Pathogenesis, Presentation, and Treatment of Lumbar Spinal Stenosis Associated with Coronal Or Sagittal Spinal Deformities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Audit of Bone Mineral Density and Associated Factors in Patients With
Review Article Clinician’s corner Images in Medicine Experimental Research Case Report Miscellaneous Letter to Editor DOI: 10.7860/JCDR/2019/39690.12544 Original Article Postgraduate Education An Audit of Bone Mineral Density and Case Series Associated Factors in Patients with Orthopaedics Section Lumbar Spinal Stenosis Short Communication ARASH RAHBAR1, RAHMATOLLAH JOKAR2, SEYED MOKHTAR ESMAEILNEJAD-GANJI3 ABSTRACT Results: Overall, 146 patients with lumbar stenosis were Introduction: Osteoporosis is a major global health problem enrolled. Based on bone densitometry of spine and femur, and is commonly observed with lumbar stenosis in older 35 (24%) and 36 (24.7%) of the patients had osteoporosis. people. It is stated that osteoporosis may cause progressive According to femoral densitometry, age (OR=1.311, 95% CI: spinal deformities and stenosis in elderly patients. 1.167-1.473), being a female (OR=3.391, 95% CI: 1.391-8.420) and being a homemaker (OR=3.675, 95% CI: 1.476-9.146) Aim: To audit prevalence of low bone mineral density and were found as risk factors for osteoporosis. Based on spinal associated factors in patients with lumbar spinal stenosis. densitometry, age (OR=1.283, 95% CI: 1.154-1.427) and being Materials and Methods: Patients with symptomatic lumbar a female (OR=2.786, 95% CI: 1.106-7.019) were associated with spinal stenosis were recruited in this cross-sectional study, osteoporosis. Significant correlations were observed between who had been referred to Shahid Beheshti hospital in Babol, bone mineral density and red blood cell counts (r=+0.168, Northern Iran, between 2016 and 2017. -

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -

Nonoperative Treatment of Lumbar Spinal Stenosis with Neurogenic Claudication a Systematic Review
SPINE Volume 37, Number 10, pp E609–E616 ©2012, Lippincott Williams & Wilkins LITERATURE REVIEW Nonoperative Treatment of Lumbar Spinal Stenosis With Neurogenic Claudication A Systematic Review Carlo Ammendolia , DC, PhD, *†‡ Kent Stuber, DC, MSc , § Linda K. de Bruin , MSc , ‡ Andrea D. Furlan, MD, PhD , ||‡¶ Carol A. Kennedy, BScPT, MSc , ‡#** Yoga Raja Rampersaud, MD , †† Ivan A. Steenstra , PhD , ‡ and Victoria Pennick, RN, BScN, MHSc ‡‡ or methylcobalamin, improve walking distance. There is very low- Study Design. Systematic review. quality evidence from a single trial that epidural steroid injections Objective. To systematically review the evidence for the improve pain, function, and quality of life up to 2 weeks compared effectiveness of nonoperative treatment of lumbar spinal stenosis with home exercise or inpatient physical therapy. There is low- with neurogenic claudication. quality evidence from a single trial that exercise is of short-term Summary of Background Data. Neurogenic claudication benefi t for leg pain and function compared with no treatment. There can signifi cantly impact functional ability, quality of life, and is low- and very low-quality evidence from 6 trials that multimodal independence in the elderly. nonoperative treatment is less effective than indirect or direct Methods. We searched CENTRAL, MEDLINE, EMBASE, CINAHL, surgical decompression with or without fusion. and ICL databases up to January 2011 for randomized controlled Conclusion. Moderate- and high-GRADE evidence for nonopera- trials published in English, in which at least 1 arm provided tive treatment is lacking and thus prohibiting recommendations to data on nonoperative treatments. Risk of bias in each study was guide clinical practice. Given the expected exponential rise in the independently assessed by 2 reviewers using 12 criteria. -
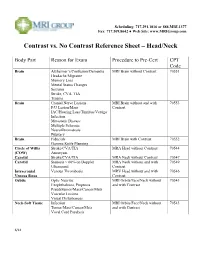
Contrast Vs. No Contrast Reference Sheet – Head/Neck
Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Head/Neck Body Part Reason for Exam Procedure to Pre-Cert CPT Code Brain Alzheimer’s/Confusion/Dementia MRI Brain without Contrast 70551 Headache/Migraine Memory Loss Mental Status Changes Seizures Stroke, CVA, TIA Trauma Brain Cranial Nerve Lesions MRI Brain without and with 70553 F/U Lesion/Mass Contrast IAC/Hearing Loss/Tinnitus/Vertigo Infection Metastatic Disease Multiple Sclerosis Neurofibromatosis Pituitary Brain Fiducials MRI Brain with Contrast 70552 Gamma Knife Planning Circle of Willis Stroke/CVA/TIA MRA Head without Contrast 70544 (COW) Aneurysm Carotid Stroke/CVA/TIA MRA Neck without Contrast 70547 Carotid Stenosis > 60% on Doppler MRA Neck without and with 70549 Ultrasound Contrast Intracranial Venous Thrombosis MRV Head without and with 70546 Venous Sinus Contrast Orbits Optic Neuritis MRI Orbits/Face/Neck without 70543 Exophthalmos, Proptosis and with Contrast Pseudotumor/Mass/Cancer/Mets Vascular Lesions Visual Disturbances Neck-Soft Tissue Infection MRI Orbits/Face/Neck without 70543 Tumor/Mass/Cancer/Mets and with Contrast Vocal Cord Paralysis 6/14 Scheduling: 717.291.1016 or 888.MRI.1377 Fax: 717.509.8642 ● Web Site: www.MRIGroup.com Contrast vs. No Contrast Reference Sheet – Spine Body Part Reason for Exam Procedure to Pre-Cert CPT Code Spine: Cervical Degenerative Disease MRI Cervical Spine without Contrast 72141 Disc Herniation Extremity Pain/Weakness Neck Pain Radiculopathy Trauma Spine: -

Double Spinal Cord Injury in a Patient with Ankylosing Spondylitis
Spinal Cord (1999) 37, 305 ± 307 ã 1999 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/99 $12.00 http://www.stockton-press.co.uk/sc Case Report Double spinal cord injury in a patient with ankylosing spondylitis MN Akman*,1 M KaratasÎ1, SÎ KilincË 1 and M AgÏ ildere1 1Department of Physical Medicine and Rehabilitation and Radiology, BahcË elievler, Ankara, Turkey Ankylosing spondylitis patients are more prone to spinal fractures and these fractures commonly result in mobile nonunion. We report a patient with a 30-year history of ankylosing spondylitis who sustained double spinal cord injuries following minor trauma. The ®rst injury occurred at the lumbar level due to pseudoarthrosis of an old fracture, and the second at the thoracic level following cardiopulmonary arrest and an episode of hypotension. The possible mechanisms of the injuries are discussed and maintaining normal blood pressure in these patients is emphasized. Keywords: spinal cord injury; ankylosing spondylitis; spinal cord infarction; spinal fractures Introduction Ankylosing spondylitis (AS) has a prevalance of 1 per diagnostic workup. His arterial blood pressure stayed 1000 in the general population and primarily involves below normal and his central venous pressure remained 1 the vertebral column. Spinal rigidity due to long- below 5 cmH2O for about 12 h. ECG, chest X-Ray standing AS renders the patient susceptible to vertebral and cranial computed tomography (CT) were normal. trauma, so that even minor trauma may cause When the patient awoke and was in a stable condition, fractures.2±9 There are only a few reports in the he could not feel or move his legs. -

Self-Help for Spinal Stenosis Information for Patients
Self-help for Spinal Stenosis Information for patients What is spinal stenosis? Spinal stenosis is a common condition affecting the lower back. It affects people over the age of 60 years. Spinal stenosis can result in symptoms including back pain, buttock pain and leg pain. Other symptoms include pins and needles, numbness and sometimes weakness in the legs or feet. If you have spinal stenosis you will likely experience a combination of these symptoms. What causes spinal stenosis? The spinal cord runs through a tunnel made from the bones in your back called vertebrae. This is because the bones are strong and act to protect the spinal cord. The nerves then branch out from the spinal cord and pass through smaller tunnels at the side of your spine. Sometimes the aging process leads to narrowing in parts of the lower back. This usually occurs gradually over time. The nerves and spinal cord may become tightened or squeezed as a result of this narrowing. Stenosis is the medical term for narrowing. Narrowing in the spine is very common but not everyone who has it will develop symptoms. Spinal stenosis can also occur at different levels in the spine. It is possible to get similar symptoms in your legs and feet that are not caused by spinal stenosis. Will spinal stenosis get better? It is not possible to reverse any age-related changes in the back; however it is possible to manage and improve your symptoms. Many people will experience “flare-ups” so it is important that you are confident in ways to manage your symptoms. -

New ASAS Criteria for the Diagnosis of Spondyloarthritis: Diagnosing Sacroiliitis by Magnetic Resonance Imaging 9
Document downloaded from http://www.elsevier.es, day 10/02/2016. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. Radiología. 2014;56(1):7---15 www.elsevier.es/rx UPDATE IN RADIOLOGY New ASAS criteria for the diagnosis of spondyloarthritis: ଝ Diagnosing sacroiliitis by magnetic resonance imaging ∗ M.E. Banegas Illescas , C. López Menéndez, M.L. Rozas Rodríguez, R.M. Fernández Quintero Servicio de Radiodiagnóstico, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain Received 17 January 2013; accepted 10 May 2013 Available online 11 March 2014 KEYWORDS Abstract Radiographic sacroiliitis has been included in the diagnostic criteria for spondy- Sacroiliitis; loarthropathies since the Rome criteria were defined in 1961. However, in the last ten years, Diagnosis; magnetic resonance imaging (MRI) has proven more sensitive in the evaluation of the sacroiliac Magnetic resonance joints in patients with suspected spondyloarthritis and symptoms of sacroiliitis; MRI has proven imaging; its usefulness not only for diagnosis of this disease, but also for the follow-up of the disease and Axial spondy- response to treatment in these patients. In 2009, The Assessment of SpondyloArthritis inter- loarthropathies national Society (ASAS) developed a new set of criteria for classifying and diagnosing patients with spondyloarthritis; one important development with respect to previous classifications is the inclusion of MRI positive for sacroiliitis as a major diagnostic criterion. This article focuses on the radiologic part of the new classification. We describe and illustrate the different alterations that can be seen on MRI in patients with sacroiliitis, pointing out the limitations of the technique and diagnostic pitfalls. -

Lumbar Spinal Stenosis a Patient's Guide to Lumbar Spinal Stenosis
Lumbar Spinal Stenosis A Patient's Guide to Lumbar Spinal Stenosis See a Washington Post story about a woman whose worsening pain stumped specialist after specialist for five years until she saw UM spine surgeon Steven Ludwig, who diagnosed the cause as spinal stenosis and performed successful surgery. Introduction Spinal stenosis is term commonly used to describe a narrowing of the spinal canal. This problem is much more common in people over the age of 60. However, it can occur in younger people who have abnormally small spinal canals as a type of birth defect. The problem usually causes back pain and leg pain that comes and goes with activities such as walking. The purpose of this information is to help you understand: • The anatomy of the spine relating to spinal stenosis • The signs and symptoms of lumbar spinal stenosis • How the condition is diagnosed • The treatments available for the condition Anatomy In order to understand your symptoms and treatment choices, you should start with some understanding of the general anatomy of your lumbar spine (lower back). This includes becoming familiar with the various parts that make up the spine and how these parts work together. Please review the document entitled: • Anatomy and Function of the Spine Causes Although there is some space between the spinal cord and the edges of the spinal canal, this space can be reduced by many conditions. Bone and tough ligaments surround the spinal canal. This tube cannot expand if the spinal cord or nerves require more space. If anything begins to narrow the spinal canal, the risk of irritation and injury of the spinal cord or nerves increases. -

Cervical Neck Pain Or Cervical Radiculopathy
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Cervical Neck Pain or Cervical Radiculopathy Variant 1: New or increasing nontraumatic cervical or neck pain. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level Radiography cervical spine Usually Appropriate ☢☢ MRI cervical spine without IV contrast May Be Appropriate (Disagreement) O CT cervical spine without IV contrast May Be Appropriate ☢☢☢ CT cervical spine with IV contrast Usually Not Appropriate ☢☢☢ MRI cervical spine without and with IV Usually Not Appropriate contrast O CT cervical spine without and with IV Usually Not Appropriate contrast ☢☢☢ CT myelography cervical spine Usually Not Appropriate ☢☢☢☢ CTA neck with IV contrast Usually Not Appropriate ☢☢☢ Discography cervical spine Usually Not Appropriate ☢☢ Facet injection/medial branch block cervical Usually Not Appropriate spine ☢☢ MRA neck with IV contrast Usually Not Appropriate O MRA neck without IV contrast Usually Not Appropriate O MRI cervical spine with IV contrast Usually Not Appropriate O Bone scan whole body with SPECT or Usually Not Appropriate SPECT/CT neck ☢☢☢ X-ray myelography cervical spine Usually Not Appropriate ☢☢☢ ACR Appropriateness Criteria® 1 Cervical Neck Pain or Cervical Radiculopathy Variant 2: New or increasing nontraumatic cervical radiculopathy. No “red flags.” Initial imaging. Procedure Appropriateness Category Relative Radiation Level MRI cervical spine without IV contrast Usually Appropriate O CT cervical spine without IV contrast -
Managing Spinal Conditions in Older Persons
JAMES ZUCHERMAN, MD JUDY SILVERMAN, MD Considering the patienfs overall medical status is crucial Managing spinal conditions in older persons ABSTRACT: Older patients who present with spinal complaints do not need to accept pain and diminished functional capacity as conse quences ofaging. Spinal stenosis results from the natural progression ofdegenerative changes in the spine. Thoracolumbar compression fractures usually are caused by trauma but also are common in pa tients who have osteoporosis. Mobility testing can help identif]^ un derlying pathology and deinse an exercise program. It is important to screenfor other causes ofpain, such as hip pathology. Radiography, MRI, and CTare useful imaging studies. The presence ofcauda equina syndrome requires urgent imaging and, usually, surgery. In This is the seventh in a special se some cases, a short course ofphysical therapy can reverse symptoms. ries ofarticles on the evaluation Lumbar or thoracic osteoporoticfracture treatmentfocuses on and management ofback pain. symptom management. (J Musculoskel Med. 2005;22:214-222) The percentage of the US popula the most common severe condi healthful living habits. Judicious ' tion older than 65 years has been tions in older persons. Consider use of exercise, proper body me increasing during the past centu ing a patient's overall medical sta chanics, medications, and surgery , ry and is peaking as baby boomers tus is crucial in management of can result in improvement in func- ; reach older age, Many older per these problems, because comor- tion and quality of Hfe. In this ar- | sons have aches, pains, and dimin bidities can affect treatment op tide, we describe the diagnosis ished functional capacity but do tions and outcomes. -

Long-Term Follow-Up Review of Patients Who Underwent Laminectomy for Lumbar Stenosis: a Prospective Study
Long-term follow-up review of patients who underwent laminectomy for lumbar stenosis: a prospective study Manucher J. Javid, M.D., and Eldad J. Hadar, M.D. Department of Neurological Surgery, University of Wisconsin Hospital and Clinics, Madison, Wisconsin Object. Decompressive laminectomy for stenosis is the most common operation performed on the lumbar spine in older patients. This prospective study was designed to evaluate long-term results in patients with symptomatic lumbar stenosis. Methods. Between January 1984 and January 1995, 170 patients underwent surgery for lumbar stenosis (86 patients), lumbar stenosis and herniated disc (61 patients), or lateral recess stenosis (23 patients). The male/female ratio for each group was 43:43, 39:22, and 14:9, respectively. The average age for all groups was 61.4 years. For patients with lumbar stenosis, the success rate was 88.1% at 6 weeks and 86.7% at 6 months. For patients with lumbar stenosis and herniated disc, the success rate was 80% at 6 weeks and 77.6% at 6 months, with no statistically significant difference between the two groups. For patients with lateral recess stenosis, the success rate was 58.7% at 6 weeks and 63.6% at 6 months; however, the sample was not large enough to be statistically significant. One year after surgery a questionnaire was sent to all patients; 163 (95.9%) responded. The success rate in patients with stenosis had declined to 69.6%, which was significant (p = 0.012); the rate for patients with stenosis and herniated disc was 77.2%; and that for lateral recess stenosis was 65.2%. -

Sacroiliitis Mimics: a Case Report and Review of the Literature Maria J
Antonelli and Magrey BMC Musculoskeletal Disorders (2017) 18:170 DOI 10.1186/s12891-017-1525-1 CASE REPORT Open Access Sacroiliitis mimics: a case report and review of the literature Maria J. Antonelli* and Marina Magrey Abstract Background: Radiographic sacroiliitis is the hallmark of ankylosing spondylitis (AS), and detection of acute sacroiliitis is pivotal for early diagnosis of AS. Although radiographic sacroiliitis is a distinguishing feature of AS, sacroiliitis can be seen in a variety of other disease entities. Case presentation: We present an interesting case of sacroiliitis in a patient with Paget disease; the patient presented with inflammatory back pain which was treated with bisphosphonate. This case demonstrates comorbidity with Paget disease and possible ankylosing spondylitis. We also present a review of the literature for other cases of Paget involvement of the sacroiliac joint. Conclusions: In addition, we review radiographic changes to the sacroiliac joint in classical ankylosing spondylitis as well as other common diseases. We compare and contrast features of other diseases that mimic sacroiliitis on a pelvic radiograph including Paget disease, osteitis condensans ilii, diffuse idiopathic skeletal hyperostosis, infections and sarcoid sacroiliitis. There are some features in the pelvic radiographic findings which help distinguish among mimics, however, one must also rely heavily on extra-pelvic radiographic lesions. In addition to the clinical presentation, various nuances may incline a clinician to the correct diagnosis; rheumatologists should be familiar with the imaging differences among these diseases and classic spondylitis findings. Keywords: Case report, Ankylosing spondylitis, Clinical diagnostics & imaging, Rheumatic disease Background We conducted a search in PubMed including combi- The presence of sacroiliitis on an anterior-posterior (AP) nations of the following search terms: sacroiliitis, sacro- pelvis or dedicated sacroiliac film is a defining feature of iliac, and Paget disease.