BREVITAL® (Methohexital Sodium) for Injection, USP
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Muscular Hyperactivity After General Anaesthesia
MUSCULAR HYPERACTIVITY AFTER GENERAL ANAESTHESIA MAGDIG. SOLIMA~,M.B., n.crl.,* and Dr_ara~lm M. M. CmLmS, wx.B., c~.~.* MvsctrzA~ HYPEr~,CrlWTY during recovery from general anaesthesia variously termed "spasticity, .... shivering," and "shakes," has been described by several authors and has been particularly related to halothane. 1~ Several mechanisms have been suggested in explanation including heat loss, t respiratory alkalosis, a early recovery of spinal reflex activity) at~d sympathetic overactivity.7 The re- ported incidence varies from 5 per cent to 70 per centa.s and this suggests that perhaps different phenomena are being described. Having noticed that some patients seemed to show true shivering whilst others showed intense muscular spasticity during emergence from general anaesthesia, this study was designed to try to elucidate whether there were, indeed, two dis- tinct phenomena, what was their incidence, and whether they were specifically i~lated to halothane anaesthesia. Spasticity was defined as sustained muscular hypertonieity most easily ob- served in jaw, neck and pectoral muscles, flexors of the upper limbs, and ex- tensors and adductors of the lower limbs. Shivering, on the other hand, was a rhythmic contraction of muscle groups with irregular intermittent periods of relaxation. METHODS The recovery of 215 unselected patients who had been anaesthetised for a wide variety of surgical procedures, both elective and emergent, was studied. Pre- medication was given one hour pre-operatively in the usual dosage, using ani- leridine and promethazine in the large majority. Induction was with thiolmntone. The largest group (I25) received halothane as the main agent, 50 received methuxyflurane, 20 cyelopropane, and 29 nitrous oxide, meperidine relaxant. -
ANESTHESIA a Comprehensive Review
ANESTHESIA A Comprehensive Review FIFTH EDITION Brian A. Hall, MD Assistant Professor of Anesthesiology College of Medicine, Mayo Clinic Rochester, Minnesota Robert C. Chantigian, MD Associate Professor of Anesthesiology College of Medicine, Mayo Clinic Rochester, Minnesota 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 ANESTHESIA: A COMPREHENSIVE REVIEW, FIFTH EDITION ISBN: 978-0-323-28662-6 Copyright © 2015, 2010, 2003, 1997, 1992 by Mayo Foundation for Medical Education and Research, Published by Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions poli- cies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). Notices Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods they should be mindful of their own safety and the safety of others, including parties for whom they have a profes- sional responsibility. -
Anticoagulation, Hemostasis, and Transfusions
FRONT OF BOOK ↑ [+] Cover [+] Authors - Foreword - Preface TABLE OF CONTENTS ↑ [+] 1 - General and Perioperative Care of the Surgical Patient [+] 2 - Common Postoperative Problems [+] 3 - Nutrition for the Surgical Patient [+] 4 - Fluid, Electrolytes, and Acid-Base Disorders [+] 5 - Anticoagulation, Hemostasis, and Transfusions [+] 6 - Anesthesia [+] 7 - Critical Care [+] 8 - Burns [+] 9 - Wound Care [+] 10 - Head, Neck, and Spinal Trauma [+] 11 - Chest Trauma [+] 12 - Abdominal Trauma [+] 13 - Extremity Trauma [+] 14 - Common Surgical Procedures [+] 15 - Acute Abdomen [+] 16 - Esophagus [+] 17 - Stomach [+] 18 - The Surgical Management of Obesity [+] 19 - Small Intestine [+] 20 - Surgical Diseases of the Liver [+] 21 - Surgical Diseases of the Biliary Tree [+] 22 - Surgical Diseases of the Pancreas [+] 23 - Spleen [+] 24 - Colon and Rectum [+] 25 - Anorectal Disease [+] 26 - Cerebrovascular Disease [+] 27 - Thoracoabdominal Vascular Disease [+] 28 - Peripheral Arterial Disease [+] 29 - Venous and Lymphatic Disease [+] 30 - Hemodialysis Access [+] 31 - Transplantation [+] 32 - Pediatric Surgery [+] 33 - Cardiac Surgery [+] 34 - Lung and Mediastinal Diseases [+] 35 - Breast [+] 36 - Skin and Soft-Tissue Tumors [+] 37 - Fundamentals of Laparoscopic, Robotic and Endoscopic Surgery [+] 38 - Hernias [+] 39 - Diseases of the Adrenal and Pituitary Gland and Hereditary Endocrine Syndromes [+] 40 - Thyroid and Parathyroid Glands [+] 41 - Otolaryngology for the General Surgeon [+] 42 - Plastic and Hand Surgery [+] 43 - Urology for the General Surgeon [+] 44 - Obstetrics and Gynecology for the General Surgeon [+] 45 - Biostatistics for the General Surgeon [+] 46 - Patient Safety and Quality Improvement in Surgery BACK OF BOOK ↑ [+] Answer Key [+] Index > Table of Contents > Authors Editors Mary E. Klingensmith MD1 1Department of Surgery Washington University School of Medicine St. Louis, Missouri Chandu Vemuri MD1 1Department of Surgery Washington University School of Medicine St. Louis, Missouri Oluwadamilola M. -
ECT – Anesthesia
Managing specific problems within anesthesia Alexander Sartorius Head of ECT Research and Supervison Head, Research Group Translational Imaging Department of Psychiatry and Psychotherapy Central Institute of Mental Health (CIMH) Medical Faculty Mannheim University of Heidelberg ECT – anesthesia: 1. Ketofol – two stones to catch one bird ? 2. Oxygen – the good gas ! 3. What’s that on the printout / monitor ? Part 1: Ketofol Adapted from: Folkerts HW. Electroconvulsive therapy. Indications, procedure and treatment results Nervenarzt. 2011 Jan;82(1):93-102 Swartz CM Electroconvulsive and neuromodulation therapies. 2009 Cambridge Univ, Cambridge New York Melbourne ECT – anesthesia: - thiopental 3-5 mg/kg - methohexital 50-120 mg - propofol 1-2 mg/kg German guidelines for tx of status epilepticus 1 => lorazepam up to 10mg i.v. 2 => phenytoin up to 30 mg/kg KG i.v. 3 => phenobarbital 20 mg/kg KG i.v. 4 => thiopental 4-7 mg/kg KG i.v. vs. propofol 1-2 mg/kg KG i.v. vs. midazolam or valproate Dosing of ECT anesthetics - experience of the anesthesiologist - experience from previous ECT sessions - time needed for full recovery - patient remembers muscle relaxation - systematic / non-systematic movements of the “cuffed” limb - objective criteria for “dosing” and “timing” do not exist … Br J Psychiatry. 1995 Jan;166(1):118-9. Anaesthetic technique in the practice of ECT. Collins IP, Scott IF. Bispectral Index Monitoring (BIS) - has been developed to prevent intraoperative awareness - uses combined EEG/EMG to derive a measure for “cortical integrity” inter alia by analyzing coherences between different frequency bands - More precisely: bispectrum is a 3rd order Fourier transformation that includes amplitude, phase AND coherence information. -

Effect of Intraoperative Infusion of Sufentanil Versus Remifentanil on Postoperative Shivering in Korea: a Prospective, Double-Blinded, Randomized Control Study
Turkish Journal of Medical Sciences Turk J Med Sci (2018) 48: 737-743 http://journals.tubitak.gov.tr/medical/ © TÜBİTAK Research Article doi:10.3906/sag-1709-161 Effect of intraoperative infusion of sufentanil versus remifentanil on postoperative shivering in Korea: a prospective, double-blinded, randomized control study 1,2 1,2 1 1,2 Ki Tae JUNG , Keum Young SO , In Gook JEE , Sang Hun KIM * 1 Department of Anesthesiology and Pain Medicine, Chosun University Hospital, Gwangju, Republic of Korea 2 Department of Anesthesiology and Pain Medicine, Chosun University, School of Medicine, Gwangju, Republic of Korea Received: 29.09.2017 Accepted/Published Online: 03.04.2018 Final Version: 16.08.2018 Background/aim: The number of published papers that compare the incidence of sufentanil- and remifentanil-related postoperative shivering is insufficient. We investigated the incidence of postoperative shivering after total intravenous anesthesia with either sufentanil or remifentanil in patients who underwent elective surgery. Materials and methods: Eighty-three patients, with a physical status classified as American Society of Anesthesiologists I or II, were randomly allocated to either the remifentanil–propofol (RP group, n = 40) or sufentanil–propofol (SP group, n = 43) group. The primary endpoint was the incidence of postoperative shivering 1 h after entering the recovery room. The secondary endpoints were intraoperative core temperatures of the esophagus and tympanic membrane at 30 min after the induction of anesthesia and at the end of surgery. Results: The overall postoperative shivering incidence was not significantly different between the RP (15%) and SP (11.6%) groups (P = 0.651). The intraoperative temperatures and their changes (the temperature 30 min after induction minus that after surgery) as measured at the distal esophagus and tympanic membrane were not significantly different between the RP and SP groups. -

Alexander Sartorius
EKT Narkose Alexander Sartorius Prof. apl. Dr. med. Dipl. Phys. Alexander Sartorius Facharzt für Psychiatrie und Psychotherapie, Geriatrie Oberarzt der Klinik für Psychiatrie und Psychotherapie Leiter der Arbeitsgruppe Translationales Imaging Wissenschaftliche Leitung und Supervision der EKT Medizinische Fakultät Mannheim / Universität Heidelberg Zentralinstitut für Seelische Gesundheit, J5, 68159 Mannheim Münsingen, 5.10.2019 3 pages on anesthesia – together! ECT – anesthesia: 1. Typical anesthetic drugs (p, e, m ,t) a. Ketofol – two stones to catch one bird ? 2. Some typical problems / solutions … a. ASTI b. Oxygen c. PAS / PIA d. Cardiac * ** *** * Hikma Pharmaceuticals stopped the production of methohexital 2019 ** Good Manufacturing Practice (GMP) problems at Lampugnani Pharmaceutici SPA *** In Germany: more or less obsolete for critically ill patients and for non-single induction use Adapted from: Folkerts HW. Electroconvulsive therapy. Indications, procedure and treatment results Nervenarzt. 2011 Jan;82(1):93-102 Swartz CM Electroconvulsive and neuromodulation therapies. 2009 Cambridge Univ, Cambridge New York Melbourne ECT – anesthesia: - thiopental 3-5 mg/kg - methohexital 50-120 mg - etomidate 0.15-0.3 mg/kg - propofol 1-2 mg/kg Etomidate: to use or not to use for endotracheal intubation Etomidate for intravenous induction of anaesthesia in the critically ill? Dumps C, Bolkenius D, Halbeck E. Smischney NJ, Kashyap R, Gajic O. Anaesthesist. 2017 Dec;66(12):969-980. J Thorac Dis. 2015 Sep;7(9):E347-9. Optimistic viewpoint: Raeder J., Curr Opin Anaesthesiol. 2019 Sep 9. [Epub ahead of print] Procedural sedation in ambulatory anaesthesia: what's new? This debate is ongoing … … and of course there are no long term studies in ECT patients… The theoretical problem of a cumulative risk remains, because of a „chronic“ HPA suppression with repeated use of etomidate. -

Reduction in the Incidence of Shivering with Perioperative Dexmedetomidine: a Randomized Prospective Study
[Downloaded free from http://www.joacp.org on Wednesday, August 20, 2014, IP: 218.241.189.21] || Click here to download free Android application for this journal Original Article Reduction in the incidence of shivering with perioperative dexmedetomidine: A randomized prospective study Sukhminder Jit Singh Bajwa, Sachin Gupta, Jasbir Kaur, Amarjit Singh, SS Parmar Department of Anaesthesiology and Intensive Care, Gian Sagar Medical College and Hospital, Ram Nagar, Banur, Punjab, India Abstract Background and Aims: Shivering is distressing to the patient and discomforting to the attending anesthesiologist, with a varying degree of success. Various drugs and regimens have been employed to abolish the occurrence of shivering. The present study aims to explore the effectiveness of dexmedetomidine in suppressing the postanesthetic shivering in patients undergoing general anesthesia. Materials and Methods: The present study was carried out on 80 patients, in American Society of Anesthesiologists I and II, aged 22–59 years, who underwent general anesthesia for laparoscopic surgical procedures. Patients were allocated randomly into two groups: group N (n = 40) and group D (n = 40). Group D were administered 1 μg/kg of dexmedetomidine intravenously, while group N received similar volume of saline during peri-op period. Cardiorespiratory parameters were observed and recorded during the preop, intraop, and postop periods. Any incidence of postop shivering was observed and recorded as per 4 point scale. Side effects were also observed, recorded, and treated symptomatically. Statistical analysis was carried out using statistical package for social sciences (SPSS) version 15.0 for windows and employing ANOVA and chi-square test with post-hoc comparisons with Bonferroni’s correction. -

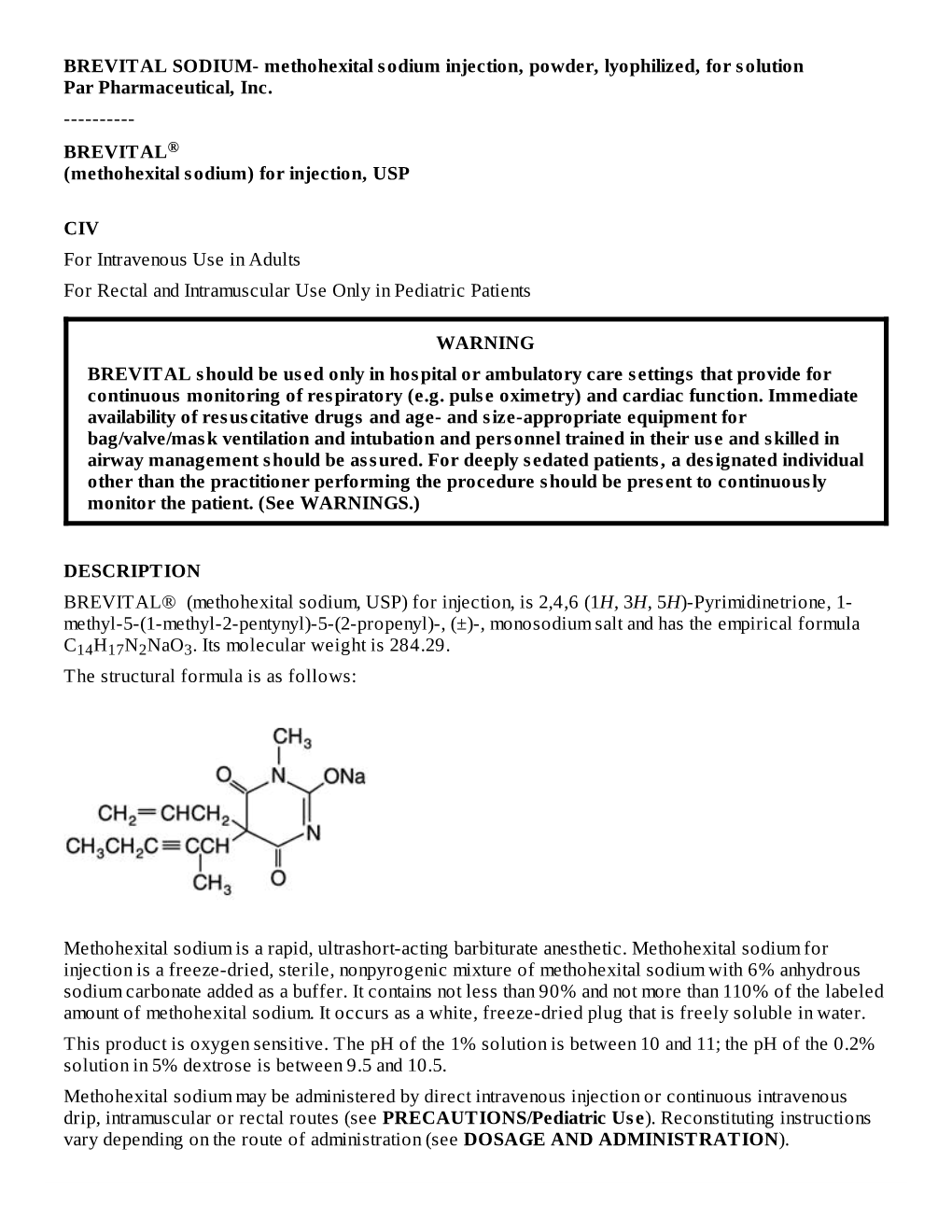
BREVITAL® (Methohexital Sodium, USP) for Injection, Is 2,4,6 (1H, 3H, 5H)-Pyrimidinetrione, 1-Methyl-5-(1-Methyl-2- Placement of the Catheter
3003014H ® BREVITAL METHOHEXITAL SODIUM FOR INJECTION, USP ® situation reevaluated. Transient blanching may or may not be noted very early; blotchy cyanosis and dark discoloration may BREVITAL then be the first sign in anesthetized patients. There is no established treatment other than prevention. The following should (methohexital sodium) for injection, USP be considered prior to injection: 1. The extent of injury is related to concentration. Concentrations of 1% methohexital will usually suffice; higher concentrations should ordinarily be avoided. 2. Check the infusion to ensure that the catheter is in the lumen of a vein before injection. Injection through a running intravenous infusion may enhance the possibility of detecting arterial placement; however, it should be remembered that the characteristic bright-red color of arterial blood is often altered by contact with drugs. The possibility of aberrant arteries should always be considered. For Intravenous Use in Adults For Rectal and Intramuscular Use Only in Pediatric Patients Post injury arterial injection of vasodilators and/or arterial infusion of parenteral fluids are generally regarded to be of no value in altering outcome. Animal experiments and published individual case reports concerned with a variety of arteriolar irritants, including barbiturates, suggest that 1 or more of the following may be of benefit in reducing the area of necrosis: WARNING BREVITAL should be used only in hospital or ambulatory care settings that provide for continuous monitoring of 1. Arterial injection of heparin at the site of injury, followed by systemic anticoagulation. respiratory (e.g. pulse oximetry) and cardiac function. Immediate availability of resuscitative drugs and age- and 2. -

Comparison of Prophylactic Use of Midazolam, Ketamine, And
British Journal of Anaesthesia 101 (4): 557–62 (2008) doi:10.1093/bja/aen205 Advance Access publication July 11, 2008 Comparison of prophylactic use of midazolam, ketamine, and ketamine plus midazolam for prevention of shivering during regional anaesthesia: a randomized double-blind placebo controlled trial A. Honarmand* and M. R. Safavi Department of Anesthesiology and Intensive Care, Isfahan University of Medical Sciences, Isfahan, Iran *Corresponding author. E-mail: [email protected] Background. Regional anaesthesia, like general anaesthesia, influences the thermoregulatory process. The aim of the present study was to compare the efficacy of low-dose prophylactic midazolam with that of placebo, ketamine, and a combination of ketamine and midazolam in the prevention of shivering caused by regional anaesthesia. Methods. In this double-blind study, 120 ASA I and II patients undergoing orthopaedic surgery were included. Subarachnoid anaesthesia was performed in all patients with bupiva- caine 15 mg. The patients were randomly allocated to receive saline (Group C), ketamine 0.5 mg (Group K), midazolam 75 mgkg21 (Group M), or ketamine 0.25 mgþmidazolam 37.5 mgkg21 (Group KM). During surgery, a shivering score was recorded at 5 min intervals. Tympanic and axillary temperature were recorded at 10 min intervals during the perioperative period. Results. After 15 min, the incidences of shivering in Groups C, M, K, and KM were 60%, 50%, 23.3%, 3.3%, respectively (P¼0.000). The differences between Group KM and Groups M, K, and C were statistically significant (P¼0.000, P¼0.026, P,0.001, respectively). The number of patients with a shivering score of 3 was significantly higher in Group C compared with Groups M, K, and KM (8 vs 4, 1, and 0, respectively, P¼0.040). -
Experience of Adverse Events with Cerebral Propofol Testing in Patients
www.nature.com/scientificreports OPEN Experience of adverse events with cerebral propofol testing in patients with drug resistant epilepsy Received: 15 March 2018 Marta Szantroch1, Aleksandra Bala1,2, Andrzej Rysz1, Jarosław Żyłkowski3 & Andrzej Marchel1 Accepted: 10 November 2018 The aim of this study was to assess the type and frequency of adverse events during the Wada test Published: xx xx xxxx conducted with propofol as an anaesthetic agent. In total, 122 patients with temporal lobe epilepsy underwent the Wada test with propofol between 2006 and 2016 as part of presurgical evaluation at the Department of Neurosurgery of the Medical University of Warsaw. The Wada test was conducted bilaterally on 118 patients (236 cases). In four cases, due to complications, the test was conducted only unilaterally, which resulted in a total of 240 cases. Those cases were further analysed for the presence of adverse events. In all cases, intracranial circulation angiography (via the transfemoral approach) was performed before memory and language testing. Of the 122 patients, adverse events were observed in 75 patients (61.4%). Serious complications were notably rare and observed only in two patients (1.6%): one patient had a carotid artery dissection, and the other had a pseudoaneurysm at the puncture site. Mild adverse events (e.g., shivers or pain of the eye) were highly common – we observed them in 71 patients (58%), but they were short-term and well-tolerated by the subjects. Two patients (1.6%) had a seizure during the Wada test. Most of the adverse events occurring during the Wada test with propofol were mild and short-lived. -

Postanaesthetic Shivering Romanian Journal of Anaesthesia and Intensive Care 2018 Vol 25 No 1, 73-81 REVIEW ARTICLE DOI
Postanaesthetic shivering Romanian Journal of Anaesthesia and Intensive Care 2018 Vol 25 No 1, 73-81 REVIEW ARTICLE DOI: http://dx.doi.org/10.21454/rjaic.7518.251.xum Postanaesthetic shivering – from pathophysiology to prevention Maria Bermudez Lopez Department of Anaesthesiology, Intensive Care Medicine and Pain Medicine, Clinic of Anaesthesia, University Hospital of Lucus Augusti, Lugo, Spain Abstract Postoperative shivering is a common complication of anaesthesia. Shivering is believed to increase oxygen consumption, increase the risk of hypoxemia, induce lactic acidosis, and catecholamine release. Therefore, it might increase the postoperative complications especially in high-risk patients. Moreover, shivering is one of the leading causes of discomfort for postsurgical patients. Shivering is usually triggered by hypothermia. However, it occurs even in normothermic patients during the perioperative period. The aetiology of shivering has been understood insufficiently. Another potential mechanism is pain and acute opioid withdrawal (especially with the use of short-acting narcotics). Besides that shivering is poorly understood, the gold standard for the treatment and prevention has not been defined yet. Perioperative hypothermia prevention is the first method to avoid shivering. Many therapeutic strategies for treating shivering exist and most are empiric. Unfortunately, the overall quality of the antishivering guidelines is low. Two main strategies are available: pharmacological and non-pharmacological antishivering methods. The combination of forced-air warming devices and intravenous meperidine is the most validated method. We also analysed different medications but final conclusion about the optimal antishivering medication is difficult to be drawn due to the lack of high-quality evidence. Nevertheless, control of PS is possible and clinically effective with simple pharmacological interventions combined with non pharmacological methods.