Originalresearch
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of 15-Lipoxygenase/15-Hydroxyeicosatetraenoic Acid in Hypoxia-Induced Pulmonary Hypertension
J Physiol Sci (2012) 62:163–172 DOI 10.1007/s12576-012-0196-9 REVIEW Role of 15-lipoxygenase/15-hydroxyeicosatetraenoic acid in hypoxia-induced pulmonary hypertension Daling Zhu • Yajuan Ran Received: 29 September 2011 / Accepted: 25 January 2012 / Published online: 14 February 2012 Ó The Physiological Society of Japan and Springer 2012 Abstract Pulmonary arterial hypertension (PAH) is a Introduction rare disease with a complex aetiology characterized by elevated pulmonary artery resistance, which leads to right Pulmonary hypertension (PH) is a severe and frequently heart ventricular afterload and ultimately progressing to fatal disease characterized by elevated mean pulmonary right ventricular failure and often death. In addition to arterial (PA) pressure greater than 25 mmHg at rest or other factors, metabolites of arachidonic acid cascade play greater than 30 mmHg with exercise [1], and which con- an important role in the pulmonary vasculature, and dis- tributes to the morbidity and mortality of adult and pedi- ruption of signaling pathways of arachidonic acid plays a atric patients with various lung and heart diseases. central role in the pathogenesis of PAH. 15-Lipoxygenase According to the Venice Classification of Pulmonary (15-LO) is upregulated in pulmonary artery endothelial Hypertension in 2003, PH is currently classified into five cells and smooth muscle cells of PAH patients, and its categories as listed in Table 1. Importantly, many of these metabolite 15-hydroxyeicosatetraenoic acid (15-HETE) in diseases or conditions are associated with persistent or particular seems to play a central role in the contractile intermittent hypoxia, either globally or regionally, within machinery, and in the initiation and propagation of cell confined areas of the lung [2]. -

Eicosanoids in Carcinogenesis
4open 2019, 2,9 © B.L.D.M. Brücher and I.S. Jamall, Published by EDP Sciences 2019 https://doi.org/10.1051/fopen/2018008 Special issue: Disruption of homeostasis-induced signaling and crosstalk in the carcinogenesis paradigm “Epistemology of the origin of cancer” Available online at: Guest Editor: Obul R. Bandapalli www.4open-sciences.org REVIEW ARTICLE Eicosanoids in carcinogenesis Björn L.D.M. Brücher1,2,3,*, Ijaz S. Jamall1,2,4 1 Theodor-Billroth-Academy®, Germany, USA 2 INCORE, International Consortium of Research Excellence of the Theodor-Billroth-Academy®, Germany, USA 3 Department of Surgery, Carl-Thiem-Klinikum, Cottbus, Germany 4 Risk-Based Decisions Inc., Sacramento, CA, USA Received 21 March 2018, Accepted 16 December 2018 Abstract- - Inflammation is the body’s reaction to pathogenic (biological or chemical) stimuli and covers a burgeoning list of compounds and pathways that act in concert to maintain the health of the organism. Eicosanoids and related fatty acid derivatives can be formed from arachidonic acid and other polyenoic fatty acids via the cyclooxygenase and lipoxygenase pathways generating a variety of pro- and anti-inflammatory mediators, such as prostaglandins, leukotrienes, lipoxins, resolvins and others. The cytochrome P450 pathway leads to the formation of hydroxy fatty acids, such as 20-hydroxyeicosatetraenoic acid, and epoxy eicosanoids. Free radical reactions induced by reactive oxygen and/or nitrogen free radical species lead to oxygenated lipids such as isoprostanes or isolevuglandins which also exhibit pro-inflammatory activities. Eicosanoids and their metabolites play fundamental endocrine, autocrine and paracrine roles in both physiological and pathological signaling in various diseases. These molecules induce various unsaturated fatty acid dependent signaling pathways that influence crosstalk, alter cell–cell interactions, and result in a wide spectrum of cellular dysfunctions including those of the tissue microenvironment. -

Fasted and Fed State Human Duodenal Fluids: Characterization, Drug Solubility, and Comparison to Simulated Fluids and with Human Bioavailability
European Journal of Pharmaceutics and Biopharmaceutics 163 (2021) 240–251 Contents lists available at ScienceDirect European Journal of Pharmaceutics and Biopharmaceutics journal homepage: www.elsevier.com/locate/ejpb Fasted and fed state human duodenal fluids: Characterization, drug solubility, and comparison to simulated fluids and with human bioavailability D. Dahlgren a, M. Venczel b,c, J.-P. Ridoux b,c, C. Skjold¨ a, A. Müllertz d, R. Holm e, P. Augustijns f, P.M. Hellstrom¨ g, H. Lennernas¨ a,* a Department of Pharmaceutical Biosciences, Biopharmaceutics, Uppsala University, Sweden b Global CMC Development Sanofi, Frankfurt, Germany c Global CMC Development Sanofi, Vitry, France d Physiological Pharmaceutics, University of Copenhagen, Copenhagen, Denmark e Drug Product Development, Janssen R&D, Johnson & Johnson, Beerse, Belgium f Drug Delivery and Disposition, KU Leuven, Leuven, Belgium g Department of Medical Sciences, Gastroenterology/Hepatology, Uppsala University, Sweden ARTICLE INFO ABSTRACT Keywords: Accurate in vivo predictions of intestinal absorption of low solubility drugs require knowing their solubility in Bioavailability physiologically relevant dissolution media. Aspirated human intestinal fluids (HIF) are the gold standard, fol Food effects lowed by simulated intestinal HIF in the fasted and fed state (FaSSIF/FeSSIF). However, current HIF charac Drug solubility terization data vary, and there is also some controversy regarding the accuracy of FaSSIF and FeSSIF for Human intestinal fluids predicting drug solubility in HIF. This study aimed at characterizing fasted and fed state duodenal HIF from 16 Drug absorption Drug dissolution human volunteers with respect to pH, buffer capacity, osmolarity, surface tension, as well as protein, phos Drug delivery pholipid, and bile salt content. -

Pharmacokinetic Interactions of Pioglitazone
Department of Clinical Pharmacology University of Helsinki Finland PHARMACOKINETIC INTERACTIONS OF PIOGLITAZONE Tiina Jaakkola ACADEMIC DISSERTATION To be presented, with the permission of the Medical Faculty of the University of Helsinki, for public examination in Auditorium 2 of Biomedicum, on August 24th, 2007, at 12 noon. Helsinki 2007 JJaakkola_Tiina_vaitos.inddaakkola_Tiina_vaitos.indd 1 117.7.20077.7.2007 221:11:231:11:23 Supervisors: Professor Pertti Neuvonen, MD Department of Clinical Pharmacology University of Helsinki Helsinki, Finland Docent Janne Backman, MD Department of Clinical Pharmacology University of Helsinki Helsinki, Finland Reviewers: Docent Kimmo Malminiemi, MD, MSc Department of Pharmacology, Clinical Pharmacology and Toxicology University of Tampere Tampere, Finland Professor emeritus Pertti Pentikäinen, MD Department of Medicine University of Helsinki Helsinki, Finland Opponent: Professor Kari Kivistö, MD Department of Pharmacology, Clinical Pharmacology and Toxicology University of Tampere Tampere, Finland ISBN 978-952-92-2224-7 (paperback) ISBN 978-952-10-4020-7 (PDF, http://ethesis.helsinki.fi ) Helsinki 2007 Yliopistopaino JJaakkola_Tiina_vaitos.inddaakkola_Tiina_vaitos.indd 2 117.7.20077.7.2007 221:11:551:11:55 JJaakkola_Tiina_vaitos.inddaakkola_Tiina_vaitos.indd 3 117.7.20077.7.2007 221:11:551:11:55 CONTENTS CONTENTS ABBREVIATIONS.......................................................................................................................................... 6 LIST OF ORIGINAL PUBLICATIONS....................................................................................................... -

Pharmacokinetic Interactions of Drugs with St John's Wort
http://www.paper.edu.cn Pharmacokinetic interactions of Journal of Psychopharmacology 18(2) (2004) 262–276 © 2004 British Association drugs with St John’s wort for Psychopharmacology ISSN 0269-8811 SAGE Publications Ltd, London, Thousand Oaks, CA and New Delhi 10.1177/0269881104042632 Shufeng Zhou Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore. Eli Chan Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore. Shen-Quan Pan Department of Biological Sciences, Faculty of Science, National University of Singapore, Singapore. Min Huang Institute of Clinical Pharmacology, School of Pharmaceutical Sciences, Sun Yat-Sen University, Guangzhou 510089, PR China. Edmund Jon Deoon Lee Department of Pharmacology, Faculty of Medicine, National University of Singapore, Singapore. Abstract There is a worldwide increasing use of herbs which are often cancer patients receiving irinotecan treatment. St John’s wort did not administered in combination with therapeutic drugs, raising the alter the pharmacokinetics of tolbutamide, but increased the incidence potential for herb–drug interactions. St John’s wort (Hypericum of hypoglycaemia. Several cases have been reported that St John’s wort perforatum) is one of the most commonly used herbal antidepressants. A decreased cyclosporine blood concentration leading to organ rejection. literature search was performed using Medline (via Pubmed), Biological St John’s wort caused breakthrough bleeding and unplanned pregnancies Abstracts, Cochrane Library, AMED, PsycINFO and Embase (all from their when used concomitantly with oral contraceptives. It also caused inception to September 2003) to identify known drug interaction with serotonin syndrome when coadministered with selective serotonin- St John’s wort. The available data indicate that St John’s wort is a reuptake inhibitors (e.g. -
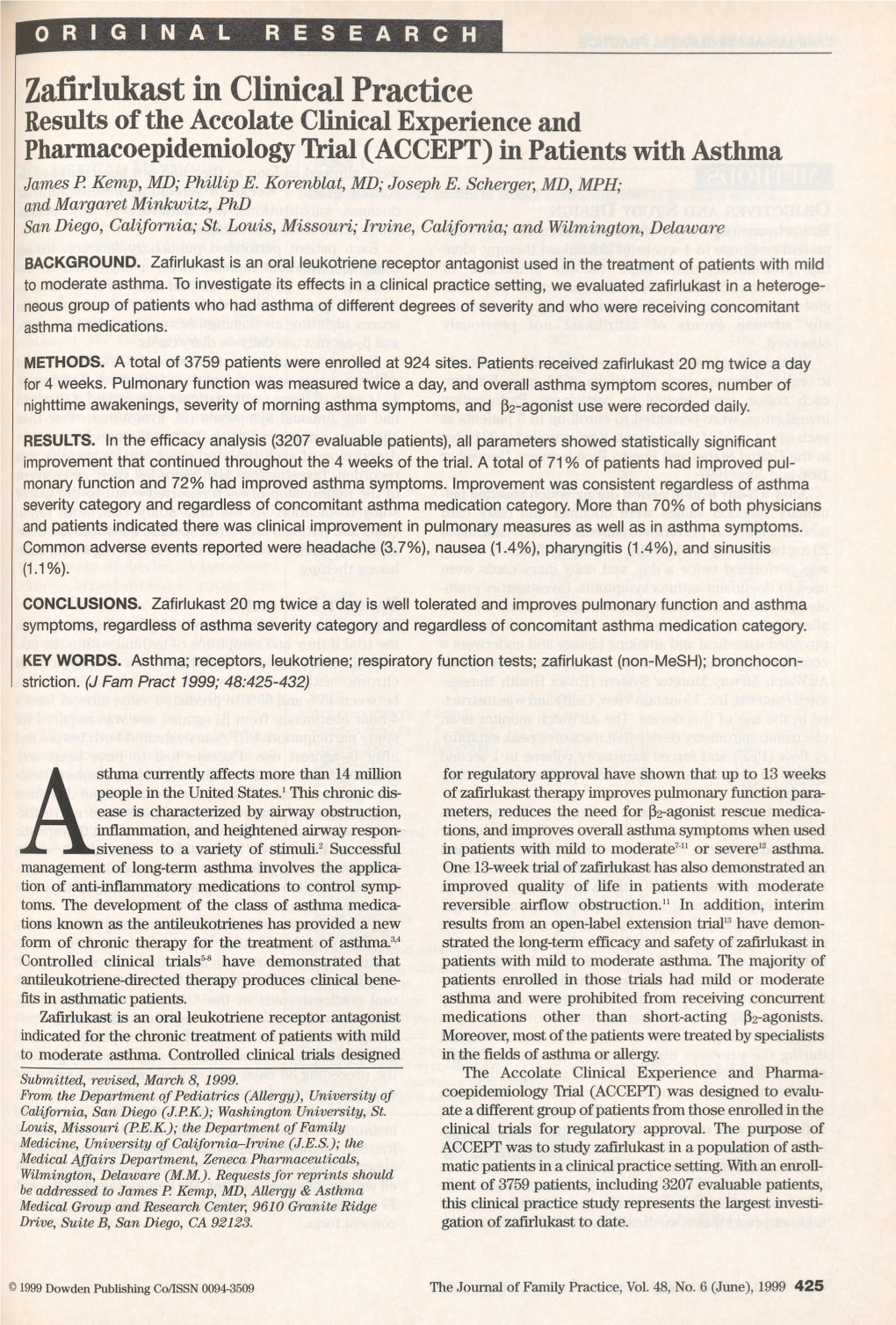
ACCOLATE® (Zafirlukast) TABLETS DESCRIPTION
ACCOLATE® (zafirlukast) TABLETS DESCRIPTION Zafirlukast is a synthetic, selective peptide leukotriene receptor antagonist (LTRA), with the chemical name 4-(5-cyclopentyloxy-carbonylamino-1-methyl-indol-3-ylmethyl)-3-methoxy-N-o tolylsulfonylbenzamide. The molecular weight of zafirlukast is 575.7 and the structural formula is: The empirical formula is: C31H33N3O6S Zafirlukast, a fine white to pale yellow amorphous powder, is practically insoluble in water. It is slightly soluble in methanol and freely soluble in tetrahydrofuran, dimethylsulfoxide, and acetone. ACCOLATE is supplied as 10 and 20 mg tablets for oral administration. Inactive Ingredients: Film-coated tablets containing croscarmellose sodium, lactose, magnesium stearate, microcrystalline cellulose, povidone, hypromellose, and titanium dioxide. CLINICAL PHARMACOLOGY Mechanism of Action: Zafirlukast is a selective and competitive receptor antagonist of leukotriene D4 and E4 (LTD4 and LTE4), components of slow-reacting substance of anaphylaxis (SRSA). Cysteinyl leukotriene production and receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle constriction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Patients with asthma were found in one study to be 25 100 times more sensitive to the bronchoconstricting activity of inhaled LTD4 than nonasthmatic subjects. In vitro studies demonstrated that zafirlukast antagonized the contractile activity of three leukotrienes (LTC4, LTD4 and LTE4) in conducting airway smooth muscle from laboratory animals and humans. Zafirlukast prevented intradermal LTD4-induced increases in cutaneous vascular permeability and Reference ID: 3407275 inhibited inhaled LTD4-induced influx of eosinophils into animal lungs. Inhalational challenge studies in sensitized sheep showed that zafirlukast suppressed the airway responses to antigen; this included both the early- and late-phase response and the nonspecific hyperresponsiveness. -

Serum Leukotriene Metabolism and Type I Hypersensitivity Reactions in Different Animal Species
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 1989 Serum leukotriene metabolism and Type I hypersensitivity reactions in different animal species Thulasi Sarojam Unnitan The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Unnitan, Thulasi Sarojam, "Serum leukotriene metabolism and Type I hypersensitivity reactions in different animal species" (1989). Graduate Student Theses, Dissertations, & Professional Papers. 3533. https://scholarworks.umt.edu/etd/3533 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. Maureen and Mike MANSFIELD TJBRARY Copying allowed as provided under provisions of the Fair Use Section of the U.S. COPYRIGHT LAW, 1976. Any copying for commercial purposes or financial gain may be undertaken only with the author's written consent. MontanaUniversity of SERUM LEUKOTRIENE METABOLISM AND TYPE I HYPERSENSITIVITY REACTIONS IN DIFFERENT ANIMAL SPECIES By Thulasi Sarojam Unnithan M.B.B.S., Trivandrum Medical College, India, 1981 Presented in partial fulfillment of the requirements for the degree of Master of Science University of Montana, 1989 8^'an, Graduate School ($hL& . & Date UMI Number: EP34626 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent on the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. -

Farmacopea De 2021 (Lista De Medicamentos Cubiertos)
Planes Medicare Advantage de ConnectiCare Plan ConnectiCare Choice 1 (HMO) Plan ConnectiCare Choice 2 (HMO) Plan ConnectiCare Choice 3 (HMO) Plan ConnectiCare Choice Part B Saver Plan ConnectiCare Flex 1 (HMO-POS) Plan ConnectiCare Flex 2 (HMO-POS) Plan ConnectiCare Flex 3 (HMO-POS) Plan ConnectiCare Passage 1 (HMO) Farmacopea de 2021 (Lista de medicamentos cubiertos) LEA LA SIGUIENTE INFORMACIÓN: ESTE DOCUMENTO CONTIENE INFORMACIÓN SOBRE LOS ME- DICAMENTOS QUE CUBRIMOS EN ESTE PLAN. 00021082, V17 Esta farmacopea se actualizó el 09/01/2021. Para obtener información más reciente o si tiene otras preguntas, comuníquese con Servicios para Miembros de ConnectiCare al 1-800-224-2273, los usuarios de TTY deben llamar al 711, de 8.00 am a 8.00 pm, hora del este, los siete días de la semana, o visite connecticare.com/medicare. Última actualización 09/01/2021 H3528_200567_C Nota para los miembros existentes: Esta farmacopea se ha cambiado desde el año pasado. Revise este documento para asegurarse de que aún se incluyan los medicamentos que usted toma. Cuando esta lista de medicamentos (farmacopea) haga referencia a “nosotros”, “nos” o “nuestro”, significa ConnectiCare. Cuando se refiere a “plan” o “nuestro plan”, significa los planes Medicare Advantage de ConnectiCare. Nuestros planes Medicare Advantage incluyen los planes ConnectiCare Choice 1 (HMO), ConnectiCare Choice 2 (HMO), ConnectiCare Choice 3 (HMO), ConnectiCare Choice Part B Saver, ConnectiCare Flex 1 (HMO-POS), ConnectiCare Flex2 (HMO-POS), ConnectiCare Flex 3 (HMO-POS) y ConnectiCare Passage 1 (HMO). Este documento incluye una lista de los medicamentos (farmacopea) para nuestro plan que se encuentra vigente desde el 09/01/2021 . -

Ioi70902.Pdf
ORIGINAL INVESTIGATION Montelukast, a Once-Daily Leukotriene Receptor Antagonist, in the Treatment of Chronic Asthma A Multicenter, Randomized, Double-blind Trial Theodore F. Reiss, MD; Paul Chervinsky, MD; Robert J. Dockhorn, MD; Sumiko Shingo, MS; Beth Seidenberg, MD; Thomas B. Edwards, MD; for the Montelukast Clinical Research Study Group Objectives: To determine the clinical effect of oral mon- Results: Montelukast improved airway obstruction telukast sodium, a leukotriene receptor antagonist, in asth- (forced expiratory volume in 1 second, morning and matic patients aged 15 years or more. evening peak expiratory flow rate) and patient-reported end points (daytime asthma symptoms, “as-needed” Design: Randomized, multicenter, double-blind, placebo- b-agonist use, nocturnal awakenings) (P,.001 com- controlled, parallel-group study. A 2-week, single- pared with placebo). Montelukast provided near- blind, placebo run-in period was followed by a 12- maximal effect in these end points within the first day week, double-blind treatment period (montelukast of treatment. Tolerance and rebound worsening of asthma sodium, 10 mg, or matching placebo, once daily at bed- did not occur. Montelukast improved outcome end points, time) and a 3-week, double-blind, washout period. including asthma exacerbations, asthma control days (P,.001 compared with placebo), and decreased periph- Setting/Patients: Fifty clinical centers randomly allo- eral blood eosinophil counts (P,.001 compared with pla- cated 681 patients with chronic, stable asthma to receive pla- cebo). The incidence of adverse events and discontinu- cebo or montelukast after demonstrating a forced expira- ations from therapy were similar in the montelukast and tory volume in 1 second 50% to 85% of the predicted value, placebo groups. -

Strict Regio-Specificity of Human Epithelial 15-Lipoxygenase-2
Strict Regio-specificity of Human Epithelial 15-Lipoxygenase-2 Delineates its Transcellular Synthesis Potential Abigail R. Green, Shannon Barbour, Thomas Horn, Jose Carlos, Jevgenij A. Raskatov, Theodore R. Holman* Department Chemistry and Biochemistry, University of California Santa Cruz, 1156 High Street, Santa Cruz CA 95064, USA *Corresponding author: Tel: 831-459-5884. Email: [email protected] FUNDING: This work was supported by the NIH NS081180 and GM56062. Abbreviations: LOX, lipoxygenase; h15-LOX-2, human epithelial 15-lipoxygenase-2; h15-LOX-1, human reticulocyte 15-lipoxygenase-1; sLO-1, soybean lipoxygenase-1; 5-LOX, leukocyte 5-lipoxygenase; 12-LOX, human platelet 12-lipoxygenase; GP, glutathione peroxidase; AA, arachidonic acid; HETE, hydoxy-eicosatetraenoic acid; HPETE, hydroperoxy-eicosatetraenoic acid; diHETEs, dihydroxy-eicosatetraenoic acids; 5-HETE, 5-hydroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid; 5-HPETE, 5-hydro peroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid; 12-HPETE, 12-hydroperoxy-5Z,8Z,10E, 14Z-eicosatetraenoic acid; 15-HPETE, 15-hydroperoxy-5Z,8Z,10Z,13E- eicosatetraenoic acid; 5,15-HETE, 5S,15S-dihydroxy-6E,8Z,10Z,13E-eicosatetraenoic acid; 5,15-diHPETE, 5,15-dihydroperoxy-6E,8Z,10Z,13E-eicosatetraenoic acid; 5,6- diHETE, 5S,6R-dihydroxy-7E,9E,11Z,14Z-eicosatetraenoic acid; LTA4, 5S-trans-5,6- oxido-7E,9E,11Z,14Z-eicosatetraenoic acid; LTB4, 5S,12R-dihydroxy-6Z,8E,10E,14Z- eicosatetraenoic acid; LipoxinA4 (LxA4), 5S,6R,15S-trihydroxy-7E,9E,11Z,13E- eicosatetraenoic acid; LipoxinB4 (LxB4), 5S,14R,15S-trihydroxy-6E,8Z,10E,12E- eicosatetraenoic acid. Abstract Lipoxins are an important class of lipid mediators that induce the resolution of inflammation, and arise from transcellular exchange of arachidonic acid (AA)- derived lipoxygenase products. -

Montelukast, a Leukotriene Receptor Antagonist, for the Treatment of Persistent Asthma in Children Aged 2 to 5 Years
Montelukast, a Leukotriene Receptor Antagonist, for the Treatment of Persistent Asthma in Children Aged 2 to 5 Years Barbara Knorr, MD*; Luis M. Franchi, MD‡; Hans Bisgaard, MD§; Jan Hendrik Vermeulen, MDʈ; Peter LeSouef, MD¶; Nancy Santanello, MD, MS*; Theresa M. Michele, MD*; Theodore F. Reiss, MD*; Ha H. Nguyen, PhD*; and Donna L. Bratton, MD# ABSTRACT. Background. The greatest prevalence of baseline period. Patients had a history of physician-di- asthma is in preschool children; however, the clinical agnosed asthma requiring use of -agonist and a pre- utility of asthma therapy for this age group is limited by defined level of daytime asthma symptoms. Caregivers a narrow therapeutic index, long-term tolerability, and answered questions twice daily on a validated, asthma- frequency and/or difficulty of administration. Inhaled specific diary card and, at specified times during the corticosteroids and inhaled cromolyn are the most com- study, completed a validated asthma-specific quality-of- monly prescribed controller therapies for young children life questionnaire. Physicians and caregivers completed a with persistent asthma, although very young patients global evaluation of asthma control at the end of the may have difficulty using inhalers, and dose delivery can study. be variable. Moreover, reduced compliance with inhaled Efficacy end points included: daytime and overnight therapy relative to orally administered therapy has been asthma symptoms, daily use of -agonist, days without reported. One potential advantage of montelukast is the asthma, frequency of asthma attacks, number of patients ease of administering a once-daily chewable tablet; ad- discontinued because of asthma, need for rescue medica- ditionally, no tachyphylaxis or change in the safety pro- tion, physician and caregiver global evaluations of file has been evidenced after up to 140 and 80 weeks of change, asthma-specific caregiver quality of life, and pe- montelukast therapy in adults and pediatric patients ripheral blood eosinophil counts. -
Medicare Part D: 2021 Value Plan Formulary
| Value Plan | Express Scripts Medicare (PDP) 2021 Formulary (List of Covered Drugs) PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN Formulary ID Number: 21095, Version 10 This formulary was updated on 9/1/2021. For more recent information or other questions, please contact Express Scripts Medicare® (PDP) Customer Service at 1.800.758.4574; New York State residents: 1.800.758.4570 or, for TTY users, 1.800.716.3231, 24 hours a day, 7 days a week, or visit express-scripts.com. Note to existing members: This formulary has changed since last year. Please review this document to make sure that it still contains the drugs you take. When this drug list (formulary) refers to “we,” “us,” or “our,” it means Medco Containment Life Insurance Company and Medco Containment Insurance Company of New York (for members located in New York State only). When it refers to “plan” or “our plan,” it means Express Scripts Medicare. This document includes a list of the drugs (formulary) for our plan, which is current as of September 1, 2021. For an updated formulary, please contact us. Our contact information, along with the date we last updated the formulary, appears on the front and back cover pages. You must generally use network pharmacies to use your prescription drug benefit. Benefits, formulary, pharmacy network and/or copayments/coinsurance may change on January 1, 2022, and from time to time during the year. What is the Express Scripts Medicare Formulary? A formulary is a list of covered drugs selected by Express Scripts Medicare in consultation with a team of healthcare providers, which represents the prescription therapies believed to be a necessary part of a quality treatment program.