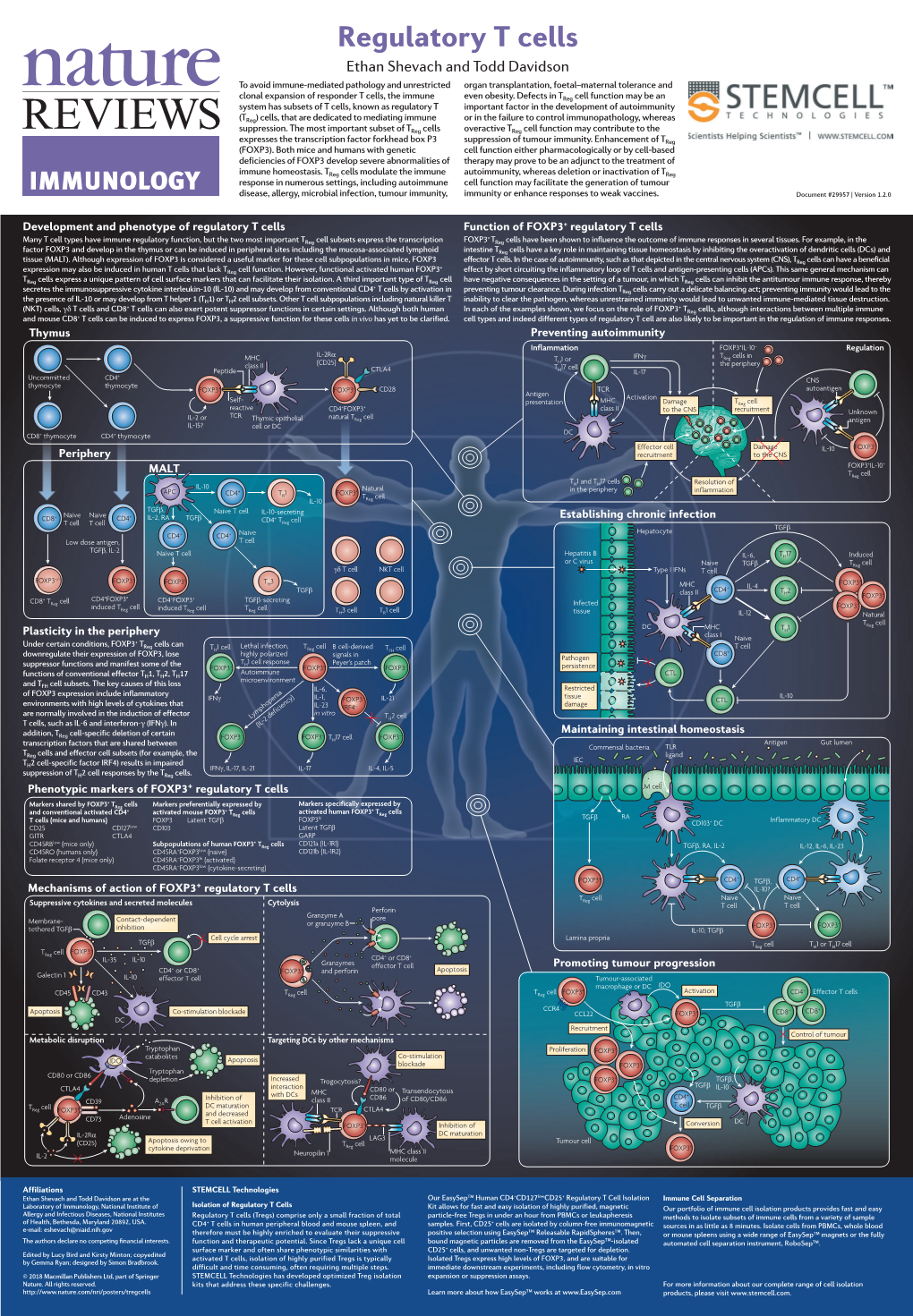
Regulatory T Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Understanding the Immune System: How It Works
Understanding the Immune System How It Works U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES NATIONAL INSTITUTES OF HEALTH National Institute of Allergy and Infectious Diseases National Cancer Institute Understanding the Immune System How It Works U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES NATIONAL INSTITUTES OF HEALTH National Institute of Allergy and Infectious Diseases National Cancer Institute NIH Publication No. 03-5423 September 2003 www.niaid.nih.gov www.nci.nih.gov Contents 1 Introduction 2 Self and Nonself 3 The Structure of the Immune System 7 Immune Cells and Their Products 19 Mounting an Immune Response 24 Immunity: Natural and Acquired 28 Disorders of the Immune System 34 Immunology and Transplants 36 Immunity and Cancer 39 The Immune System and the Nervous System 40 Frontiers in Immunology 45 Summary 47 Glossary Introduction he immune system is a network of Tcells, tissues*, and organs that work together to defend the body against attacks by “foreign” invaders. These are primarily microbes (germs)—tiny, infection-causing Bacteria: organisms such as bacteria, viruses, streptococci parasites, and fungi. Because the human body provides an ideal environment for many microbes, they try to break in. It is the immune system’s job to keep them out or, failing that, to seek out and destroy them. Virus: When the immune system hits the wrong herpes virus target or is crippled, however, it can unleash a torrent of diseases, including allergy, arthritis, or AIDS. The immune system is amazingly complex. It can recognize and remember millions of Parasite: different enemies, and it can produce schistosome secretions and cells to match up with and wipe out each one of them. -

A Novel BCMA/CD3 Bispecific T-Cell Engager for the Treatment
OPEN Leukemia (2017) 31, 1743–1751 www.nature.com/leu ORIGINAL ARTICLE A novel BCMA/CD3 bispecific T-cell engager for the treatment of multiple myeloma induces selective lysis in vitro and in vivo S Hipp1, Y-T Tai2,3, D Blanset4, P Deegen5, J Wahl5, O Thomas5, B Rattel5, PJ Adam1, KC Anderson2,3 and M Friedrich5 B-cell maturation antigen (BCMA) is a highly plasma cell-selective protein that is expressed on malignant plasma cells of multiple myeloma (MM) patients and therefore is an ideal target for T-cell redirecting therapies. We developed a bispecific T-cell engager (BiTE) targeting BCMA and CD3ε (BI 836909) and studied its therapeutic impacts on MM. BI 836909 induced selective lysis of BCMA- positive MM cells, activation of T cells, release of cytokines and T-cell proliferation; whereas BCMA-negative cells were not affected. Activity of BI 836909 was not influenced by the presence of bone marrow stromal cells, soluble BCMA or a proliferation-inducing ligand (APRIL). In ex vivo assays, BI 836909 induced potent autologous MM cell lysis in both, newly diagnosed and relapsed/ refractory patient samples. In mouse xenograft studies, BI 836909 induced tumor cell depletion in a subcutaneous NCI-H929 xenograft model and prolonged survival in an orthotopic L-363 xenograft model. In a cynomolgus monkey study, administration of BI 836909 led to depletion of BCMA-positive plasma cells in the bone marrow. Taken together, these results show that BI 836909 is a highly potent and efficacious approach to selectively deplete BCMA-positive MM cells and represents a novel immunotherapeutic for the treatment of MM. -
Regulatory Lymphocytes: the Dice That Resolve the Tumor Endgame Subhadip Pati, Anandi Chowdhury, Sumon Mukherjee, Aharna Guin, Shravanti Mukherjee and Gaurisankar Sa*
Pati et al. Applied Cancer Research (2020) 40:7 Applied Cancer Research https://doi.org/10.1186/s41241-020-00091-0 REVIEW Open Access Regulatory lymphocytes: the dice that resolve the tumor endgame Subhadip Pati, Anandi Chowdhury, Sumon Mukherjee, Aharna Guin, Shravanti Mukherjee and Gaurisankar Sa* Abstract A large number of cancer patients relapse after chemotherapeutic treatment. The immune system is capable of identifying and destroying cancer cells, so recent studies have highlighted the growing importance of using combinatorial chemotherapy and immunotherapy. However, many patients have innate or acquired resistance to immunotherapies. Long-term follow-up in a pooled meta-analysis exhibited long-term survival in approximately 20% of patients treated with immune checkpoint inhibitors or the adoptive transfer of chimeric T cells. It has been reported that high levels of immunoregulatory cells in cancer patients contribute to immunotherapy resistance via immunosuppression. Among the most important regulatory cell subtypes are the CD4+ T-regulatory cells (Tregs), identified by their expression of the well-characterized, lineage-specific transcription factor FOXP3. In addition to CD4+ Tregs, other regulatory cells present in the tumor microenvironment, namely CD8+ Tregs and IL10-producing B-regulatory cells (Bregs) that also modulate the immune response in solid and lymphoid tumors. These cells together have detrimental effects on tumor immune surveillance and anti-tumor immunity. Therefore, targeting these regulatory lymphocytes will be crucial in improving treatment outcomes for immunotherapy. Keywords: Breg, CTLA4, FOXP3, Immunotherapy, IL10, PDL1, Treg Background neo-antigens, which are not present in non-cancerous The suppression of anti-tumor immune responses and cells [5]. These neo-antigens offer a clinical advantage augmentation of tumor-promoting immune responses since the tumor cells expressing neo-antigens are then both contribute to tumor progression [1]. -

Immunology 101
Immunology 101 Justin Kline, M.D. Assistant Professor of Medicine Section of Hematology/Oncology Committee on Immunology University of Chicago Medicine Disclosures • I served as a consultant on Advisory Boards for Merck and Seattle Genetics. • I will discuss non-FDA-approved therapies for cancer 2 Outline • Innate and adaptive immune systems – brief intro • How immune responses against cancer are generated • Cancer antigens in the era of cancer exome sequencing • Dendritic cells • T cells • Cancer immune evasion • Cancer immunotherapies – brief intro 3 The immune system • Evolved to provide protection against invasive pathogens • Consists of a variety of cells and proteins whose purpose is to generate immune responses against micro-organisms • The immune system is “educated” to attack foreign invaders, but at the same time, leave healthy, self-tissues unharmed • The immune system can sometimes recognize and kill cancer cells • 2 main branches • Innate immune system – Initial responders • Adaptive immune system – Tailored attack 4 The immune system – a division of labor Innate immune system • Initial recognition of non-self (i.e. infection, cancer) • Comprised of cells (granulocytes, monocytes, dendritic cells and NK cells) and proteins (complement) • Recognizes non-self via receptors that “see” microbial structures (cell wall components, DNA, RNA) • Pattern recognition receptors (PRRs) • Necessary for priming adaptive immune responses 5 The immune system – a division of labor Adaptive immune system • Provides nearly unlimited diversity of receptors to protect the host from infection • B cells and T cells • Have unique receptors generated during development • B cells produce antibodies which help fight infection • T cells patrol for infected or cancerous cells • Recognize “foreign” or abnormal proteins on the cell surface • 100,000,000 unique T cells are present in all of us • Retains “memory” against infections and in some cases, cancer. -

Regulatory T Cell Research
Regulatory T cell research Unique kits for cell isolation Harmonized cell culture and expansion tools Convenient functional assay tools Germany/Austria/ Benelux France Nordics and Baltics South Korea Switzerland Miltenyi Biotec B.V. Miltenyi Biotec SAS Miltenyi Biotec Norden AB Miltenyi Biotec Korea Co., Ltd Reliable flow cytometry analysis Miltenyi Biotec GmbH Schipholweg 68 H 10 rue Mercoeur Scheelevägen 17 Arigi Bldg. 8F Friedrich-Ebert-Straße 68 2316 XE Leiden 75011 Paris, France 223 70 Lund 562 Nonhyeon-ro 51429 Bergisch Gladbach The Netherlands Phone +33 1 56 98 16 16 Sweden Gangnam-gu Germany [email protected] Fax +33 1 56 98 16 17 [email protected] Seoul 06136, South Korea Phone +49 2204 8306-0 Customer service [email protected] Customer service Sweden Phone +82 2 555 1988 Fax +49 2204 85197 The Netherlands Phone 0200-111 800 Fax +82 2 555 8890 [email protected] Phone 0800 4020120 Italy Fax 046-280 72 99 [email protected] Fax 0800 4020100 Miltenyi Biotec S.r.l. Customer service Denmark USA/Canada Customer service Belgium Via Persicetana, 2/D Phone 80 20 30 10 Spain Miltenyi Biotec Inc. Phone 0800 94016 40012 Calderara di Reno (BO) Fax +46 46 280 72 99 Miltenyi Biotec S.L. 2303 Lindbergh Street Fax 0800 99626 Italy Customer service C/Luis Buñuel 2 Auburn, CA 95602, USA Customer service Luxembourg Phone +39 051 6 460 411 Norway, Finland, Iceland, Ciudad de la Imagen Phone 800 FOR MACS Phone 800 24971 Fax +39 051 6 460 499 and Baltic countries 28223 Pozuelo de Alarcón (Madrid) Phone +1 530 888 8871 Fax 800 24984 [email protected] Phone +46 46 280 72 80 Spain Fax +1 877 591 1060 Fax +46 46 280 72 99 Phone +34 91 512 12 90 [email protected] China Japan Fax +34 91 512 12 91 Miltenyi Biotec Technology & Miltenyi Biotec K.K. -

CD8+CD122+Cd49dlow Regulatory T Cells Maintain T-Cell
+ + CD8 CD122 CD49dlow regulatory T cells maintain T-cell homeostasis by killing activated T cells via Fas/FasL-mediated cytotoxicity Kazuyuki Akanea,b, Seiji Kojimab, Tak W. Makc,1, Hiroshi Shikud,e, and Haruhiko Suzukia,1 aDepartment of Immunology, Nagoya University Graduate School of Medicine, Nagoya, Aichi 466-8550, Japan; bDepartment of Pediatrics, Nagoya University Graduate School of Medicine, Nagoya, Aichi 466-8550, Japan; cCampbell Family Institute for Breast Cancer Research, Princess Margaret Cancer Centre/University Health Network, Toronto, Ontario, Canada M5G 2M9; dDepartment of Cancer Vaccine, Mie University Graduate School of Medicine, Tsu, Mie 514-8507, Japan; and eDepartment of Immuno-Gene Therapy, Mie University Graduate School of Medicine, Tsu, Mie 514-8507, Japan Contributed by Tak W. Mak, January 15, 2016 (sent for review October 5, 2015; reviewed by Toshiaki Ohteki and Heiichiro Udono) The Fas/FasL (CD95/CD178) system is required for immune regula- regulatory action are available. Therefore, it is not clear precisely tion; however, it is unclear in which cells, when, and where Fas/FasL which subset of T cells express FasL or where Fas/FasL-dependent + molecules act in the immune system. We found that CD8+CD122+ CD8 Tregs, if such cells exist, are located and at which point cells, which are mostly composed of memory T cells in compari- they function. Thus, the ultimate pathophysiological role of the + − son with naïve cells in the CD8 CD122 population, were previ- Fas/FasL system is still unknown. ously shown to include cells with regulatory activity and could Regulation of the immune reaction is of pivotal importance be separated into CD49dlow cells and CD49dhigh cells. -

The Anatomy of T-Cell Activation and Tolerance Anna Mondino*T, Alexander Khoruts*, and Marc K
Proc. Natl. Acad. Sci. USA Vol. 93, pp. 2245-2252, March 1996 Review The anatomy of T-cell activation and tolerance Anna Mondino*t, Alexander Khoruts*, and Marc K. Jenkins Department of Microbiology and the Center for Immunology, University of Minnesota Medical School, 420 Delaware Street S.E, Minneapolis, MN 55455 ABSTRACT The mammalian im- In recent years, it has become clear that TCR is specific for a self peptide-class I mune system must specifically recognize a full understanding of immune tolerance MHC complex) T cell that will exit the and eliminate foreign invaders but refrain cannot be achieved with reductionist in thymus and seed the secondary lymphoid from damaging the host. This task is vitro approaches that separate the individ- tissues (3, 4). In contrast, cortical CD4+ accomplished in part by the production of ual lymphocyte from its in vivo environ- CD8+ thymocytes that express TCRs that a large number of T lymphocytes, each ment. The in vivo immune response is a have no avidity for self peptide-MHC bearing a different antigen receptor to well-organized process that involves mul- complexes do not survive and die by an match the enormous variety of antigens tiple interactions of lymphocytes with each apoptotic mechanism. Cortical epithelial present in the microbial world. However, other, with bone-marrow-derived antigen- cells are essential for the process of pos- because antigen receptor diversity is gen- presenting cells (APCs), as well as with itive selection because they display the self erated by a random mechanism, the im- nonlymphoid cells and their products. The peptide-MHC complexes that are recog- mune system must tolerate the function of anatomic features that are designed to op- nized by CD4+ CD8+ thymocytes and also T lymphocytes that by chance express a timize immune tolerance toward innocuous provide essential differentiation factors self-reactive antigen receptor. -

Vaccine Immunology Claire-Anne Siegrist
2 Vaccine Immunology Claire-Anne Siegrist To generate vaccine-mediated protection is a complex chal- non–antigen-specifc responses possibly leading to allergy, lenge. Currently available vaccines have largely been devel- autoimmunity, or even premature death—are being raised. oped empirically, with little or no understanding of how they Certain “off-targets effects” of vaccines have also been recog- activate the immune system. Their early protective effcacy is nized and call for studies to quantify their impact and identify primarily conferred by the induction of antigen-specifc anti- the mechanisms at play. The objective of this chapter is to bodies (Box 2.1). However, there is more to antibody- extract from the complex and rapidly evolving feld of immu- mediated protection than the peak of vaccine-induced nology the main concepts that are useful to better address antibody titers. The quality of such antibodies (e.g., their these important questions. avidity, specifcity, or neutralizing capacity) has been identi- fed as a determining factor in effcacy. Long-term protection HOW DO VACCINES MEDIATE PROTECTION? requires the persistence of vaccine antibodies above protective thresholds and/or the maintenance of immune memory cells Vaccines protect by inducing effector mechanisms (cells or capable of rapid and effective reactivation with subsequent molecules) capable of rapidly controlling replicating patho- microbial exposure. The determinants of immune memory gens or inactivating their toxic components. Vaccine-induced induction, as well as the relative contribution of persisting immune effectors (Table 2.1) are essentially antibodies— antibodies and of immune memory to protection against spe- produced by B lymphocytes—capable of binding specifcally cifc diseases, are essential parameters of long-term vaccine to a toxin or a pathogen.2 Other potential effectors are cyto- effcacy. -

Maxpar Human Helper T-Cell
PRD013-201318 Rev. 7 PRODUCT INFORMATION SHEET Maxpar Human Helper T Cell Phenotyping Panel Kit, 15 Marker—25 Tests Catalog: 201318 Storage: Package size: 25 tests • Antibodies, buffers, and water: 4 °C. Do not freeze. • Cell-ID Intercalator-Ir: –20 °C. Contents: Target Clone Metal Target Clone Metal • Maxpar® Cell Staining Buffer (500 mL) CD196/CCR6 G034E3 141Pr CD161 HP-3G10 159Tb • Maxpar Fix and Perm Buffer (25 mL) CD195/CCR5 NP-6G4 144Nd CD45RO UCHL1 165Ho • Maxpar Water (500 mL) CD8 RPA-T8 146Nd CD25 2A3 169Tm • Cell-IDTM Intercalator-Ir (125 µM; 25 µL) CD278/ICOS C398.4A 151Eu CD185/CXCR5 RF8B2 171Yb • Maxpar antibodies (see table for panel)* CD45RA HI100 153Eu CD4 SK3 174Yb CD3 UCHT1 154Sm CD279/PD-1 EH12.2H7 175Lu * The antibodies are provided in individual tubes, not a pre-mixed cocktail. CD183/CXCR3 G025H7 156Gd CD127 A019D5 176Yb CD194/CCR4 L291H4 158Gd Technical Information Description: The Maxpar Human Helper T Cell Phenotyping Panel Kit is for the identification and phenotyping of human CD4+ helper T cell subsets, including T helper 1 (TH1), TH2, TH17, TH22, T follicular helper (TFH), and T regulatory (TREG). Differentiation of CD4+ T cells into functionally distinct helper T subsets is essential for normal immunoregulation. These subsets are specified by extrinsic and intrinsic cues, and the resultant cell populations acquire stable phenotypes defined by the expression of signature cytokines, master regulator transcription factors, and characteristic cell surface phenotypes. Originally, CD4+ T cells were viewed as having only two major fates: 1) TH1 cells, which express T-bet and selectively produce interferon IFNγ and 2) TH2 cells, which express Gata3 and produce interleukin 4 (IL-4). -

T Cells by Regulatory T Cells + CD8 Differential Suppression of Tumor
Differential Suppression of Tumor-Specific CD8 + T Cells by Regulatory T Cells Edward James, Alex Yeh, Cathy King, Firouzeh Korangy, Ian Bailey, Denise S. Boulanger, Benoît J. Van den Eynde, This information is current as Nicholas Murray and Tim J. Elliott of October 2, 2021. J Immunol 2010; 185:5048-5055; Prepublished online 4 October 2010; doi: 10.4049/jimmunol.1000134 http://www.jimmunol.org/content/185/9/5048 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2010/10/04/jimmunol.100013 Material 4.DC1 References This article cites 42 articles, 19 of which you can access for free at: http://www.jimmunol.org/ http://www.jimmunol.org/content/185/9/5048.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on October 2, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Differential Suppression of Tumor-Specific CD8+ T Cells by Regulatory T Cells Edward James,* Alex Yeh,*,1 Cathy King,* Firouzeh Korangy,† Ian Bailey,* Denise S. -

Regulatory T-Cell Therapy in Crohn's Disease: Challenges and Advances
Recent advances in basic science Regulatory T- cell therapy in Crohn’s disease: Gut: first published as 10.1136/gutjnl-2019-319850 on 24 January 2020. Downloaded from challenges and advances Jennie N Clough ,1,2 Omer S Omer,1,3 Scott Tasker ,4 Graham M Lord,1,5 Peter M Irving 1,3 1School of Immunology and ABStract pathological process increasingly recognised as Microbial Sciences, King’s The prevalence of IBD is rising in the Western world. driving intestinal inflammation and autoimmunity College London, London, UK 2NIHR Biomedical Research Despite an increasing repertoire of therapeutic targets, a is the loss of immune homeostasis secondary to Centre at Guy’s and Saint significant proportion of patients suffer chronic morbidity. qualitative or quantitative defects in the regulatory Thomas’ NHS Foundation Trust Studies in mice and humans have highlighted the critical T- cell (Treg) pool. and King’s College, London, UK + 3 role of regulatory T cells in immune homeostasis, with Tregs are CD4 T cells that characteristically Department of defects in number and suppressive function of regulatory Gastroenterology, Guy’s and express the high- affinity IL-2 receptor α-chain Saint Thomas’ Hospitals NHS T cells seen in patients with Crohn’s disease. We review (CD25) and master transcription factor Forkhead Trust, London, UK the function of regulatory T cells and the pathways by box P-3 (Foxp3) which is essential for their suppres- 4 Division of Transplantation which they exert immune tolerance in the intestinal sive phenotype and stability.4–6