triquetrum is mainly articulated with the disc Functional anatomy: the radiocarpal joint • Physiological motion of • Carpal glide of the wrist proximal row –Flexion – Dorsal – Extension – Volar – Radial deviation – Ulnar – Ulnar deviation – Radial Functional anatomy: the midcarpal joint • The proximal row of the scaphoid, lunate, and triquetrum articulates with the distal row the trapezium, trapezoid, capitate, and hamate. • The capitate and hamate are convex and glide on the concave surface of the scaphoid, lunate, and triquetrum • The concave trapezium and trapezoid glide on the convex distal surface of the scaphoid Functional anatomy: the carpometacarpal (CMC) joint of digit 2 through 5 • Between each metacarpal and the distal row of carpals and the articulations between the base of each metacarpal • The flexion of the metacarpals and additional adduction of the fifth contribute to the cupping of the hand, improving prehension. Functional anatomy: the carpometacarpal (CMC) joint of the thumb • Saddle-shaped joint between the trapezium and base of the first metacarpal. • For flexion-extension of the thumb occurring in the frontal plane, the trapezium is convex and the base of the metacarpal is concave. -

Median Nerve Variation
ISSN: 0975-8585 Research Journal of Pharmaceutical, Biological and Chemical Sciences Median Nerve Variation. M Kavimani1*, K Suba Anandhi2, and Christilda Felicia Jebakani3. 1Department of Anatomy, Sree Balaji Medical College and Hospital (Bharath university), Chrompet, Chennai, Tamil Nadu, India. 2Department of Anatomy, Indira Gandhi Medical College and Hospital, Pondicheery, India. 3Department of Anatomy, Madras Medical College and Hospital, Chennai, Tamil Nadu, India. ABSTRACT The median nerve is a nerve in humans and other animals in the upper limb. It is one of the five main nerves originating from the brachial plexus. The median nerve is formed from contributions from the lateral and medial cords of the brachial plexus, originating from ventral roots of C5, C6 & C7 (lateral cord) and C8 & T1 (medial cord). The present study was done by dissecting forearm and palm in the human cadaver available in the Institute of Anatomy, Madras medical college, Chennai. In the present study on 15 specimens of upper limb the accessory muscular branch to thenar muscles is seen in 20%. Of which in 10% the accessory branch to the thenar muscles is arising proximal to the flexor retinaculum from the main nerve trunk. In 5% the accessory branch to the thenar muscles is arising distal to the flexor retinaculum from the proper digital branch to the lateral sides of the thumb. Keywords: Recurrent muscular branch, flexor retinaculum, median nerve. *Corresponding author November - December 2014 RJPBCS 5(6) Page No. 805 ISSN: 0975-8585 INTRODUCTION The median nerve receives fibers from roots C6, C7, C8, T1 and sometimes C5 [1]. It is formed in the axilla by a branch from the medial and lateral chords of the brachial plexus, which are on either side of the axillary artery and fuse together to create the nerve anterior to the artery. -
Feil Syndrome: a Rare Clinical Case and Literature Review
Hirurgia Pozvonochnika 2021;18(1):6–13 E.V. Petrova et al., 2021 Staged surgical treatment of brachioplexopathy in an adolescent with Klippel – Feil syndrome: a rare clinical case and literature review E.V. Petrova1, O.E. Agranovich1, M.V. Savina1, E.L. Gabbasova1, V.P. Snishchuk1–3, A.Yu. Mushkin2, 4 1H. Turner National Medical Research Center for Сhildren’s Orthopedics and Trauma Surgery, St. Petersburg, Russia 2St. Petersburg Research Institute of Phthisiopulmonology, St. Petersburg, Russia 3Leningrad Regional Children’s Clinical Hospital, St. Petersburg, Russia 4Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia Klippel – Feil syndrome is a congenital malformation, the leading component of which is a violation of segmentation of the cervical ver- tebral bodies. The syndrome can be combined with other skeletal anomalies: skull asymmetry, scoliosis, high shoulder blades, and cervi- cal ribs. Treatment of the syndrome is usually symptomatic; indications for surgical treatment are progressive neurological disorders and persistent pain syndrome, which usually develop due to instability of unblocked segments, or neurogenic pain. A clinical case of treatment of a 17-year-old patient with Klippel – Feil syndrome who developed a picture of severe upper limb monoparesis during three years due to compression of the brachial plexus associated with cervical ribs is presented. Decompression of the brachial plexus was performed, which led to rapid relief of pain syndrome and gradual partial regression of motor disorders. Due to incomplete restoration of the gripping func- tion, tendon-muscle plasty of the right hand was performed, which significantly improved the possibility of self-care. The results of radia- tion and staged neurophysiological studies are described, as well as a review of the literature on the Klippel – Feil syndrome.