Cervical Radiculopathy Clinical Guidelines for Medical Necessity Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
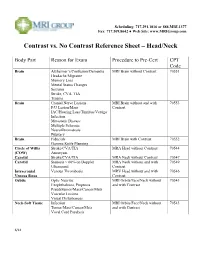
Contrast Vs. No Contrast Reference Sheet – Head/Neck
Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Head/Neck Body Part Reason for Exam Procedure to Pre-Cert CPT Code Brain Alzheimer’s/Confusion/Dementia MRI Brain without Contrast 70551 Headache/Migraine Memory Loss Mental Status Changes Seizures Stroke, CVA, TIA Trauma Brain Cranial Nerve Lesions MRI Brain without and with 70553 F/U Lesion/Mass Contrast IAC/Hearing Loss/Tinnitus/Vertigo Infection Metastatic Disease Multiple Sclerosis Neurofibromatosis Pituitary Brain Fiducials MRI Brain with Contrast 70552 Gamma Knife Planning Circle of Willis Stroke/CVA/TIA MRA Head without Contrast 70544 (COW) Aneurysm Carotid Stroke/CVA/TIA MRA Neck without Contrast 70547 Carotid Stenosis > 60% on Doppler MRA Neck without and with 70549 Ultrasound Contrast Intracranial Venous Thrombosis MRV Head without and with 70546 Venous Sinus Contrast Orbits Optic Neuritis MRI Orbits/Face/Neck without 70543 Exophthalmos, Proptosis and with Contrast Pseudotumor/Mass/Cancer/Mets Vascular Lesions Visual Disturbances Neck-Soft Tissue Infection MRI Orbits/Face/Neck without 70543 Tumor/Mass/Cancer/Mets and with Contrast Vocal Cord Paralysis 6/14 Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Spine Body Part Reason for Exam Procedure to Pre-Cert CPT Code Spine: Cervical Degenerative Disease MRI Cervical Spine without Contrast 72141 Disc Herniation Extremity Pain/Weakness Neck Pain Radiculopathy Trauma Spine: -

Cervical Spondylosis
Page 1 of 6 Cervical Spondylosis This leaflet is aimed at people who have been told they have cervical spondylosis as a cause of their neck symptoms. Cervical spondylosis is a 'wear and tear' of the vertebrae and discs in the neck. It is a normal part of ageing and does not cause symptoms in many people. However, it is sometimes a cause of neck pain. Symptoms tend to come and go. Treatments include keeping the neck moving, neck exercises and painkillers. In severe cases, the degeneration may cause irritation or pressure on the spinal nerve roots or spinal cord. This can cause arm or leg symptoms (detailed below). In these severe cases, surgery may be an option. Understanding the neck The back of the neck includes the cervical spine and the muscles and ligaments that surround and support it. The cervical spine is made up of seven bones called vertebrae. The first two are slightly different to the rest, as they attach the spine to the skull and allow the head to turn from side to side. The lower five cervical vertebrae are roughly cylindrical in shape - a bit like small tin cans - with bony projections. The sides of the vertebrae are linked by small facet joints. Between each of the vertebrae is a 'disc'. The discs are made of a tough fibrous outer layer and a softer gel-like inner part. The discs act like 'shock absorbers' and allow the spine to be flexible. Strong ligaments attach to adjacent vertebrae to give extra support and strength. Various muscles attached to the spine enable the spine to bend and move in various ways. -

Chapter 4: Massage and Sciatica: an In-Depth Study 2 CE Hours
Chapter 4: Massage and Sciatica: An In-Depth Study 2 CE Hours By: Kerry Davis, LMT, CIMT, CPT Learning objectives Define the characteristics of sciatica. Discuss how to construct a treatment plan. Recognize the causes of sciatica. Discuss how to assess the client’s posture and gait. Compare sciatica with other conditions of the low back. Describe the evaluation of the client’s pain patterns and symptoms. Distinguish the muscle imbalance patterns attributing to sciatica. Demonstrate practice of test assessments to rule out other Understand the pattern of referred pain resulting from sciatica. conditions of the low back. Illustrate application of massage techniques to treat the client. Overview Low back pain affects more than three million people in the United encounter multiple cases during the course of their practice due to the States each year (Werner, 2002). According to a 2010 survey, low back impact that low back pain has on society. This course will educate the pain was listed as the third most oppressive condition afflicting people. massage therapist about how to identify sciatica. It will also familiarize Low back pain does not discriminate between men and women and the therapist with the most common causes of sciatica, discuss usually presents as early as the age of thirty; in fact, the prevalence differences between sciatica from piriformis syndrome and sacroiliac increases in correlation with age (National Institute of Neurological joint dysfunctions, examine the proper evaluation of the condition, as Disorders and Stroke, 2015). It is likely that massage therapists will well as develop the treatment protocols for sciatica. UNDERSTANDING SCIATICA Sciatica, or lumbar radiculopathy, is characterized as an inflammation in the feet and toes. -

Cervical Neck Pain Or Cervical Radiculopathy
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Cervical Neck Pain or Cervical Radiculopathy Variant 1: New or increasing nontraumatic cervical or neck pain. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography cervical spine Usually Appropriate ☢☢ MRI cervical spine without IV contrast May Be Appropriate (Disagreement) O CT cervical spine without IV contrast May Be Appropriate ☢☢☢ CT cervical spine with IV contrast Usually Not Appropriate ☢☢☢ MRI cervical spine without and with IV Usually Not Appropriate contrast O CT cervical spine without and with IV Usually Not Appropriate contrast ☢☢☢ CT myelography cervical spine Usually Not Appropriate ☢☢☢☢ CTA neck with IV contrast Usually Not Appropriate ☢☢☢ Discography cervical spine Usually Not Appropriate ☢☢ Facet injection/medial branch block cervical Usually Not Appropriate spine ☢☢ MRA neck with IV contrast Usually Not Appropriate O MRA neck without IV contrast Usually Not Appropriate O MRI cervical spine with IV contrast Usually Not Appropriate O Bone scan whole body with SPECT or Usually Not Appropriate SPECT/CT neck ☢☢☢ X-ray myelography cervical spine Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Cervical Neck Pain or Cervical Radiculopathy Variant 2: New or increasing nontraumatic cervical radiculopathy. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level MRI cervical spine without IV contrast Usually Appropriate O CT cervical spine without IV contrast -
Adult Spinal Deformity and Its Relationship with Height Loss
Shimizu et al. BMC Musculoskeletal Disorders (2020) 21:422 https://doi.org/10.1186/s12891-020-03464-2 RESEARCH ARTICLE Open Access Adult spinal deformity and its relationship with height loss: a 34-year longitudinal cohort study Mutsuya Shimizu1* , Tetsuya Kobayashi1, Hisashi Chiba2, Issei Senoo1, Hiroshi Ito1, Keisuke Matsukura3 and Senri Saito3 Abstract Background: Age-related height loss is a normal physical change that occurs in all individuals over 50 years of age. Although many epidemiological studies on height loss have been conducted worldwide, none have been long- term longitudinal epidemiological studies spanning over 30 years. This study was designed to investigate changes in adult spinal deformity and examine the relationship between adult spinal deformity and height loss. Methods: Fifty-three local healthy subjects (32 men, 21 women) from Furano, Hokkaido, Japan, volunteered for this longitudinal cohort study. Their heights were measured in 1983 and again in 2017. Spino-pelvic parameters were compared between measurements obtained in 1983 and 2017. Individuals with height loss were then divided into two groups, those with degenerative spondylosis and those with degenerative lumbar scoliosis, and different characteristics were compared between the two groups. Results: The mean age of the subjects was 44.4 (31–55) years at baseline and 78.6 (65–89) years at the final follow- up. The mean height was 157.4 cm at baseline and 153.6 cm at the final follow-up, with a mean height loss of 3.8 cm over 34.2 years. All parameters except for thoracic kyphosis were significantly different between measurements taken in 1983 and 2017 (p < 0.05). -

Acute Calcific Discitis with Intravertebral Disc Herniation in the Dorsolumbar Spine
Published online: 2021-08-02 MUSCULOSKELETAL Case report: Acute calcific discitis with intravertebral disc herniation in the dorsolumbar spine Puneet Mittal, Kavita Saggar, Parambir Sandhu, Kamini Gupta Department of Radiodiagnosis, Dayanand Medical College & Hospital, Ludhiana, Punjab, India Correspondence: Dr. Puneet Mittal, Department of Radiodiagnosis, Dayanand Medical College & Hospital, Tagore Nagar, Civil Lines, Ludhiana, Punjab - 141 001, India. E-mail: [email protected] Abstract Acute calcific discitis is a rare but well-known condition of unknown etiology. In symptomatic cases, the most common site is the cervical spine. We describe the CT scan and MRI findings in a symptomatic patient, with a lesion in the dorsolumbar spine. Key words: Acute; calcific; discitis; dorsolumbar; MR Introduction Acute calcifc discitis is a rare condition. When symptomatic, it can be mistaken for infection.[1] Most of the symptomatic cases present in the cervical spine.[1-3] We present the CT scan and MRI findings in a patient who had involvement of the dorsolumbar spine, with associated intravertebral disc herniation. Case Report A 10-year-old boy presented with a 2-week history of pain in the lower back following a yoga session in school. The pain had gradually worsened over the last 5 days. The patient was afebrile. The total white blood cell (WBC) count was normal. The erythrocyte sedimentation rate (ESR) was raised (52 mm/h). The Mantoux test was negative. A radiograph obtained elsewhere and repeated a day after the MRI [Figure 1], showed calcification of the D12-L1 intervertebral disc. MRI showed hypointense signal in the D12-L1 intervertebral disc on T1W [Figure 2A] and T2W [Figure 2B and C] images. -

Cervical Spondylodiscitis in an Infant with Torticollis
Cervical Spondylodiscitis in IMAGES IN CLINICAL an Infant with Torticollis RADIOLOGY BRECHT VAN BERKEL KRISTIN SUETENS LUC BREYSEM *Author affiliations can be found in the back matter of this article ABSTRACT CORRESPONDING AUTHOR: Brecht Van Berkel Teaching point: Narrowing of the intervertebral space and destruction of the adjacent UZ Leuven, BE vertebral end plates on conventional radiography or CT should raise suspicion for brecht.vanberkel@student. spondylodiscitis in symptomatic infants. kuleuven.be KEYWORDS: Spondylodiscitis; MRI; pediatric; torticollis; cervical; CT TO CITE THIS ARTICLE: Van Berkel B, Suetens K, Breysem L. Cervical Spondylodiscitis in an Infant with Torticollis. Journal of the Belgian Society of Radiology. 2021; 105(1): 35, 1–4. DOI: https://doi.org/10.5334/ jbsr.2454 Van Berkel et al. Journal of the Belgian Society of Radiology DOI: 10.5334/jbsr.2454 2 CASE REPORT disc space and loss of height of vertebral bodies C3 and C4 and irregular alignment of the end plates. On An eight-month-old infant presented at the emergency the sagittal T1-weighted Short-tau inversion-recovery department with a history of torticollis for six weeks. (STIR) images, the hyperintense signal in the vertebral Blood results showed no elevated inflammatory bodies of C3 and C4, as well as in the surrounding tissues parameters. Vertical lateral X-ray of the cervical spine (arrowheads) were compatible with a widespread area demonstrated a kyphotic angulation at the level of C3– of bone and soft tissue oedema (Figure 2). There were C4, narrowing of the intervertebral disc space, irregular no diffusion-restricted areas and no accompanying fluid end plates, and loss of height of the vertebral body of collections. -

Differential Diagnoses for Disc Herniation
Revista Chilena de Radiología. Vol. 23 Nº 2, año 2017; 66-76. Differential diagnoses for disc herniation Marcelo Gálvez M.1, Jorge Cordovez M.1, Cecilia Okuma P.1, Carlos Montoya M.2, Takeshi Asahi K.2 1. Imaging Department, Clínica Las Condes. Santiago, Chile 2. Medical Biomodeling Laboratory, Clínica Las Condes. Santiago, Chile. Abstract Disc herniation is a frequent pathology in the radiologist’s daily practice. There are different pathologies that can imitate a herniated disc from the clinical, and especially the imaging point of view, that we should consider whenever we report a herniated disc. These lesions may originate from the vertebral body (os- teophytes and metastases), the intervertebral disc (discal cyst), the intervertebral foramina (neurinomas), the interapophyseal joints (synovial cyst) and from the epidural space (hematoma and epidural abscess). Keywords: Herniated disc, Spondylosis, osteophyte, bone metastasis, discal cyst, neurinoma, synovial cyst, epidural hematoma, epidural abscess. Introduction enhancement, with a “fried egg” appearance. We should Disc herniation is one of the most frequent diag- make the differential diagnosis of the herniated disc noses in the radiological practice of spine pathology. with other lesions that, although less frequent, can However, we must consider in the differential diagnosis lead to a misdiagnosis. These lesions can originate other pathologies that can imitate disc hernias, es- in neighboring structures such as the vertebral body, pecially in some sequences or planes when reading intervertebral disc, intervertebral foramen, interapophy- an MRI. Herniated discs, are frequently in contact siary joint or epidural space. We will consider that the with the intervertebral disc, and are located in the lesions that can originate from the vertebral body are extradural intrathecal space. -

Lumbar Degenerative Disease Part 1
International Journal of Molecular Sciences Article Lumbar Degenerative Disease Part 1: Anatomy and Pathophysiology of Intervertebral Discogenic Pain and Radiofrequency Ablation of Basivertebral and Sinuvertebral Nerve Treatment for Chronic Discogenic Back Pain: A Prospective Case Series and Review of Literature 1, , 1,2, 1 Hyeun Sung Kim y * , Pang Hung Wu y and Il-Tae Jang 1 Nanoori Gangnam Hospital, Seoul, Spine Surgery, Seoul 06048, Korea; [email protected] (P.H.W.); [email protected] (I.-T.J.) 2 National University Health Systems, Juronghealth Campus, Orthopaedic Surgery, Singapore 609606, Singapore * Correspondence: [email protected]; Tel.: +82-2-6003-9767; Fax.: +82-2-3445-9755 These authors contributed equally to this work. y Received: 31 January 2020; Accepted: 20 February 2020; Published: 21 February 2020 Abstract: Degenerative disc disease is a leading cause of chronic back pain in the aging population in the world. Sinuvertebral nerve and basivertebral nerve are postulated to be associated with the pain pathway as a result of neurotization. Our goal is to perform a prospective study using radiofrequency ablation on sinuvertebral nerve and basivertebral nerve; evaluating its short and long term effect on pain score, disability score and patients’ outcome. A review in literature is done on the pathoanatomy, pathophysiology and pain generation pathway in degenerative disc disease and chronic back pain. 30 patients with 38 levels of intervertebral disc presented with discogenic back pain with bulging degenerative intervertebral disc or spinal stenosis underwent Uniportal Full Endoscopic Radiofrequency Ablation application through either Transforaminal or Interlaminar Endoscopic Approaches. Their preoperative characteristics are recorded and prospective data was collected for Visualized Analogue Scale, Oswestry Disability Index and MacNab Criteria for pain were evaluated. -

Lumbar Spinal Stenosis Clinical Guidelines for Medical Necessity Review
Lumbar Spinal Stenosis Clinical Guidelines for Medical Necessity Review Version: 4.0 Effective Date: November 13, 2020 Lumbar Spinal Stenosis (v4.0) © 2020 Cohere Health, Inc. All Rights Reserved. Important Notices Notices & Disclaimers: GUIDELINES SOLELY FOR COHERE’S USE IN PERFORMING MEDICAL NECESSITY REVIEWS AND ARE NOT INTENDED TO INFORM OR ALTER CLINICAL DECISION MAKING OF END USERS. Cohere Health, Inc. (“Cohere”) has published these clinical guidelines to determine medical necessity of services (the “Guidelines”) for informational purposes only, and solely for use by Cohere’s authorized “End Users”. These Guidelines (and any attachments or linked third party content) are not intended to be a substitute for medical advice, diagnosis, or treatment directed by an appropriately licensed healthcare professional. These Guidelines are not in any way intended to support clinical decision making of any kind; their sole purpose and intended use is to summarize certain criteria Cohere may use when reviewing the medical necessity of any service requests submitted to Cohere by End Users. Always seek the advice of a qualified healthcare professional regarding any medical questions, treatment decisions, or other clinical guidance. The Guidelines, including any attachments or linked content, are subject to change at any time without notice. ©2020 Cohere Health, Inc. All Rights Reserved. Other Notices: CPT copyright 2019 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. Guideline Information: Specialty Area: Diseases of the musculoskeletal system and connective tissue (M00-M99) CarePath Group: Spine CarePath Name: Lumbar Spinal Stenosis (M48) Physician author: Mandy Armitage, MD (Sports Medicine) Peer reviewed by: Adrian Thomas, MD (Orthopedic Spine Surgeon) Literature review current through: June 22, 2020 Document last updated: November 13, 2020 Type: [X] Adult (18+ yo) | [_] Pediatric (0-17yo) Page 2 of 57 Lumbar Spinal Stenosis (v4.0) © 2020 Cohere Health, Inc. -

A Comparison of the Techniques of Direct Pars Interarticularis Repairs for Spondylolysis and Low-Grade Spondylolisthesis: a Meta-Analysis
NEUROSURGICAL FOCUS Neurosurg Focus 44 (1):E10, 2018 A comparison of the techniques of direct pars interarticularis repairs for spondylolysis and low-grade spondylolisthesis: a meta-analysis Nasser Mohammed, MD, MCh, Devi Prasad Patra, MD, MCh, Vinayak Narayan, MD, MCh, Amey R. Savardekar, MCh, Rimal Hanif Dossani, MD, Papireddy Bollam, MD, MSChe, Shyamal Bir, MD, PhD, and Anil Nanda, MD, MPH Department of Neurosurgery, LSU-HSC, Shreveport, Louisiana OBJECTIVE Spondylosis with or without spondylolisthesis that does not respond to conservative management has an excellent outcome with direct pars interarticularis repair. Direct repair preserves the segmental spinal motion. A number of operative techniques for direct repair are practiced; however, the procedure of choice is not clearly defined. The pres- ent study aims to clarify the advantages and disadvantages of the different operative techniques and their outcomes. METHODS A meta-analysis was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The following databases were searched: PubMed, Cochrane Library, Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature). Studies of patients with spondylolysis with or without low-grade spondylolisthesis who underwent direct repair were included. The patients were divided into 4 groups based on the operative technique used: the Buck repair group, Scott repair group, Morscher repair group, and pedicle screw–based repair group. The pooled data were analyzed using the DerSimonian and Laird random-effects model. Tests for bias and heterogeneity were performed. The I2 statistic was calculated, and the results were analyzed. Statistical analysis was performed using StatsDirect version 2. -

Cervical Spondylosis
PATIENT EDUCATION Cervical Spondylosis Cervical Spondylosis Pain in the neck is common and may be a natural consequence of aging in people over 50. Like the rest of the body, bones in the neck (cervical spine) progressively degenerate as we grow older. Over time, arthritis of the neck (cervical spondylosis) may result from bony spurs and problems with ligaments and disks. The spinal canal may narrow (stenosis) and compress the spinal cord and nerves to the arms. Injuries can also cause spinal cord compression. The pain that results may range from mild discomfort to severe, crippling dysfunction. Symptoms ● Cervical spondylosis can lead to chronic pain and stiffness in the neck that may also radiate to the upper extremities (radiculopathy). ● Neck pain and stiffness may be worse with upright activity. ● You may have numbness and weakness in the arms, hands and fingers, and trouble walking due to weakness in the legs. ● You may feel or hear grinding or popping in the neck when you move. ● Muscle spasms or headaches may originate in the neck. ● The condition can make you feel irritable and fatigued, disturb your sleep and impair your ability to work. See your doctor soon for diagnosis and treatment. Doctor's exam Give the doctor your complete medical history. This can help him or her rule out other conditions that cause symptoms similar to cervical spondylosis. The doctor will examine you physically and may take Xrays or use other diagnostic imaging tests to see inside the body. Medical history. Tell the doctor if you have any illnesses or chronic conditions.