Clinical Papercan Ambulance Telephone Triage Using NHS
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

NHS Ambulance Services
Report by the Comptroller and Auditor General NHS England NHS Ambulance Services HC 972 SESSION 2016-17 26 JANUARY 2017 Our vision is to help the nation spend wisely. Our public audit perspective helps Parliament hold government to account and improve public services. The National Audit Office scrutinises public spending for Parliament and is independent of government. The Comptroller and Auditor General (C&AG), Sir Amyas Morse KCB, is an Officer of the House of Commons and leads the NAO, which employs some 785 people. The C&AG certifies the accounts of all government departments and many other public sector bodies. He has statutory authority to examine and report to Parliament on whether departments and the bodies they fund have used their resources efficiently, effectively, and with economy. Our studies evaluate the value for money of public spending, nationally and locally. Our recommendations and reports on good practice help government improve public services, and our work led to audited savings of £1.21 billion in 2015. NHS England NHS Ambulance Services Report by the Comptroller and Auditor General Ordered by the House of Commons to be printed on 24 January 2017 This report has been prepared under Section 6 of the National Audit Act 1983 for presentation to the House of Commons in accordance with Section 9 of the Act Sir Amyas Morse KCB Comptroller and Auditor General National Audit Office 23 January 2017 HC 972 | £10.00 This report reviews the progress that the NHS ambulance services have made since our previous report and that of the Committee of Public Accounts. -

Enc E Isle of Wight NHS Trust Board Performance Report 2015/16 March 16
Enc E Isle of Wight NHS Trust Board Performance Report 2015/16 March 16 Title Isle of Wight NHS Trust Board Performance Report 2015/16 Sponsoring Executive Director Chris Palmer - Executive Director of Financial & Human Resources Author(s) Iain Hendey - Deputy Director of Information Purpose To update the Trust Board regarding progress against key performance measures and highlight risks and the management of these risks. Action required by the Board: Receive X Approve Previously considered by (state date): Trust Executive Committee Mental Health Act Scrutiny Committee Audit and Corporate Risk Committee Renumination and Nominations Committee Charitable Funds Committee Quality Governance Committee Finance, Information, Investment & Workforce Committee 29/03/2016 Please add any other committees below as needed Other (please state) Staff, stakeholder, patient and public engagement: Executive Summary: This paper sets out the key performance indicators by which the Trust is measuring its performance in 2015/16. A more detailed executive summary of this report is set out on page 4. For following sections – please indicate as appropriate: Trust Vision: Quality care for everyone,everytime Excellent patient care; Working with others to keep improving our services; A positive experience for patients, service users and staff; Trust Goals: Skilled and capable staff; Cost effective, sustainable services Principal Risks (please enter applicable BAF references – eg 1.1; 1.6) Assurance Level (shown on BAF) £ Red £ Amber £ Green Legal implications, regulatory -

Trust Board Papers
Trust Board Papers Isle of Wight NHS Trust Board Meeting in Public (Part 1) to be held on Wednesday 7th December 2016 at 9.30am - Conference Room, School of Health Sciences (South Hospital) St. Mary’s Hospital, Parkhurst Road, NEWPORT, Isle of Wight, PO30 5TG Staff and members of the public are welcome to attend the meeting. Refuse Store Emergency Generator 32 48 PARENT & CHILD & PARENT 49 S I YS L A I D 32 . 30 O N 5 DOCTOR ON CALL 32 30 28 47 TENNIS 29 COURT 52 31 Bund wall El Sub Sta KEEP Medical Vacuum Plant Room Medical Gas Store Refuse 37 Sub-Station "A". Electrical Main Intake CLEAR M/C 46 Solent El Sub Sta Medina El 21 26 Sub Sta 51 24 25 43 50 22 23 44 33 43 15 KEEP Sevenacres NO EXIT CLEAR 34 CHEMO POINT 39 DROP OFF DROP OFF 41 Shelter ONLY AND 14.9m WAITING 27 Margham House El Sub Sta 35 20 35 Upper St Cross Farm 20 Pond 20 36 PAVING SMALL TREES & BUSHES SLABS Pond 53 IN THIS AREA Block Numbers And BuildingsRadio Station List PAVING GRASS 8 to 11 SLABS SMALL TREES & BUSHES TARMAC IN THIS AREA GRASS 01 AMBULANCE STATION GRASS TREE STUMPS 02 SOCIAL CLUB 20 18.37 ramp 03 HELI PAD FIRE APPLIANCE KEEP AREA CLEAR AREA KEEP APPLIANCE FIRE 04 AMBULANCE HQ, RESEARCH DEPT.31 S4 18.954 12 GRASS 20 13.1m & TRANSPORT S1 KEEP AREA CLEAR AREA KEEP FIRE APPLIANCE FIRE 05 MAIN BOILERHOUSE FIRE APPLIANCE KEEP AREA CLEAR 06 MAINDodnor SOUTH Park HOSPITAL BUILDING 29 07 WHEELCHAIR SERVICES GRASS Sedum / Grass 08 LAIDLAW DAY UNIT GRASS 09 ALMONDGATE/CHERRYGATE6 MEDINA WAY 03 Pond path 10 PODIATRY/ORTHOTICS/SPEECH THERAPY 16 CAR PARK 11 ALLERGY RESEARCH CENTRE 12 HOLLY HOUSE 27 13 DIABETIC CENTRE 14 BREAST SCREENING UNIT6 El Sub Sta 15 BREAST CARE UNIT 16 SCHOOL OF NURSING 1 17 THE COTTAGE 18 VECTASEARCH UNIT 01 19 SOUTH PUBLIC WC's/GENERATOR 25 52 20 MAIN HOSPITAL 23 El Sub Sta 21 HV ELECTRICAL INTAKE 22 MOTTISTONE BLOCK 15 23 B BLOCK 13 19 PCs 50 24 PHYSIO/MANAGEMENT BLOCK 02 60 25 A BLOCK 15.2m 26 MFU/ORTHODONTICS 27 DAY PROCEDURES UNIT 9 28 MATERNITY 29 LINEN SERVICES/MORTUARY 30 SEXUAL HEALTH SERVICE 06 & IT DEPARTMENT / SERVER ROOM 15 06 06 04 48a 16 31 MED. -

List of Designated Bodies Below You Will Find an A-Z List of Designated Bodies (DB), Their Responsible Officer (RO) and the DB Email Address That We Hold
List of designated bodies Below you will find an A-Z list of designated bodies (DB), their Responsible Officer (RO) and the DB email address that we hold. Please take care when using the following email addresses, especially if you intend to send confidential information. Sometimes the email addresses we hold become out of date. Please check with the intended recipient if in doubt. If there is no email address it is because we do not hold one. We have approved a number of suitable persons. You can find our list of GMC approved suitable persons at: http://www.gmc-uk.org/Revalidation___Suitable_Person_details___DC4964.pdf_53912287.pdf We update this list on a weekly basis. This list was last updated on 20 September 2021. Details of responsible officers are provided to the GMC by each designated body. The GMC is not responsible for the appointment of responsible officers. If you have any queries regarding the responsible officer details for an individual designated body please contact the designated body. RO Title RO First Name RO Last Name RO UID DB Email Address 21st Century Clinic Ltd Dr Philip Dobson 3279643 [email protected] 4 Ways Healthcare Ltd Dr John Timmis 2273581 [email protected] 4Recruitment Services Ltd Dr Timothy Nuthall 3691263 [email protected] 58 Queen Square Mr Nigel Mercer 2626770 [email protected] Abicare Health Solutions Ltd Dr Harrison Offiong 7059321 [email protected] ABL Health Ltd Dr Francis Andrews 3334715 [email protected] About Health Ltd Dr Uma Krishnamoorthy 4754750 [email protected] -
4Th March 2015.Pdf
Trust Board Papers Isle of Wight NHS Trust Board Meeting in Public (Part 1) to be held on Wednesday 4th March 2015 at 9.30am - Conference Room, School of Health Sciences (South Hospital) St. Mary’s Hospital, Parkhurst Road, NEWPORT, Isle of Wight, PO30 5TG Staff and members of the public are welcome to attend the meeting. Key Trust Strategic Objectives & Critical Success Factors 2014/15 Strategic Objectives Critical Success Factors 1. QUALITY - To achieve the highest CSF 1 - Improve the CSF2 - Improve clinical possible quality standards for our experience and effectiveness, safety and patients in terms of outcomes, satisfaction of our outcomes for our safety and positive experience of patients, their carers, our patients care partners and staff 2. CLINICAL STRATEGY - To deliver CSF3 - Continuously CSF4 - Develop our the Trust’s clinical strategy, develop and successfully relationships with key integrating service delivery within implement our Integrated stakeholders to our organisation and with our Business Plan continually build on our partners, and providing services integration across health locally wherever clinically appropriate and cost effective and between health, social care and the voluntary/third sector, collectively delivering a sustainable local system 3. RESILIENCE - Build the resilience CSF5 - Demonstrate CSF6 - Develop our of our services and organisation, robust linkages with our quality governance and through partnerships within the NHS partners, the local financial management NHS, with social care and with the authority, the third sector systems and processes private and voluntary/third sectors and commercial entities to deliver performance for the clear benefit of our that exceeds the patients standards set down for Foundation Trusts 4. -

Fin Cupid Number Eligible Company Account Name
FIN CUPID NUMBER ELIGIBLE COMPANY ACCOUNT NAME POSTAL CODE Z4268 119045570 3M UNITED KINGDOM PLC RG12 8HT Z6507 117348112 AAH PHARMACEUTICALS LTD CV2 2TX 2693 125824576 ADMIRAL INSURANCE COMPANY LIMITED CF10 3AZ P0412 113833308 AEGON & OTHER SUBSIDIARY COMPANIES EH12 9SE 995 118956328 AGGREGATE INDUSTRIES PLC LE67 1TL R0214 3388117 AGUSTA WESTLAND BA20 2YB 38476 300487403 AIRBUS OPERATIONS LTD BS99 7AR N2462 137865155 AIREDALE N H S TRUST BD20 6TD S7651 119990226 ALCATEL LUCENT TELECOM LTD SL6 2PJ Z1513 117246934 ALD AUTOMOTIVE BS16 7LB 51747 350223183 ALLIANZ GLOBAL ASSISTANCE GU1 1DB Z1789 116068464 ALLIANZ MANAGEMENT SERVICES LTD GU1 1DB 22542 191070636 ANEURIN BEVAN HEALTH BOARD NP44 8YN P2452 105376615 ASSOCIATED BRITISH PORTS DN40 2LZ 27376 213569197 ASTRAZENECA UK PLC SK10 4TF Z1252 120026764 AVIS BUDGET UK RG12 2EW Z4500 5265546 AVIVA CENTRAL SERVICES UK LTD NR7 0WF 9383 131164647 AYRSHIRE & ARRAN COMMUNITY HEALTH DIVISION KA6 6AB R0198 105599696 BABCOCK INTERNATIONAL LTD BS32 4AQ 31632 131965694 BAE SYSTEMS PLC BB2 7LF 9140 136846638 BARKING, HAVERING & REDBRIDGE UNIVERSITY NHS TRUST RM7 0AG 15032 143134756 BARLOWS (UK) LTD SY14 8LU T1497 118959168 BARRATT DEVELOPMENTS PLC M16 9HQ 9352 136694545 BARTS HEALTH NHS TRUST E1 1BB Z5027 119045908 BEDFORDSHIRE POLICE FORCE MK42 8AX 8931 131506583 BELFAST HEALTH & SOCIAL CARE TRUST BT9 7AB 8927 128138327 BIRMINGHAM & SOLIHULL MENTAL HEALTH N H S TRUST B15 2QZ 1462 123177371 BIRMINGHAM CITY COUNCIL B9 4BA 54586 354018461 BIRMINGHAM COMMUNITY HEALTHCARE TRUST NHS PR2 9QB 8924 130116070 -

Operational Productivity and Performance in English NHS Ambulance Trusts: Unwarranted Variations
Operational productivity and performance in English NHS Ambulance Trusts: Unwarranted variations Foreword by Lord Carter of Coles The ambulance service plays a pivotal role in saving lives and has a major influence on the flow of patients to hospitals. Trusts answered 10 million 999 calls and responded to over seven million separate incidents last year. Nine out of 10 of these calls were not life-threatening but were lower acuity calls, often involving elderly patients, and nearly 60% of responses resulted in a patient being conveyed to A&E. Over two million patients brought to A&E were admitted to wards and at any one time 40% of all patients in hospital beds in England will have been taken to hospital in an ambulance. The speed of response to stroke or cardiac arrest victims can be the difference between life and death. Ambulance services are also at the forefront of responding to major incidents. The tragic events at Manchester Arena last year saw the first call to the ambulance service at 22.32, one minute after the bomb exploded. An advanced paramedic, self-deployed, arrived on scene 10 minutes later. In this review I have been struck by the dedication of all those working in the ambulance service. The Five Year Forward View outlines an ambition to place care closer to home, but further work is needed to make this a reality. In my review of community health services, I identified that elderly patients, whose average length of stay in hospital for a non- elective admission is 13 days, needed a focused approach. -

Department of Health NHS Isle
Department family Entity Date Expense Type Expense area Supplier Transaction numberAP Amount (£) Department of Health NHS Isle Of Wight CCG 30/09/2020 Clinical&Medical-Independent Sector COMMUNITY SERVICES ACTION ON HEARING LOSS 33895538 38,985.00 Department of Health NHS Isle Of Wight CCG 30/09/2020 Clinical&Medical-Independent Sector COMMUNITY SERVICES AGE UK ISLE OF WIGHT 33972922 76,000.00 Department of Health NHS Isle Of Wight CCG 30/09/2020 Sterile Products PRESCRIBING AMCARE LTD 33828493 70,124.09 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS DES Minor Surgery PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 583.33 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS Global Sum PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 44,562.00 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS PCN DES Participation PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 871.06 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS Prem Notional Rent PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 1,916.67 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS Prem Rates PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 862.00 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS Prem Water Rates PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 36.99 Department of Health NHS Isle Of Wight CCG 30/09/2020 C&M-GMS QOF Aspiration PRC DELEGATED CO-COMMISSIONING ARGYLL HOUSE SURGERY 33959557 4,876.26 Department of Health NHS -

Stakeholder List PDF 47 KB
Decision making and mental capacity Stakeholders ABL Health Acorns Children's Hospice Action for Children Action on Elder Abuse Action on Hearing Loss ADFAM Advantage Accreditation Age UK All of Us Alzheimer's Research UK Alzheimer's Society Amberley Lodge Care Home with Nursing ARU Homecare Association of Chartered Physiotherapists for People with Learning Disabilities Association of Chartered Physiotherapists in Oncology and Palliative Care Association of Directors of Children's Services Association of Directors of Public Health Association of Independent Healthcare Organisations Association of Mental Health Providers Association of Police and Crime Commissioners AT-Autism Autistica Bangor University BAPIO Barnardo's Barnsley Hospice Barnsley Hospital NHS Foundation Trust Beat Beds and Luton Fair Play Behind The Mask Foundation Belfast Health and Social Care Trust Berkshire Healthcare NHS Foundation Trust Bespoke Supported Living Birmingham Women’s NHS Foundation Trust Bluebird Care Boehringer Ingelheim Ltd Bolton Council Bournemouth University Dementia Institute Brainstrust bridgewater nhs British Association for Behavioural & Cognitive Psychotherapies British Association for Counselling and Psychotherapy British Association of Brain Injury Case Managers British Association of Social Workers British Dental Industry Association British Institute of Learning Disabilities British Psychological Society British Psychological Society British Society of Gerodontology Broad Hey Limted Brookdale care Buckinghamshire Disability Service Camphill Families and Friends Care England Care Quality Commission Care Right Now Carers Trust Carers Trust Carers UK CAUSE Central & North West London NHS Foundation Trust Central and Cecil Centre for Mental Health Centre for Social Work Practice Cerebra Ceretas Challenging Behaviour Foundation CHANGE Children England CIS'ters CLASP Charity Cochrane UK College of Mental Health Pharmacy Coma and Disorders of Consciousness Research Centre Community Action Bradford & District Community Choice and Inclusion Community Links Trust Ltd. -

UKCPAPIN COVID-19 Survey
15/11/2020 UKCPAPIN COVID-19 Survey UKCPAPIN COVID-19 Survey The UKCPA PIN committee invite infection/antimicrobial pharmacists to complete this short survey which is open until 10 June The purpose of this survey is to understand: * the impact of the COVID-19 pandemic on antimicrobial stewardship, * what support you believe would be helpful from UKCPAPIN or other relevant bodies The survey should take approximately 12 minutes to complete. Ideally we are seeking one answer per trust but if you are unsure if another colleague has completed, please do complete. Please try to answer all questions so we can understand need and how to support or advocate for support. We will aim to publish the findings to share knowledge and support advocating for our speciality. Individual Trust names or contributors will not linked to their responses within publications. Thank you in advance for your important contribution UKCPAPIN committee in collaboration with Association of Scottish Antimicrobial Pharmacists All Wales Antimicrobial Pharmacists Group Northern Ireland Regional Antimicrobial Pharmacists Network * Required Consent 1. The survey is completely voluntary and part of UKCPA Pharmacy Infection Network support provision. You have the right to refuse to answer questions or withdraw at any time. By proceeding to the next page: I consent to UKCPAPIN collecting and using the information about me that I voluntarily provide for the purposes of the survey I have read, understand and agree to the information provided above * Mark only one oval. Yes No Organisation Information 1/29 15/11/2020 UKCPAPIN COVID-19 Survey 2. Which UK country is your organisation in? * Mark only one oval. -
FTSU-Index-Report-2021
Freedom to Speak Up Index Report 2021 1 Contents Foreword ................................................................................................................... 3 Key Findings .............................................................................................................. 6 Introduction .............................................................................................................. 7 Summary of results .................................................................................................. 9 A. FTSU Index – National Averages ......................................................................... 9 B. FTSU Index – By region ..................................................................................... 12 C. FTSU Index – By trust type ................................................................................ 13 D. Trusts with the highest FTSU Index scores ......................................................... 13 E. Trusts with the greatest overall increase & decrease in FTSU Index scores ....... 14 F. FTSU Index by Ethnicity ..................................................................................... 15 G. Q18f by Ethnicity ................................................................................................. 17 H. FTSU Index by Gender ....................................................................................... 18 I. 18f by Gender...................................................................................................... 19 Conclusions -
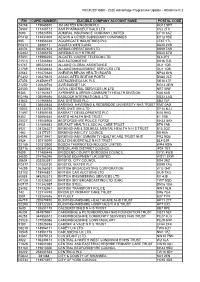
2020 Advantage Programme Update - Attachment 2
VS/UK/20/188R - 2020 Advantage Programme Update - Attachment 2 FIN CUPID NUMBER ELIGIBLE COMPANY ACCOUNT NAME POSTAL CODE Z4268 119045570 3M UNITED KINGDOM PLC RG12 8HT Z6507 117348112 AAH PHARMACEUTICALS LTD CV2 2TX 2693 125824576 ADMIRAL INSURANCE COMPANY LIMITED CF10 3AZ P0412 113833308 AEGON & OTHER SUBSIDIARY COMPANIES EH12 9SE 995 118956328 AGGREGATE INDUSTRIES PLC LE67 1TL R0214 3388117 AGUSTA WESTLAND BA20 2YB 38476 300487403 AIRBUS OPERATIONS LTD BS99 7AR N2462 137865155 AIREDALE N H S TRUST BD20 6TD S7651 119990226 ALCATEL LUCENT TELECOM LTD SL6 2PJ Z1513 117246934 ALD AUTOMOTIVE BS16 7LB 51747 350223183 ALLIANZ GLOBAL ASSISTANCE GU1 1DB Z1789 116068464 ALLIANZ MANAGEMENT SERVICES LTD GU1 1DB 22542 191070636 ANEURIN BEVAN HEALTH BOARD NP44 8YN P2452 105376615 ASSOCIATED BRITISH PORTS DN40 2LZ 27376 213569197 ASTRAZENECA UK PLC SK10 4TF Z1252 120026764 AVIS BUDGET UK RG12 2EW Z4500 5265546 AVIVA CENTRAL SERVICES UK LTD NR7 0WF 9383 131164647 AYRSHIRE & ARRAN COMMUNITY HEALTH DIVISION KA6 6AB R0198 105599696 BABCOCK INTERNATIONAL LTD BS32 4AQ 31632 131965694 BAE SYSTEMS PLC BB2 7LF 9140 136846638 BARKING, HAVERING & REDBRIDGE UNIVERSITY NHS TRUST RM7 0AG 15032 143134756 BARLOWS (UK) LTD SY14 8LU T1497 118959168 BARRATT DEVELOPMENTS PLC M16 9HQ 9352 136694545 BARTS HEALTH NHS TRUST E1 1BB Z5027 119045908 BEDFORDSHIRE POLICE FORCE MK42 8AX 8931 131506583 BELFAST HEALTH & SOCIAL CARE TRUST BT9 7AB 8927 128138327 BIRMINGHAM & SOLIHULL MENTAL HEALTH N H S TRUST B15 2QZ 1462 123177371 BIRMINGHAM CITY COUNCIL B9 4BA 54586 354018461 BIRMINGHAM