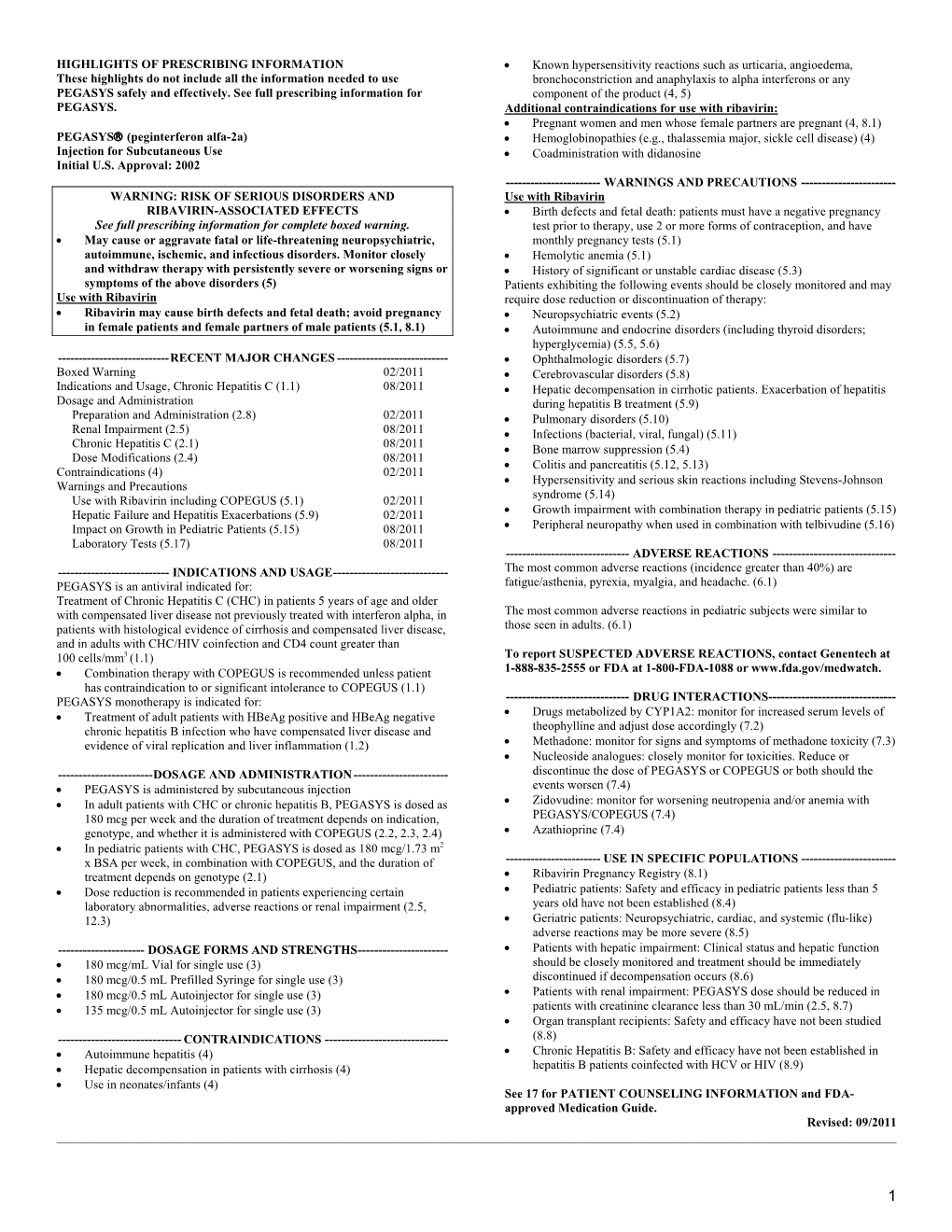
Pegasys (Peginterferon Alfa-2A) Label
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Induction of a TRAIL Mediated Suicide Program by Interferon Alpha in Primary E€Usion Lymphoma
Oncogene (2001) 20, 7029 ± 7040 ã 2001 Nature Publishing Group All rights reserved 0950 ± 9232/01 $15.00 www.nature.com/onc Induction of a TRAIL mediated suicide program by interferon alpha in primary eusion lymphoma Ngoc L Toomey1,4, Vadim V Deyev2,4, Charles Wood3, Lawrence H Boise2, Duncan Scott1, Lei Hua Liu1, Lisa Cabral1, Eckhard R Podack2, Glen N Barber2 and William J Harrington Jr*,1 1Department of Medicine University of Miami School of Medicine, Miami, Florida, FL 33136, USA; 2Department of Microbiology and Immunology, University of Miami School of Medicine, Miami, Florida, FL 33136, USA; 3School of Biological Sciences, University of Nebraska, Lincoln, Nebraska, NE 68588, USA Gammaherpes viruses are often detected in lymphomas Virus (EBV) or Human Herpes Virus Type 8 (HHV-8) arising in immunocompromised patients. We have found have been isolated from lymphomas found in im- that Azidothymidine (AZT) alone induces apoptosis in munosuppressed organ transplant recipients, children Epstein Barr Virus (EBV) positive Burkitt's lymphoma with hereditary immunode®ciencies and patients with (BL) cells but requires interferon alpha (IFN-a) to induce acquired immunode®ciency (AIDS) (Swinnen, 1999; apoptosis in Human Herpes Virus Type 8 (HHV-8) Goldsby and Carroll, 1998; Knowles, 1999). Many of positive Primary Eusion Lymphomas (PEL). Our these tumors can be categorized into distinct subtypes analysis of a series of AIDS lymphomas revealed that based on a variety of morphologic and molecular IFN-a selectively induced very high levels of the Death criteria. For example, AIDS associated large cell Receptor (DR) tumor necrosis factor-related apoptosis- diuse or immunoblastic lymphomas (DLCL, IBL) inducing ligand (TRAIL) in HHV-8 positive PEL lines are often EBV positive while AIDS associated Burkitt's and primary tumor cells whereas little or no induction lymphomas (BL) less frequently contain EBV (Gaidano was observed in primary EBV+ AIDS lymphomas and et al., 1994). -

Lenograstim in the Treatment of Severe Neutropenia in Patients Treated with Peg-IFN and Ribavirin
Le Infezioni in Medicina, n. 1, 21-23, 2009 Lavori originali Lenograstim in the treatment of severe neutropenia in Original articles patients treated with Peg-IFN and ribavirin: the experience of a single hepatology unit Trattamento mediante lenograstim della neutropenia grave in corso di terapia con Peg-IFN e ribavirina: esperienza di una singola unità di epatologia Luciano Tarantino1, Annunziata De Rosa2, Orsola Tambaro1, Carmine Ripa1, Marta Celiento3, Antonio Schiano1 1Unità di Epatologia ed Ecointerventistica, Ospedale San Giovanni di Dio, Frattamaggiore, Napoli, Italy; 2AOU “Federico II”, Dipartimento di Malattie Infettive, ASL NA 2, Napoli, Italy; 3AOU “Federico II”, Dipartimento di Chirurgia Generale e Geriatria, ASL NA 2, Napoli, Italy n INTRODUCTION doses of 80 mcg s.c./week of Peg-IFN 2b and 1200 mg/die of ribavirin. We checked quanti- he standard treatment of chronic hepatitis C tative HCV- RNA at 12 and 48 weeks of treat- (ECA C) is pegylated interferon-alpha (Peg- ment. Every two weeks, two days before ad- TIFN ) combined with ribavirin [1]. One of the ministration of the weekly dose of Peg-IFN 2b most frequent causes of suspension of therapy or all patients had blood count and liver enzyme reduction of the doses of Peg-IFN is haemato- tests. Patients with absolute neutrophil counts toxicity, which includes anaemia and/or neu- <900 cells/mmc started on lenograstim (263 tropenia and/or thrombocytopenia [2]. The use µg) 24 hours before administration of Peg- of growth factors (G-CSF) in responder patients IFNα 2b (Figure 1). Indication for administer- allows effective doses of Peg-IFN and RIBA to be ing lenograstim was early viral response kept stable [3]. -

Effectiveness and Safety of Sofosbuvir Plus Ribavirin for the Treatment of HCV Genotype 2 Infection
Hepatology ORIGINAL ARTICLE Effectiveness and safety of sofosbuvir plus ribavirin Gut: first published as 10.1136/gutjnl-2016-311609 on 13 July 2016. Downloaded from for the treatment of HCV genotype 2 infection: results of the real-world, clinical practice HCV-TARGET study Tania M Welzel,1 David R Nelson,2 Giuseppe Morelli,2 Adrian Di Bisceglie,3 Rajender K Reddy,4 Alexander Kuo,5 Joseph K Lim,6 Jama Darling,7 Paul Pockros,8 Joseph S Galati,9 Lynn M Frazier,10 Saleh Alqahtani,11 Mark S Sulkowski,11 Monika Vainorius,7 Lucy Akushevich,7 Michael W Fried,7 Stefan Zeuzem,1 for the HCV-TARGET Study Group ► Additional material is ABSTRACT published online only. To view Objective Due to a high efficacy in clinical trials, Significance of this study please visit the journal online sofosbuvir (SOF) and ribavirin (RBV) for 12 or 16 weeks (http://dx.doi.org/10.1136/ gutjnl-2016-311609). is recommended for treatment of patients with HCV genotype (GT) 2 infection. We investigated safety and What is already known on this subject? For numbered affiliations see effectiveness of these regimens for GT2 in HCV-TARGET ▸ fi end of article. Due to a high ef cacy in clinical trials, the participants. all-oral combination of sofosbuvir (SOF) and Correspondence to Design HCV-TARGET, an international, prospective ribavirin (RBV) for 12 weeks is currently Dr Tania Mara Welzel, JW observational study evaluates clinical practice data on considered standard of care in patients with Goethe University Hospital, novel antiviral therapies at 44 academic and 17 HCV genotype 2 (GT2) infection. -

Porvac® Subunit Vaccine E2-CD154 Induces Remarkable Rapid Protection Against Classical Swine Fever Virus
Article Porvac® Subunit Vaccine E2-CD154 Induces Remarkable Rapid Protection against Classical Swine Fever Virus Yusmel Sordo-Puga 1, Marisela Suárez-Pedroso 1 , Paula Naranjo-Valdéz 2, Danny Pérez-Pérez 1, Elaine Santana-Rodríguez 1, Talia Sardinas-Gonzalez 1, Mary Karla Mendez-Orta 1, Carlos A. Duarte-Cano 1, Mario Pablo Estrada-Garcia 1 and María Pilar Rodríguez-Moltó 1,* 1 Animal Biotechnology Department, Center for Genetic Engineering and Biotechnology, P.O. Box 6162, Havana 10600, Cuba; [email protected] (Y.S.-P.); [email protected] (M.S.-P.); [email protected] (D.P.-P.); [email protected] (E.S.-R.); [email protected] (T.S.-G.); [email protected] (M.K.M.O.); [email protected] (C.A.D.); [email protected] (M.P.E.) 2 Central Laboratory Unit for Animal Health (ULCSA), Havana 11400, Cuba; [email protected] * Correspondence: [email protected]; Tel.: +53-7-2504419 Abstract: Live attenuated C-strain classical swine fever vaccines provide early onset protection. These vaccines confer effective protection against the disease at 5–7 days post-vaccination. It was previously reported that intramuscular administration of the Porvac® vaccine protects against highly virulent Citation: Sordo-Puga, Y.; classical swine fever virus (CSFV) “Margarita” strain as early as seven days post-vaccination. In Suárez-Pedroso, M.; Naranjo-Valdéz, order to identify how rapidly protection against CSFV is conferred after a single dose of the Porvac® P.; Pérez-Pérez, D.; subunit vaccine E2-CD154, 15 swine, vaccinated with a single dose of Porvac®, were challenged Santana-Rodríguez, E.; 3 intranasally at five, three, and one day post-vaccination with 2 × 10 LD50 of the highly pathogenic Sardinas-Gonzalez, T.; Mendez-Orta, Cuban “Margarita” strain of the classical swine fever virus. -

Anti-Inflammatory Effects of Amantadine and Memantine
Journal of Personalized Medicine Communication Anti-Inflammatory Effects of Amantadine and Memantine: Possible Therapeutics for the Treatment of Covid-19? Félix Javier Jiménez-Jiménez 1,* , Hortensia Alonso-Navarro 1 , Elena García-Martín 2 and José A. G. Agúndez 2 1 Section of Neurology, Hospital Universitario del Sureste, Arganda del Rey, E-28500 Madrid, Spain; [email protected] 2 University Institute of Molecular Pathology Biomarkers, UNEx. ARADyAL Instituto de Salud Carlos III, E-10071 Cáceres, Spain; [email protected] (E.G.-M.); [email protected] (J.A.G.A.) * Correspondence: [email protected]; Tel.: +34-636968395 Received: 2 October 2020; Accepted: 6 November 2020; Published: 9 November 2020 Abstract: We have reviewed current data on the anti-inflammatory effects of amantadine and memantine in clinical and in vivo models of inflammation, and we propose that these effects have potential interest for the treatment of the SARS-CoV-2 infection (COVID-19 disease). To that end, we performed a literature search using the PubMed Database from 1966 up to October 31 2020, crossing the terms “amantadine” and “memantine” with “inflammation” and “anti-inflammatory”. Amantadine and/or memantine have shown anti-inflammatory effects in chronic hepatitis C, in neuroinflammation induced by sepsis and by lipopolysaccharides, experimental models of multiple sclerosis, spinal cord injury, and respiratory diseases. Since the inflammatory response is one of the main pathogenetic mechanisms in the progression of the SARS-CoV-2 infection, anti-inflammatory effects of amantadine and memantine could be hypothetically useful in the treatment of this condition. This potential utility deserves further research. Keywords: amantadine; memantine; anti-inflammatory effects; SARS-Cov-2; COVID-19; therapy 1. -

Age- and Gender-Specific Modulation of Serum Osteopontin and Interferon-Α by Osteopontin Genotype in Systemic Lupus Er
Genes and Immunity (2009) 10, 487–494 & 2009 Macmillan Publishers Limited All rights reserved 1466-4879/09 $32.00 www.nature.com/gene ORIGINAL ARTICLE Age- and gender-specific modulation of serum osteopontin and interferon-a by osteopontin genotype in systemic lupus erythematosus SN Kariuki1, JG Moore1, KA Kirou2,MKCrow2, TO Utset1 and TB Niewold1 1Section of Rheumatology, University of Chicago, Chicago, IL, USA and 2Mary Kirkland Center for Lupus Research, Hospital for Special Surgery, New York, NY, USA Osteopontin (OPN) is a multifunctional cytokine involved in long bone remodeling and immune system signaling. Additionally, OPN is critical for interferon-a (IFN-a) production in murine plasmacytoid dendritic cells. We have previously shown that IFN-a is a heritable risk factor for systemic lupus erythematosus (SLE). Genetic variants of OPN have been associated with SLE susceptibility, and one study suggests that this association is particular to men. In this study, the 3 0 UTR SLE-risk variant of OPN (rs9138C) was associated with higher serum OPN and IFN-a in men (P ¼ 0.0062 and P ¼ 0.0087, respectively). In women, the association between rs9138 C and higher serum OPN and IFN-a was restricted to younger subjects, and risk allele carriers showed a strong age-related genetic effect of rs9138 genotype on both serum OPN and IFN-a (Po0.0001). In African- American subjects, the 5 0 region single nucleotide polymorphisms, rs11730582 and rs28357094, were associated with anti- RNP antibodies (odds ratio (OR) ¼ 2.9, P ¼ 0.0038 and OR ¼ 3.9, P ¼ 0.021, respectively). Thus, we demonstrate two distinct genetic influences of OPN on serum protein traits in SLE patients, which correspond to previously reported SLE-risk variants. -

Antiviral Agents Active Against Influenza a Viruses
REVIEWS Antiviral agents active against influenza A viruses Erik De Clercq Abstract | The recent outbreaks of avian influenza A (H5N1) virus, its expanding geographic distribution and its ability to transfer to humans and cause severe infection have raised serious concerns about the measures available to control an avian or human pandemic of influenza A. In anticipation of such a pandemic, several preventive and therapeutic strategies have been proposed, including the stockpiling of antiviral drugs, in particular the neuraminidase inhibitors oseltamivir (Tamiflu; Roche) and zanamivir (Relenza; GlaxoSmithKline). This article reviews agents that have been shown to have activity against influenza A viruses and discusses their therapeutic potential, and also describes emerging strategies for targeting these viruses. HXNY In the face of the persistent threat of human influenza A into the interior of the virus particles (virions) within In the naming system for (H3N2, H1N1) and B infections, the outbreaks of avian endosomes, a process that is needed for the uncoating virus strains, H refers to influenza (H5N1) in Southeast Asia, and the potential of to occur. The H+ ions are imported through the M2 haemagglutinin and N a new human or avian influenza A variant to unleash a (matrix 2) channels10; the transmembrane domain of to neuraminidase. pandemic, there is much concern about the shortage in the M2 protein, with the amino-acid residues facing both the number and supply of effective anti-influenza- the ion-conducting pore, is shown in FIG. 3a (REF. 11). virus agents1–4. There are, in principle, two mechanisms Amantadine has been postulated to block the interior by which pandemic influenza could originate: first, by channel within the tetrameric M2 helix bundle12. -

Ribavirin) Tablets Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------------ CONTRAINDICATIONS ----------------------------- These highlights do not include all the information needed to use • Pregnant women and men whose female partners are pregnant (4, 5.1, COPEGUS safely and effectively. See full prescribing information for 8.1) COPEGUS. • Hemoglobinopathies (4) • Coadministration with didanosine (4, 7.1) ® COPEGUS (ribavirin) Tablets Initial U.S. Approval: 2002 COPEGUS in combination with PEGASYS is contraindicated in patients with: WARNING: RISK OF SERIOUS DISORDERS AND RIBAVIRIN • Autoimmune hepatitis (4) ASSOCIATED EFFECTS • Hepatic decompensation in cirrhotic patients (4, 5.3) See full prescribing information for complete boxed warning. • Ribavirin monotherapy, including COPEGUS, is not effective for ----------------------- WARNINGS AND PRECAUTIONS ---------------------- the treatment of chronic hepatitis C virus infection (Boxed • Birth defects and fetal death with ribavirin: Do not use in pregnancy and Warning). for 6 months after treatment. Patients must have a negative pregnancy • The hemolytic anemia associated with ribavirin therapy may result test prior to therapy, use at least 2 forms of contraception and undergo in worsening of cardiac disease and lead to fatal and nonfatal monthly pregnancy tests (4, 5.1, 8.1) myocardial infarctions. Patients with a history of significant or unstable cardiac disease should not be treated with COPEGUS (2.3, PEGASYS/COPEGUS: Patients exhibiting the following conditions should be 5.2, 6.1). closely monitored and may require dose reduction or discontinuation of • Significant teratogenic and embryocidal effects have been therapy: demonstrated in all animal species exposed to ribavirin. Therefore, • Hemolytic anemia may occur with a significant initial drop in COPEGUS is contraindicated in women who are pregnant and in hemoglobin. -

Interferon-Γ Enhances Interleukin 12 Production in Rheumatoid Synovial
Interferon-γ Enhances Interleukin 12 Production in Rheumatoid Synovial Cells via CD40-CD154 Dependent and Independent Pathways MINETAKE KITAGAWA, HIROSHI SUZUKI, YOSHIHIRO ADACHI, HIROSHI NAKAMURA, SHINICHI YOSHINO, and TAKAYUKI SUMIDA ABSTRACT. Objective. To determine the role of interferon-γ (IFN-γ) in CD40-CD154 dependent production of interleukin 12 (IL-12) by synovial cells of patients with rheumatoid arthritis (RA). Methods. We examined the effects of IFN-γ, tumor necrosis factor-α (TNF-α), and granulocyte- macrophage colony stimulating factor (GM-CSF) on CD40 expression on CD68+ synovial macrophage-lineage cells (SMC). The effects of IFN-γ and soluble CD154 (sCD154) on IL-12 production by RA synovial cells were determined by ELISA. Results. CD68+ SMC expressed substantial levels of CD40. IFN-γ, but not TNF-α or GM-CSF, markedly upregulated CD40 expression on CD68+ SMC. IFN-γ also dose dependently increased IL- γ 12 production by synovial cells. The effects of IFN- on CD40 expression (EC50 = 127.4 U/ml) were observed at a concentration 19 times lower than the effects on IL-12 production (EC50 = 6.8 U/ml). Treatment with IFN-γ at a concentration low enough to augment CD40 expression but not IL-12 production enhanced spontaneous IL-12 production synergy with sCD154. The synergistic enhance- ment of spontaneous IL-12 production was abrogated by CD40-Fc. In contrast, IL-12 production induced by high concentration of IFN-γ was not neutralized by CD40-Fc. Conclusion. IFN-γ enhanced IL-12 production via both CD40-CD154 dependent and independent pathways in RA synovium. IFN-γ may play a crucial role in the development of RA synovitis through regulation of IL-12 production. -

Combination Therapy for Chronic Hepatitis B: Current Indications
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Curr Hepatitis Rep (2011) 10:98–105 DOI 10.1007/s11901-011-0095-1 Combination Therapy for Chronic Hepatitis B: Current Indications Navin Paul & Steven-Huy Han Published online: 19 February 2011 # The Author(s) 2011. This article is published with open access at Springerlink.com Abstract Hepatitis B infection remains a major public infected adults in the United States alone and an annual health problem globally and in the United States, with financial burden of $1.3 billion [1, 2•]. Currently available significant use of healthcare resources. Several therapeu- therapeutic options include both parenteral and oral agents, tic agents active against viral and host targets are which act on various host and viral targets. These include currently available for its treatment. The success of medications such as standard interferon and pegylated combination therapy in HIV infection, which has simi- interferon (peg-interferon), which target receptors on the larities to hepatitis B in both therapeutic targets and host cell membranes, and nucleotide and nucleoside treatment options, stimulated studies on the efficacy and analogues, which inhibit HBV RNA-dependent DNA safety of various combinations of available drugs in the polymerase (lamivudine, telbivudine, entecavir, adefovir treatment of hepatitis B infection. In this review, we dipivoxil, and tenofovir disoproxil fumarate) [3]. analyze the current role of combination therapy in The availability of agents acting on different targets chronic hepatitis B infection. makes the option of combination therapy to achieve better therapeutic results particularly attractive. -

Dysregulated Interferon Response Underlying Severe COVID-19
viruses Review Dysregulated Interferon Response Underlying Severe COVID-19 LeAnn Lopez y, Peter C. Sang y, Yun Tian y and Yongming Sang * Department of Agricultural and Environmental Sciences, College of Agriculture, Tennessee State University, 3500 John A. Merritt Boulevard, Nashville, TN 37209, USA; [email protected] (L.L.); [email protected] (P.C.S.); [email protected] (Y.T.) * Correspondence: [email protected]; Tel.: +1-615-963-5183 These authors contributed equally. y Academic Editor: Andrew Davidson Received: 27 October 2020; Accepted: 9 December 2020; Published: 13 December 2020 Abstract: Innate immune interferons (IFNs), including type I and III IFNs, constitute critical antiviral mechanisms. Recent studies reveal that IFN dysregulation is key to determine COVID-19 pathogenesis. Effective IFN stimulation or prophylactic administration of IFNs at the early stage prior to severe COVID-19 may elicit an autonomous antiviral state, restrict the virus infection, and prevent COVID-19 progression. Inborn genetic flaws and autoreactive antibodies that block IFN response have been significantly associated with about 14% of patients with life-threatening COVID-19 pneumonia. In most severe COVID-19 patients without genetic errors in IFN-relevant gene loci, IFN dysregulation is progressively worsened and associated with the situation of pro-inflammation and immunopathy, which is prone to autoimmunity. In addition, the high correlation of severe COVID-19 with seniority, males, and individuals with pre-existing comorbidities will be plausibly explained by the coincidence of IFN aberrance in these situations. Collectively, current studies call for a better understanding of the IFN response regarding the spatiotemporal determination and subtype-specificity against SARS-CoV-2 infections, which are warranted to devise IFN-related prophylactics and therapies. -

Interplay Between Hepatitis D Virus and the Interferon Response
viruses Review Interplay between Hepatitis D Virus and the Interferon Response Zhenfeng Zhang 1 and Stephan Urban 1,2,* 1 Department of Infectious Diseases, Molecular Virology, University Hospital Heidelberg, 69120 Heidelberg, Germany; [email protected] 2 German Centre for Infection Research (DZIF), Partner Site Heidelberg, 69120 Heidelberg, Germany * Correspondence: [email protected]; Tel.: +49-6221-564-902 Received: 27 October 2020; Accepted: 18 November 2020; Published: 20 November 2020 Abstract: Chronic hepatitis D (CHD) is the most severe form of viral hepatitis, with rapid progression of liver-related diseases and high rates of development of hepatocellular carcinoma. The causative agent, hepatitis D virus (HDV), contains a small (approximately 1.7 kb) highly self-pairing single-strand circular RNA genome that assembles with the HDV antigen to form a ribonucleoprotein (RNP) complex. HDV depends on hepatitis B virus (HBV) envelope proteins for envelopment and de novo hepatocyte entry; however, its intracellular RNA replication is autonomous. In addition, HDV can amplify HBV independently through cell division. Cellular innate immune responses, mainly interferon (IFN) response, are crucial for controlling invading viruses, while viruses counteract these responses to favor their propagation. In contrast to HBV, HDV activates profound IFN response through the melanoma differentiation antigen 5 (MDA5) pathway. This cellular response efficiently suppresses cell-division-mediated HDV spread and, to some extent, early stages of HDV de novo infection, but only marginally impairs RNA replication in resting hepatocytes. In this review, we summarize the current knowledge on HDV structure, replication, and persistence and subsequently focus on the interplay between HDV and IFN response, including IFN activation, sensing, antiviral effects, and viral countermeasures.