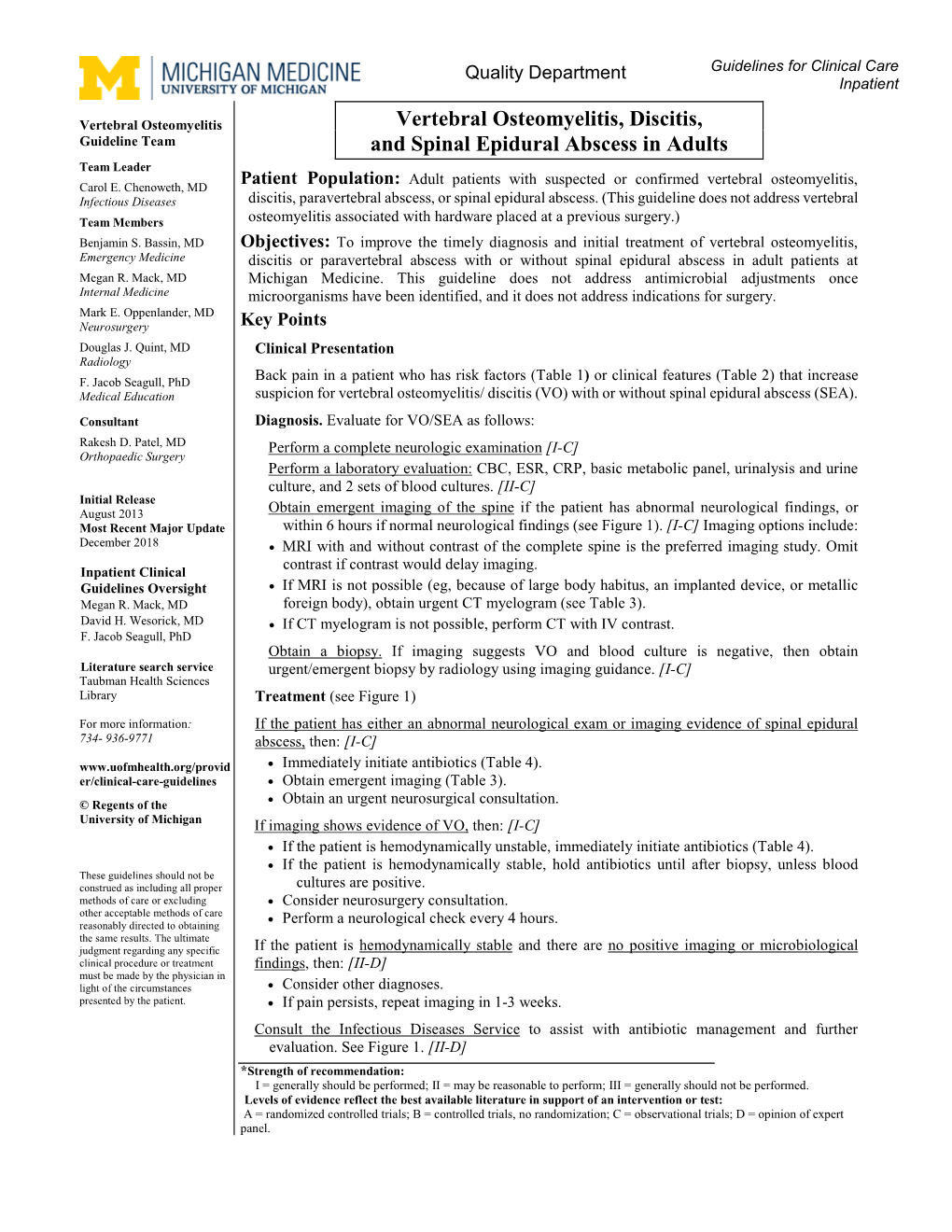
Vertebral Osteomyelitis, Discitis, and Spinal Epidural Abscess in Adults
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rehabilitation Outcomes Following Infections Causing Spinal Cord Myelopathy
Spinal Cord (2014) 52, 444–448 & 2014 International Spinal Cord Society All rights reserved 1362-4393/14 www.nature.com/sc ORIGINAL ARTICLE Rehabilitation outcomes following infections causing spinal cord myelopathy PW New1,2 and I Astrakhantseva1 Study design: Retrospective, open-cohort, consecutive case series. Objective: To describe the demographic characteristics, clinical features and outcomes in patients undergoing initial in-patient rehabilitation after an infectious cause of spinal cord myelopathy. Setting: Spinal Rehabilitation Unit, Melbourne, Victoria, Australia. Admissions between 1 January 1995 and 31 December 2010. Methods: The following data were recorded: aetiology of spinal cord infection, risk factors, rehabilitation length of stay (LOS), level of injury (paraplegia vs tetraplegia), complications related to spinal cord damage and discharge destination. The American Spinal Injury Association (ASIA) Impairment Scale (AIS) and functional independence measure (FIM) were assessed at admission and at discharge. Results: Fifty-one patients were admitted (men ¼ 32, 62.7%) with a median age of 65 years (interquartile range (IQR) 52–72, range 22–89). On admission, 37 (73%) had paraplegic level of injury and most patients (n ¼ 46, 90%) had an incomplete grade of spinal damage. Infections were most commonly bacterial (n ¼ 47, 92%); the other causes were viral (n ¼ 3, 6%) and tuberculosis (n ¼ 1, 2%). The median LOS was 106 days (IQR 65–135). The most common complications were pain (n ¼ 47, 92%), urinary tract infection (n ¼ 27, 53%), spasticity (n ¼ 25, 49%) and pressure ulcer during acute hospital admission (n ¼ 19, 37%). By the time of discharge from rehabilitation, patients typically showed a significant change in their AIS grade of spinal damage (Po0.001). -

Brucellar Spondylodiscitis with Rapidly Progressive Spinal Epidural Abscess Showing Cauda Equina Syndrome
Citation: Spinal Cord Series and Cases (2016) 2, 15030; doi:10.1038/scsandc.2015.30 © 2016 International Spinal Cord Society All rights reserved 2058-6124/16 www.nature.com/scsandc CASE REPORT Brucellar spondylodiscitis with rapidly progressive spinal epidural abscess showing cauda equina syndrome Tan Hu1,2,JiWu1,2, Chao Zheng1 and Di Wu1 Early diagnosis of Brucellosis is often difficult in the patient with only single non-specific symptom because of its rarity. We report a patient with Brucellar spondylodiscitis, in which the low back pain was the only symptom and the magnetic resonance imaging (MRI) showed not radiographic features about infection at initial stage. He was misdiagnosed as a lumbar disc herniation for inappropriate treatment in a long time. The delay in diagnosis and correct treatment led to rapid progression of the disease and severe complications. The patient was treated successfully with triple-antibiotic and surgical intervention in the end. Brucellar spondylodiscitis should always be suspended in the differential diagnosis specially when the patient comes from an endemic area or has consumed dairy products from animals in such an area and comprehensive examination should be done for the patent to rule out some important diseases like Brucellosis with sufficient reasons. Spinal Cord Series and Cases (2016) 2, 15030; doi:10.1038/scsandc.2015.30; published online 7 January 2016 Brucellosis is caused by small, non-motile, Gram-negative, aerobic post meridiem and intermittent left lower limb numbness for the and facultative intracellular coccobacilli of the genus Brucella recent weeks. One week before admission, the patient returned transmitted from infected animals to humans either by to the local clinic because his symptoms worsen. -
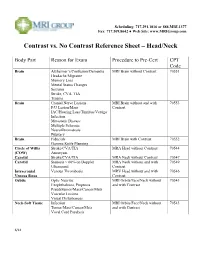
Contrast Vs. No Contrast Reference Sheet – Head/Neck
Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Head/Neck Body Part Reason for Exam Procedure to Pre-Cert CPT Code Brain Alzheimer’s/Confusion/Dementia MRI Brain without Contrast 70551 Headache/Migraine Memory Loss Mental Status Changes Seizures Stroke, CVA, TIA Trauma Brain Cranial Nerve Lesions MRI Brain without and with 70553 F/U Lesion/Mass Contrast IAC/Hearing Loss/Tinnitus/Vertigo Infection Metastatic Disease Multiple Sclerosis Neurofibromatosis Pituitary Brain Fiducials MRI Brain with Contrast 70552 Gamma Knife Planning Circle of Willis Stroke/CVA/TIA MRA Head without Contrast 70544 (COW) Aneurysm Carotid Stroke/CVA/TIA MRA Neck without Contrast 70547 Carotid Stenosis > 60% on Doppler MRA Neck without and with 70549 Ultrasound Contrast Intracranial Venous Thrombosis MRV Head without and with 70546 Venous Sinus Contrast Orbits Optic Neuritis MRI Orbits/Face/Neck without 70543 Exophthalmos, Proptosis and with Contrast Pseudotumor/Mass/Cancer/Mets Vascular Lesions Visual Disturbances Neck-Soft Tissue Infection MRI Orbits/Face/Neck without 70543 Tumor/Mass/Cancer/Mets and with Contrast Vocal Cord Paralysis 6/14 Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Spine Body Part Reason for Exam Procedure to Pre-Cert CPT Code Spine: Cervical Degenerative Disease MRI Cervical Spine without Contrast 72141 Disc Herniation Extremity Pain/Weakness Neck Pain Radiculopathy Trauma Spine: -

Paraplegia Caused by Infectious Agents; Etiology, Diagnosis and Management
Chapter 1 Paraplegia Caused by Infectious Agents; Etiology, Diagnosis and Management Farhad Abbasi and Soolmaz Korooni Fardkhani Additional information is available at the end of the chapter http://dx.doi.org/10.5772/56989 1. Introduction Paraplegia or paralysis of lower extremities is caused mainly by disorders of the spinal cord and the cauda equina. They are classified as traumatic and non traumatic. Traumatic paraple‐ gia occurs mostly as a result of traffic accidents and falls caused by lateral bending, dislocation, rotation, axial loading, and hyperflexion or hyperextension of the cord. Non-traumatic paraplegia has multiple causes such as cancer, infection, intervertebral disc disease, vertebral injury and spinal cord vascular disease [1, 2]. Although the incidence of spinal cord injury is low, the consequences of this disabling condition are extremely significant for the individual, family and community [3]. A spinal cord injury not only causes paralysis, but also has long- term impact on physical, psychosocial, sexual and mental health. The consequences of spinal cord injury require that health care professionals begin thinking about primary prevention. Efforts are often focused on care and cure, but evidence-based prevention should have a greater role. Primary prevention efforts can offer significant cost benefits, and efforts to change behavior and improve safety can and should be emphasized. Primary prevention can be applied to various etiologies of injury, including motor vehicle crashes, sports injuries, and prevention of sequelae of infectious diseases and prompt and correct diagnosis and treatment of infections involving spinal cord and vertebrae [4]. Infections are important causes of paraplegia. Several infections with different mechanisms can lead to paraplegia. -

Cervical Neck Pain Or Cervical Radiculopathy
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Cervical Neck Pain or Cervical Radiculopathy Variant 1: New or increasing nontraumatic cervical or neck pain. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography cervical spine Usually Appropriate ☢☢ MRI cervical spine without IV contrast May Be Appropriate (Disagreement) O CT cervical spine without IV contrast May Be Appropriate ☢☢☢ CT cervical spine with IV contrast Usually Not Appropriate ☢☢☢ MRI cervical spine without and with IV Usually Not Appropriate contrast O CT cervical spine without and with IV Usually Not Appropriate contrast ☢☢☢ CT myelography cervical spine Usually Not Appropriate ☢☢☢☢ CTA neck with IV contrast Usually Not Appropriate ☢☢☢ Discography cervical spine Usually Not Appropriate ☢☢ Facet injection/medial branch block cervical Usually Not Appropriate spine ☢☢ MRA neck with IV contrast Usually Not Appropriate O MRA neck without IV contrast Usually Not Appropriate O MRI cervical spine with IV contrast Usually Not Appropriate O Bone scan whole body with SPECT or Usually Not Appropriate SPECT/CT neck ☢☢☢ X-ray myelography cervical spine Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Cervical Neck Pain or Cervical Radiculopathy Variant 2: New or increasing nontraumatic cervical radiculopathy. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level MRI cervical spine without IV contrast Usually Appropriate O CT cervical spine without IV contrast -

Musculoskeletal Radiology.Pdf
MS 1 Acute osteomyelitis Acute osteomyelitis Plain radiographs reviewed Spine Other bones MRI Acute osteomyelitis Acute osteomyelitis diagnosed not diagnosed CT, MRI or Nuclear medicine Diagnosis Normal established scan Osteomyelitis Treatment excluded 144 MS 1 Acute osteomyelitis REMARKS 1 Plain radiograph 1.1 Regional radiographs should be the initial examination to determine whether there is any underlying pathological condition. 1.2 Typical findings of bone destruction and periosteal reaction may not appear until 10- 21 days after the onset of infection because 30-50% of bone density loss must occur before radiographs become abnormal. 1.3 Plain radiographs are unreliable to establish the diagnosis of osteomyelitis in patients with violated bone. 1.4 Plain radiographs of spine are not sensitive to detect vertebral osteomyelitis but findings of endplate destruction and progressive narrowing of adjacent disc space are highly suggestive of infection. 2 Nuclear medicine 2.1 Scans should be interpreted with contemporary radiographs. 2.2 Three-phase Technetium-99m methylene diphosphonate (Tc-99m-MDP) bone scan 2.2.1 Bone scan is more sensitive than plain radiography (up to 90% sensitivity). 2.2.2 Bone scan can be positive as early as 3 days after onset of disease (10-14 days earlier than plain radiograph). 2.3 Gallium scan 2.3.1 Gallium scan is helpful as conjunction with a bone scan. Combined gallium and bone scan studies has sensitivity of 81-90% and specificity of 69-100% 2.4 White blood cells (WBC) scan 2.4.1 This is sensitive and specific for bone infection and particularly useful in violated bone. -

An Unusual Cause of Back Pain in Osteoporosis: Lessons from a Spinal Lesion
Ann Rheum Dis 1999;58:327–331 327 MASTERCLASS Series editor: John Axford Ann Rheum Dis: first published as 10.1136/ard.58.6.327 on 1 June 1999. Downloaded from An unusual cause of back pain in osteoporosis: lessons from a spinal lesion S Venkatachalam, Elaine Dennison, Madeleine Sampson, Peter Hockey, MIDCawley, Cyrus Cooper Case report A 77 year old woman was admitted with a three month history of worsening back pain, malaise, and anorexia. On direct questioning, she reported that she had suVered from back pain for four years. The thoracolumbar radiograph four years earlier showed T6/7 vertebral collapse, mild scoliosis, and degenerative change of the lumbar spine (fig 1); but other investigations at that time including the eryth- rocyte sedimentation rate (ESR) and protein electophoresis were normal. Bone mineral density then was 0.914 g/cm2 (T score = −2.4) at the lumbar spine, 0.776 g/cm2 (T score = −1.8) at the right femoral neck and 0.738 g/cm2 (T score = −1.7) at the left femoral neck. She was given cyclical etidronate after this vertebral collapse as she had suVered a previous fragility fracture of the left wrist. On admission, she was afebrile, but general examination was remarkable for pallor, dental http://ard.bmj.com/ caries, and cellulitis of the left leg. A pansysto- lic murmur was heard at the cardiac apex on auscultation; there were no other signs of bac- terial endocarditis. She had kyphoscoliosis and there was diVuse tenderness of the thoraco- lumbar spine. Her neurological examination was unremarkable. on September 29, 2021 by guest. -

Acute Calcific Discitis with Intravertebral Disc Herniation in the Dorsolumbar Spine
Published online: 2021-08-02 MUSCULOSKELETAL Case report: Acute calcific discitis with intravertebral disc herniation in the dorsolumbar spine Puneet Mittal, Kavita Saggar, Parambir Sandhu, Kamini Gupta Department of Radiodiagnosis, Dayanand Medical College & Hospital, Ludhiana, Punjab, India Correspondence: Dr. Puneet Mittal, Department of Radiodiagnosis, Dayanand Medical College & Hospital, Tagore Nagar, Civil Lines, Ludhiana, Punjab - 141 001, India. E-mail: [email protected] Abstract Acute calcific discitis is a rare but well-known condition of unknown etiology. In symptomatic cases, the most common site is the cervical spine. We describe the CT scan and MRI findings in a symptomatic patient, with a lesion in the dorsolumbar spine. Key words: Acute; calcific; discitis; dorsolumbar; MR Introduction Acute calcifc discitis is a rare condition. When symptomatic, it can be mistaken for infection.[1] Most of the symptomatic cases present in the cervical spine.[1-3] We present the CT scan and MRI findings in a patient who had involvement of the dorsolumbar spine, with associated intravertebral disc herniation. Case Report A 10-year-old boy presented with a 2-week history of pain in the lower back following a yoga session in school. The pain had gradually worsened over the last 5 days. The patient was afebrile. The total white blood cell (WBC) count was normal. The erythrocyte sedimentation rate (ESR) was raised (52 mm/h). The Mantoux test was negative. A radiograph obtained elsewhere and repeated a day after the MRI [Figure 1], showed calcification of the D12-L1 intervertebral disc. MRI showed hypointense signal in the D12-L1 intervertebral disc on T1W [Figure 2A] and T2W [Figure 2B and C] images. -

Cervical Spondylodiscitis in an Infant with Torticollis
Cervical Spondylodiscitis in IMAGES IN CLINICAL an Infant with Torticollis RADIOLOGY BRECHT VAN BERKEL KRISTIN SUETENS LUC BREYSEM *Author affiliations can be found in the back matter of this article ABSTRACT CORRESPONDING AUTHOR: Brecht Van Berkel Teaching point: Narrowing of the intervertebral space and destruction of the adjacent UZ Leuven, BE vertebral end plates on conventional radiography or CT should raise suspicion for brecht.vanberkel@student. spondylodiscitis in symptomatic infants. kuleuven.be KEYWORDS: Spondylodiscitis; MRI; pediatric; torticollis; cervical; CT TO CITE THIS ARTICLE: Van Berkel B, Suetens K, Breysem L. Cervical Spondylodiscitis in an Infant with Torticollis. Journal of the Belgian Society of Radiology. 2021; 105(1): 35, 1–4. DOI: https://doi.org/10.5334/ jbsr.2454 Van Berkel et al. Journal of the Belgian Society of Radiology DOI: 10.5334/jbsr.2454 2 CASE REPORT disc space and loss of height of vertebral bodies C3 and C4 and irregular alignment of the end plates. On An eight-month-old infant presented at the emergency the sagittal T1-weighted Short-tau inversion-recovery department with a history of torticollis for six weeks. (STIR) images, the hyperintense signal in the vertebral Blood results showed no elevated inflammatory bodies of C3 and C4, as well as in the surrounding tissues parameters. Vertical lateral X-ray of the cervical spine (arrowheads) were compatible with a widespread area demonstrated a kyphotic angulation at the level of C3– of bone and soft tissue oedema (Figure 2). There were C4, narrowing of the intervertebral disc space, irregular no diffusion-restricted areas and no accompanying fluid end plates, and loss of height of the vertebral body of collections. -

Spinal Epidural Abscess
The new england journal of medicine review article CURRENT CONCEPTS Spinal Epidural Abscess Rabih O. Darouiche, M.D. From the Infectious Disease Section, the espite advances in medical knowledge, imaging techniques, and Michael E. DeBakey Veterans Affairs Medi- surgical interventions, spinal epidural abscess remains a challenging prob- cal Center, and the Center for Prostheses Infection, Baylor College of Medicine, Dlem that often eludes diagnosis and receives suboptimal treatment. The inci- Houston. Address reprint requests to Dr. dence of this disease — two decades ago diagnosed in approximately 1 of 20,000 Darouiche at the Center for Prostheses hospital admissions1 — has doubled in the past two decades, owing to an aging popu- Infection, Baylor College of Medicine, 1333 Moursund Ave., Suite A221, Houston, TX lation, increasing use of spinal instrumentation and vascular access, and the spread 77030, or at [email protected]. of injection-drug use.2-5 Still, spinal epidural abscess remains rare: the medical literature contains only 24 reported series of at least 20 cases each.1-24 This review N Engl J Med 2006;355:2012-20. Copyright © 2006 Massachusetts Medical Society. addresses the pathogenesis, clinical features, diagnosis, treatment, common diag- nostic and therapeutic pitfalls, and outcome of bacterial spinal epidural abscess. PATHOGENESIS Most patients with spinal epidural abscess have one or more predisposing condi- tions, such as an underlying disease (diabetes mellitus, alcoholism, or infection with human immunodeficiency virus), -

Disorders of the Thoracic Spine: Pathology and Treatment
Disorders of the thoracic spine: pathology and treatment CHAPTER CONTENTS • Extraspinal tumours involve the bony parts of the Disorders and their treatment e169 vertebrae. Benign tumours are usually located in the posterior parts (spinous and transverse processes), Tumours of the thoracic spine . e169 malignant tumours in the vertebral body. Extradural haematoma . e171 Spinal cord herniation . e173 Thoracic spinal canal stenosis . e173 Chest deformities . e173 Intraspinal tumours Fracture of a transverse process . e179 Spinal infections . e179 Thoracic neurofibroma Lateral recess stenosis . e180 Pathology Arthritis of the costovertebral and This benign tumour usually originates from the dorsal root and costotransverse joints . e180 arises from proliferating nerve fibres, fibroblasts and Schwann Arthritis of the thoracic facet joints . e181 cells. Sensory or motor fibres may be involved.1 Some confu- Paget’s disease . e181 sion exists about the terminology: various names, such as neu- rofibroma, neurinoma, neurilemmoma or schwannoma have been used. Some believe that all these terms cover the same type of tumour; others distinguish some slight histological dif- Disorders and their treatment ferences between them. Multiple tumours in nerve fibres and the subcutaneous tissues, often accompanied by patchy café Tumours of the thoracic spine au lait pigmentation, constitute the syndrome known as von Recklinghausen’s disease. Neuromas are the most common primary tumours of the Spinal neoplasms, both primary and secondary, are unusual spine accounting for approximately one-third of the cases. causes of thoracolumbar pain. However, because these lesions They are most often seen at the lower thoracic region and the are associated with high mortality, examiners must always be thoracolumbar junction.2 More than half of all these lesions are aware of the possibility of neoplastic diseases and must include intradural extramedullary (Fig 1), 25% are purely extradural, them in their differential diagnosis. -
2012 Meeting Program
Western Orthopaedic Association 76th Annual Meeting June 13–16, 2012 The Hilton Portland Portland, Oregon 2012 Meeting Program Chuck Freitag Executive Director, Data Trace Management Services, a Data Trace Company Cynthia Lichtefeld Director of Operations, Data Trace Management Services, a Data Trace Company WOA Central Office, Data Trace Management Services 110 West Road, Suite 227 Towson, MD 21204 Phone: 866-962-1388 Fax: 410-494-0515 Email: [email protected] Visit us on the World Wide Web @ www.woa-assn.org Please notify the WOA Central Office of any changes in your home or office address. This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the American Academy of Ortho- paedic Surgeons and the Western Orthopaedic Association. The American Academy of Orthopaedic Surgeons is accredited by the ACCME to provide continuing medical education for physicians. The American Academy of Orthopaedic Surgeons designates this live activity for a maximum of 28.75 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Cover Design by Lauren Murphy. Copyright © 2012 by Data Trace Publishing Company, Towson, MD. All rights reserved. Western Orthopaedic Association 76th Annual Meeting Portland, Oregon 2012 President’s Message Dear Colleagues, elcome to Portland for the 76th Annual Meeting of the Western Orthopaedic Association. Jeanne and I are honored to welcome you to The City of Roses. We hope Wyou enjoy the diverse and educational academic program in combination with unique social activities planned for you and your family.