NAMS 53 4.Cdr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cons 103020 Sf.Pdf
OUTSTANDING AMOUNT IN ASSET DATE OF DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR DIN FOR DIRECTOR PAN_DIR1 DIN FOR DIRECTOR DIN FOR DIRECTOR PAN_DIR1 DIN FOR DIRECTOR PAN_DIR1 DIN FOR DIRECTOR PAN_DIR1 DIN FOR DIRECTOR PAN_DIR1 DIN FOR DIRECTOR PAN_DIR1 DIN FOR DIRECTOR SRNO PARTY CREDIT GRANTOR STATE CREDIT GRANTOR BRANCH REGISTERED ADDRESS SUIT OTHER BANK DIRECTOR 1 PAN_DIR1 DIN FOR DIRECTOR 1 DIRECTOR 2 PAN_DIR2 DIRECTOR 3 PAN_DIR3 DIRECTOR 4 PAN_DIR4 DIRECTOR 5 PAN_DIR5 DIRECTOR 6 PAN_DIR6 DIN FOR DIRECTOR 6 DIRECTOR 7 PAN_DIR7 DIRECTOR 8 PAN_DIR8 DIN FOR DIRECTOR 8 DIRECTOR 9 PAN_DIR9 DIRECTOR 10 PAN_DIR10 DIRECTOR 11 PAN_DIR11 DIRECTOR 12 PAN_DIR12 DIRECTOR 13 DIRECTOR 14 PAN_DIR14 DIRECTOR 15 DIRECTOR 16 DIRECTOR 17 DIRECTOR 18 DIRECTOR 19 DIRECTOR 20 LACS CLASSIFICATION CLASSIFICATION 2 3 4 5 7 9 10 11 12 3 13 14 5 15 6 16 7 17 8 18 9 19 1 Datar Switchgears Ltd. HDFC BANK LTD Maharashtra Nasik Datar Commpercial Complex, Vakil Wadi, Nasik 422 001. 1086 Loss Assets 31.08.2001 Suit Rajan Datar Shobhana Datar Sophi, 18 New Kanta Wadi Road, Off.Perry Cross Road, Bandra, 2 East West Travels & Trade Links HDFC BANK LTD Maharashtra Mumbai 194 Loss Assets 31.03.2001 Suit Thakiyudeen Wahid Naserudhin Wahid Mumbai - 400 050. 604/65, Keshava Building, Bandra Kurla Complex, Bandra (East), 3 Kedia Distilleries Ltd. HDFC BANK LTD Maharashtra Mumbai 309 Loss Assets 30.04.1998 Suit K.P. Kedia Vinay Kedia P.K. Deora T.C. -

53Rd AIIMS ANNUAL REPORT 2008–2009
53rd AIIMS ANNUAL REPORT 2008–2009 All India Institute of Medical Sciences New Delhi 110029 Edited jointly by: Dr Sunil Chumber, Additional Professor, Department of Surgical Disciplines and Sub-Dean (Academic) Dr Tanuj Dada, Associate Professor, Dr R.P. Centre for Ophthalmic Sciences Dr Venkata Karthikeyan C, Assistant Professor, Department of Otorhinolaryngology (ENT) Dr S.K. Maulik, Professor, Department of Pharmacology Dr Raj D. Mehra, Professor, Department of Anatomy Dr Kameshwar Prasad, Professor, Department of Neurology Dr S. Rastogi, Professor, Department of Orthopaedics Dr Sushma Sagar, Assistant Professor, JPNA Trauma Centre Dr Peush Sahni, Professor, Department of Gastrointestinal Surgery Dr Pratap Sharan, Professor, Department of Psychiatry Dr D.N. Sharma, Assistant Professor, Dr BRA, Institute Rotary Cancer Hospital Dr Subrata Sinha, Professor and Head, Department of Biochemistry Dr Sanjay Kumar Sood, Assistant Professor, Department of Physiology Dr Sachin Talwar, Assistant Professor, Department of C.T.V.S. February 2010 Printed at Saurabh Printers Pvt. Ltd., A-16, Sector-IV, NOIDA (U.P.) All India Institute of Medical Sciences The All India Institute of Medical Sciences (AIIMS) was established in 1956 as an institution of national importance by an Act of Parliament with the objects to develop patterns of teaching in undergraduate and postgraduate medical education in all its branches so as to demonstrate a high standard of medical education to all medical colleges and other allied institutions in India; to bring together in one place educational facilities of the highest order for the training of personnel in all important branches of health activity and to attain self-sufficiency in postgraduate medical education. -

Current Affairs 2013- January International
Current Affairs 2013- January International The Fourth Meeting of ASEAN and India Tourism Minister was held in Vientiane, Lao PDR on 21 January, in conjunction with the ASEAN Tourism Forum 2013. The Meeting was jointly co-chaired by Union Tourism Minister K.Chiranjeevi and Prof. Dr. Bosengkham Vongdara, Minister of Information, Culture and Tourism, Lao PDR. Both the Ministers signed the Protocol to amend the Memorandum of Understanding between ASEAN and India on Strengthening Tourism Cooperation, which would further strengthen the tourism collaboration between ASEAN and Indian national tourism organisations. The main objective of this Protocol is to amend the MoU to protect and safeguard the rights and interests of the parties with respect to national security, national and public interest or public order, protection of intellectual property rights, confidentiality and secrecy of documents, information and data. Both the Ministers welcomed the adoption of the Vision Statement of the ASEAN-India Commemorative Summit held on 20 December 2012 in New Delhi, India, particularly on enhancing the ASEAN Connectivity through supporting the implementation of the Master Plan on ASEAN Connectivity. The Ministers also supported the close collaboration of ASEAN and India to enhance air, sea and land connectivity within ASEAN and between ASEAN and India through ASEAN-India connectivity project. In further promoting tourism exchange between ASEAN and India, the Ministers agreed to launch the ASEAN-India tourism website (www.indiaasean.org) as a platform to jointly promote tourism destinations, sharing basic information about ASEAN Member States and India and a visitor guide. The Russian Navy on 20 January, has begun its biggest war games in the high seas in decades that will include manoeuvres off the shores of Syria. -

General Studies Series
IAS General Studies Series Current Affairs (Prelims), 2013 by Abhimanu’s IAS Study Group Chandigarh © 2013 Abhimanu Visions (E) Pvt Ltd. All rights reserved. No part of this document may be reproduced or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or any information storage or retrieval system or otherwise, without prior written permission of the owner/ publishers or in accordance with the provisions of the Copyright Act, 1957. Any person who does any unauthorized act in relation to this publication may be liable to criminal prosecution and civil claim for the damages. 2013 EDITION Disclaimer: Information contained in this work has been obtained by Abhimanu Visions from sources believed to be reliable. However neither Abhimanu's nor their author guarantees the accuracy and completeness of any information published herein. Though every effort has been made to avoid any error or omissions in this booklet, in spite of this error may creep in. Any mistake, error or discrepancy noted may be brought in the notice of the publisher, which shall be taken care in the next edition but neither Abhimanu's nor its authors are responsible for it. The owner/publisher reserves the rights to withdraw or amend this publication at any point of time without any notice. TABLE OF CONTENTS PERSONS IN NEWS .............................................................................................................................. 13 NATIONAL AFFAIRS .......................................................................................................................... -
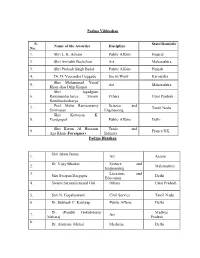
Padma Vibhushan S. No. Name of the Awardee Discipline State/Domicile
Padma Vibhushan S. State/Domicile Name of the Awardee Discipline No. 1. Shri L. K. Advani Public Affairs Gujarat 2. Shri Amitabh Bachchan Art Maharashtra 3. Shri Prakash Singh Badal Public Affairs Punjab 4. Dr. D. Veerendra Heggade Social Work Karnataka Shri Mohammad Yusuf 5. Art Maharashtra Khan alias Dilip Kumar Shri Jagadguru 6. Ramanandacharya Swami Others Uttar Pradesh Rambhadracharya Prof. Malur Ramaswamy Science and 7. Tamil Nadu Srinivasan Engineering Shri Kottayan K. 8. Venugopal Public Affairs Delhi Shri Karim Al Hussaini Trade and 9. France/UK Aga Khan ( Foreigner) Industry Padma Bhushan Shri Jahnu Barua 1. Art Assam Dr. Vijay Bhatkar Science and 2. Maharashtra Engineering 3. Literature and Shri Swapan Dasgupta Delhi Education 4. Swami Satyamitranand Giri Others Uttar Pradesh 5. Shri N. Gopalaswami Civil Service Tamil Nadu 6. Dr. Subhash C. Kashyap Public Affairs Delhi Dr. (Pandit) Gokulotsavji Madhya 7. Art Maharaj Pradesh 8. Dr. Ambrish Mithal Medicine Delhi 9. Smt. Sudha Ragunathan Art Tamil Nadu 10. Shri Harish Salve Public Affairs Delhi 11. Dr. Ashok Seth Medicine Delhi 12. Literature and Shri Rajat Sharma Delhi Education 13. Shri Satpal Sports Delhi 14. Shri Shivakumara Swami Others Karnataka Science and 15. Dr. Kharag Singh Valdiya Karnataka Engineering Prof. Manjul Bhargava Science and 16. USA (NRI/PIO) Engineering 17. Shri David Frawley Others USA (Vamadeva) (Foreigner) 18. Shri Bill Gates Social Work USA (Foreigner) 19. Ms. Melinda Gates Social Work USA (Foreigner) 20. Shri Saichiro Misumi Others Japan (Foreigner) Padma Shri 1. Dr. Manjula Anagani Medicine Telangana Science and 2. Shri S. Arunan Karnataka Engineering 3. Ms. Kanyakumari Avasarala Art Tamil Nadu Literature and Jammu and 4. -

Sl.No Membership Id Name State
Sl.No Membership Id Name State 1 10 BHAT K L DELHI 2 13 ADINARAYANA RAO S V ANDHRA PRADESH 3 20 AGARWAL S K WEST BENGAL 4 22 AGARWAL Y M HARYANA 5 26 AGARWAL P K JHARKHAND 6 32 AHMAD ABDUL HAI BIHAR 7 33 AHUJA A M LT GENERAL DELHI 8 35 SINGHVI A M RAJASTHAN 9 39 ALMAST S C DELHI 10 46 AMARESH BHASKAR NALLAVANDU AIR MSHL KARNATAKA 11 47 AMARESWAR T KARNATAKA 12 48 AMARJIT SINGH PUNJAB 13 49 AMBIKE V S MAHARASTRA 14 55 ANAND PRAKASH UTTAR PRADESH 15 58 ANANTHAKRISHNAN L TAMIL NADU 16 59 NARAYAN PRASAD K TAMILNADU 17 60 ANANTHANARAYANA RAO N KARNATAKA 18 72 ANTIA N H MAHARASTRA 19 76 APTE B P MAHARASTRA 20 79 ARCANJO DE MENESES GOA 21 83 ARORA S MAHARASTRA 22 91 ASOPA H S UTTAR PRADESH 23 95 VIKRAM PRATAP SINGH LT. COL. DELHI 24 101 BAJAJ P S BIHAR 25 108 BAPAT V C MADHYA PRADESH 26 109 BHATTACHARYYA S MAHARASTRA 27 118 KRISHNA HANDE H TAMIL NADU 28 123 BALLAL C R KARNATAKA 29 127 BAMRAH N S BRIG CHANDIGARH 30 130 BANERJEE L K DELHI 31 131 BANERJEE S WEST BENGAL 32 134 ASHIM BANERJEE(COL) WEST BENGAL 33 138 BAPAT S D MAHARASHTRA 34 140 DEEPAK V BHATT GUJARAT 35 147 PRANAB KUMAR BASU UTTAR PRADESH 36 149 BAWA H S PUNJAB 37 153 BEHERA D K ODISHA 38 159 BHAJEKAR A B MAHARASTRA 39 161 BAKTHAVATSALAM G TAMIL NADU 40 163 BHALERAO R A MAHARASHTRA 41 170 BHANUSHALI H S MAHARASTRA 42 176 BHARUCHA P B MAHARASTRA 43 179 BHASALE S P MAHARASHTRA 44 184 BHATT M V MAHARASHTRA 45 188 BHATHENA T R MAHARASHTRA 46 189 JAGDISHWER BHATT RAJASTHAN 47 195 SINGARAJU KRISHNA PRABHAKAR TELANGANA 48 199 RAVIKANTH C BANGALORE KARNATAKA 49 200 BHAKTA V P MAHARASTRA 50 -

January 2013
January1 of 91. 2013 International affairs: US President Barack Obama on 31 January, has come out with his much-awaited comprehensive immigration reforms, that will pave the way for legalization of more than 11 million undocumented immigrants. The reforms, which also propose to eliminate the annual country caps in the employment category, are expected to benefit large number of Indian technocrats and professionals. In a major policy speech on comprehensive immigration in Las Vegas, Obama urged the Congress to act on his proposals. The other key proposals of his "comprehensive" reform plan include "stapling" a green card to the diplomas of science, technology, engineering and mathematics (STEM), PhD and Masters Degree graduates from qualified US universities who have found employment in the country. The President also proposed to create a startup visa for job-creating entrepreneurs. The proposal allows foreign entrepreneurs, who attract financing or revenue from American investors and customers, to start and grow their businesses in the US, and to remain permanently if their companies grow further, create jobs for American workers, and strengthen the economy. The proposal removes the backlog for employment-sponsored immigration by eliminating annual country caps and adding additional visas to the system. Outdated legal immigration programs are reformed to meet current and future demands by exempting certain categories from annual visa limitations, the White House said. Obama also proposed to eliminate existing backlogs in the family-sponsored immigration system by recapturing unused visas and temporarily increasing annual visa numbers. The proposal also raises existing annual country caps from seven per cent to 15 per cent for the family-sponsored immigration system. -

Total No. of Diesel Vehicles Registered in ROHINI
Total No. of Diesel Vehicles is registered before 07-nov-2001 or 15 years old and not have valid fitness on 08-nov-2016 Sno regn_no regn_dt fit_upto owner_name f_name p_add1 p_add2 p_add3 p_pincodedescr off_name 76028 DNH5736 10-11-1989 09-11-2004 MADHU SHARMA & VARINDER KUMAR 73-A KHANNA MARKET TIS HAZARI DELHI 0 DIESEL ROHINI 76029 DL8C7087 24-08-1994 23-08-2009 SUBODH SINGH SUGRIV SINGH A-30 EAST UTTAM NGR DELHI 0 DIESEL ROHINI 76030 DL8CB8642 09-04-1997 08-04-2012 PRITHVI RAJ SH PYARE LAL 228 VILL SAMAI PUR DELHI-42 0 DIESEL ROHINI 76031 DL8CB4169 19-06-1996 18-06-2011 DINESH RANBIR SINGH N 8 SATYAWATI COLY ASHOK VIHAR DELHI 0 DIESEL ROHINI 76032 DNH2099 15-09-1989 14-09-2004 THE TRESURER AICC (I) NA 24 AKBAR ROAD NEW DE LHI 0 DIESEL ROHINI 76033 DNH4334 23-10-1989 22-10-2004 MANJU CHAUHAN W/O SATPAL CHAUHAN 2175/114 H NO 118 PANCHSHEEL VIHAR KHIRKI EXTN.N DELHI 0 DIESEL ROHINI 76034 DL8C4418 15-04-1994 14-04-2009 RAMA KANT S/O MAUJI RAM L-159 J J COLONY AM SHAKARPUR DELHI 0 DIESEL ROHINI 76035 DL8CB7350 06-12-1996 05-12-2011 SUKDEEP SINGH BHAGWANT SINGH 8 POOSA ROAD DELHI 0 DIESEL ROHINI 76036 DL8CB7351 06-12-1996 05-12-2011 PREM WATI JILE SINGH TIKRI KALAN DELHI 45 0 DIESEL ROHINI 76037 DNH2582 27-09-1989 26-09-2004 SH RAJEEV BABEL S/O SH D C BABEL C-29 N D S E PART-I AMRIT NAGAR N DELHI 110049 0 DIESEL ROHINI 76038 DL8C8385 19-02-1996 18-02-2011 NA NA NA 0 DIESEL ROHINI 76039 DL8CB8009 04-02-1997 03-02-2012 MD ASIF NAIM JEHRA H N 98 KHUREJI KHAS DL 51 0 DIESEL ROHINI 76040 DL8CG4870 02-07-2001 01-07-2016 SOMESHWAR SINGH SH HEM PAL SINGH C-II/48 NEW ASHOK NAGAR DELHI . -

National Law University, Delhi Sector-14, Dwarka New Delhi-110078
NATIONAL LAW UNIVERSITY, DELHI SECTOR-14, DWARKA NEW DELHI-110078 ALL INDIA LAW ENTRANCE TEST-2016 (AILET-2016), B.A. LL.B.(HONS.) RESULT Marks Wise S.No. Roll No Name of the Candidate Name of Father/Mother/ Guardian DoB Gender Marks 1 52788 KARAN DHALLA DEEPESH DHALLA 03/02/1998 M 119 2 55979 SHUBHAM JAIN BHUPENDRA JAIN 20/11/1997 M 116 3 56876 VANSH AGGARWAL PAWAN SINGHAL 25/03/1998 M 116 4 63245 ARTH NAGPAL RAJESH NAGPAL 28/08/1997 M 114 5 64122 RIJU SHRIVASTAVA YUGENDRA ARYA 27/04/1998 F 114 6 69185 ROHIL BIPIN DESHPANDE BIPIN GAJANAN DESHPANDE 10/05/1998 M 114 7 70191 ARVIND KUMAR TIWARI AKHILESH CHANDRA TIWARI 03/10/1997 M 114 8 75260 ANUBHUTI GARG ARUN GARG 13/06/1997 F 114 9 63398 EKANSH ARORA RAJESH ARORA 08/01/1997 M 113 10 66089 KARISHMA KARTHIK KARTHIK SUBRAMANIAN 06/04/1998 F 113 11 75266 ANUNA TIWARI SANJAY TIWARI 14/08/1997 F 113 12 77055 ANMOL DHAWAN SANJEEV DHAWAN 29/12/1998 M 113 13 77061 ANUKRITI KUDESHIA ANURODH KUDESHIA 27/09/1997 F 113 14 64048 PRANSHU SHUKLA SANJAY SHUKLA 24/02/1998 M 112 15 71044 NIKHIL SHARMA PRAMOD KUMAR SHARMA 21/01/1997 M 112 16 75365 AVANI AGARWAL SURENDRA KUMAR AGARWAL 28/06/1998 F 112 17 63385 DIVYA KUMAR GARG NITIN GARG 05/04/1998 M 111 18 64071 PRIYANKA CHATURVEDI D. P. CHATURVEDI 20/02/1997 F 111 19 72316 PRITHVI JOSHI ARUN JOSHI 28/10/1998 M 111 20 74213 SHIVAM SINGHANIA SUNIL SINGHANIA 27/02/1998 M 111 21 74227 SHREYA JAIPURIA BIRENDRA JAIPURIA 22/12/1997 F 111 22 77417 SREEDEVI GOPALAKRISHNAN NAIR GOPALAKRISHNAN NAIR 01/07/1997 F 111 23 50911 ANKUR SINGHAL ANIL KUMAR SINGHAL 26/12/1997 -

Awards & Honours
1st January to 15 th January AWARDS & HONOURS The Hollywood Foreign Press Association (HFPA) presented the 72nd Annual Golden Globe Awards. The winners are:- BEST MOTION PICTURE DRAMA - Boyhood (IFC Films) BEST PERFORMANCE BY AN ACTRESS IN A MOTION PICTURE – DRAMA - Julianne Moore – Still Alice BEST PERFORMANCE BY AN ACTOR IN A MOTION PICTURE DRAMA - Eddie Redmayne – The Theory of Everything BEST MOTION PICTURE COMEDY OR MUSICAL - The Grand Budapest Hotel (Fox Searchlight) BEST PERFORMANCE BY AN ACTRESS IN A MOTION PICTURE – COMEDY OR MUSICAL - Amy Adams – Big Eyes BEST PERFORMANCE BY AN ACTOR IN A MOTION PICTURE – COMEDY OR MUSICAL- Michael Keaton – Birdman BEST ANIMATED FEATURE FILM - How to Train a Dragon 2 (DreamWorks Animation) BEST FOREIGN LANGUAGE FILM - Leviathan – Russia (Sony Pictures Classics) Prime Minister Narendra Modi released commemorative coins to honour Tata Group founder Jamsetji Nusserwanji Tata. PM released coins in the denomination of 100 and five rupee to mark Jamsetji Tata’s 175th birth anniversary. Thus, Jamsetji will be the first industrialist in India to be felicitated by the government in such a manner. So far government has minted coins in honour of artists, freedom fighters, scientists, institutions and organisations. Reserve Bank of India's (RBI) Raghuram Rajan has been awarded as the Governor of the Year in the Central Banking Awards for 2015, while the Reserve Bank of New Zealand (RBNZ) scooped the prize for Central Bank of the Year. Last year, Rajan was also conferred with the Best Central Bank Governor award for 2014 by the Euromoney magazine for his tough monetary stance to combat the 'ravaging deficit-ridden economy' and battling vested interests "to arouse a sleepy financial system for over one billion people.” French economist Thomas Piketty, who rose to international fame after the publication of his book, “Capital in the Twenty-First Century,” in 2013, turned down Legion D'Honneur -- France’s highest distinction. -

Alphabetical List of Persons for Whom Recommendations Were Received for Padma Awards - 2015
Alphabetical List of Persons for whom recommendations were received for Padma Awards - 2015 Sl. No. Name 1. Shri Aashish 2. Shri P. Abraham 3. Ms. Sonali Acharjee 4. Ms. Triveni Acharya 5. Guru Shashadhar Acharya 6. Shri Gautam Navnitlal Adhikari 7. Dr. Sunkara Venkata Adinarayana Rao 8. Shri Pankaj Advani 9. Shri Lal Krishna Advani 10. Dr. Devendra Kumar Agarwal 11. Shri Madan Mohan Agarwal 12. Dr. Nand Kishore Agarwal 13. Dr. Vinay Kumar Agarwal 14. Dr. Shekhar Agarwal 15. Dr. Sanjay Agarwala 16. Smt. Raj Kumari Aggarwal 17. Ms. Preety Aggarwal 18. Dr. S.P. Aggarwal 19. Dr. (Miss) Usha Aggarwal 20. Shri Vinod Aggarwal 21. Shri Jaikishan Aggarwal 22. Dr. Pratap Narayan Agrawal 23. Shri Badriprasad Agrawal 24. Dr. Sudhir Agrawal 25. Shri Vishnu Kumar Agrawal 26. Prof. (Dr.) Sujan Agrawal 27. Dr. Piyush C. Agrawal 28. Shri Subhash Chandra Agrawal 29. Dr. Sarojini Agrawal 30. Shri Sushiel Kumar Agrawal 31. Shri Anand Behari Agrawal 32. Dr. Varsha Agrawal 33. Dr. Ram Autar Agrawal 34. Shri Gopal Prahladrai Agrawal 35. Shri Anant Agrawal 36. Prof. Afroz Ahmad 37. Prof. Afzal Ahmad 38. Shri Habib Ahmed 39. Dr. Siddeek Ahmed Haji Panamtharayil 40. Dr. Ranjan Kumar Akhaury 41. Ms. Uzma Akhtar 42. Shri Eshan Akhtar 43. Shri Vishnu Akulwar 44. Shri Bruce Alberts 45. Captain Abbas Ali 46. Dr. Mohammed Ali 47. Dr. Govardhan Aliseri 48. Dr. Umar Alisha 49. Dr. M. Mohan Alva 50. Shri Mohammed Amar 51. Shri Gangai Amaren 52. Smt. Sindhutai Ramchandra Ambike 53. Mata Amritanandamayi 54. Dr. Manjula Anagani 55. Shri Anil Kumar Anand 56. -

National Academy of Medical Sciences (India)
NATIONAL ACADEMY OF MEDICAL SCIENCES (INDIA) ANNUAL REPORT 2015-16 NAMS House Ansari Nagar, Mahatma Gandhi Marg, New Delhi - 110029 Postal Address: NATIONAL ACADEMY OF MEDICAL SCIENCES (INDIA) NAMS House, Ansari Nagar, Mahatma Gandhi Marg, New Delhi – 110029 Telephone: 011-26588718 President : 011-26588792 Secretary : 011-26589289 Fax No.: 011-26588992 E-mail: [email protected] Website: http://nams-india.in CONTENTS Page No. The Council ─ 2015-16 1 Officers & Executive Staff 2 Editorial Board of Annals of NAMS 3 A. Organizational Activities 5 Organisational Activities & Annual Meeting 7 Award of Fellowships & Memberships at the Annual Meeting 8-17 Lifetime Achievement Award for the year 2014 18 Orations and Awards 19-24 NAMS 2007 Amritsar Award 25 Prof. J.S. Bajaj Award 25 Meetings of the Council 26 Election of Fellows – 2015 26-30 Election of Members – 2015 31-40 Candidates proposed for Membership (MNAMS) on passing DNB Examination 41-48 Fellows/Members on rolls of the Academy 49 Nominations of Medical Scientists for Orations and Awards – 2015-16 50-54 Golden Jubilee Commemoration Award Lecture 55 Lifetime Achievement Award for the year 2015 55 Maintenance of Building 55-56 Publication of Annals 57-59 Obituary 60 Text of the address by the President Dr. Mukund Sadashiv Joshi, delivered at the Annual Convocation on 17th October, 2015 at Patna, Bihar (Annexure I) 61 Text of the address by the Chief Guest Dr. Ram Nath Kovind, Governor of Bihar, GoI, at the Annual Convocation on 17th October 2015, at Patna (Annexure II) 62-63 B. Academic Report 65 Continuing Medical Education Programme 67 Report of activities April 1, 2015 - March 31, 2016 67-71 State-wise distribution of Extramural CME Programmes 72 Extramural CME Programmes of NAMS Chapters (Annexure III) 73-74 Report on Extramural CME Programmes (Annexure IV) 75-87 The Medical Scientists’ Exchange Programmes (Health Manpower Development) 88 Report on Intramural CME Programmes (Annexure V) 89-96 NAMS Chapters (Annexure VI) 97-100 Emeritus Professors of NAMS 101-103 NAMS Website 104 C.