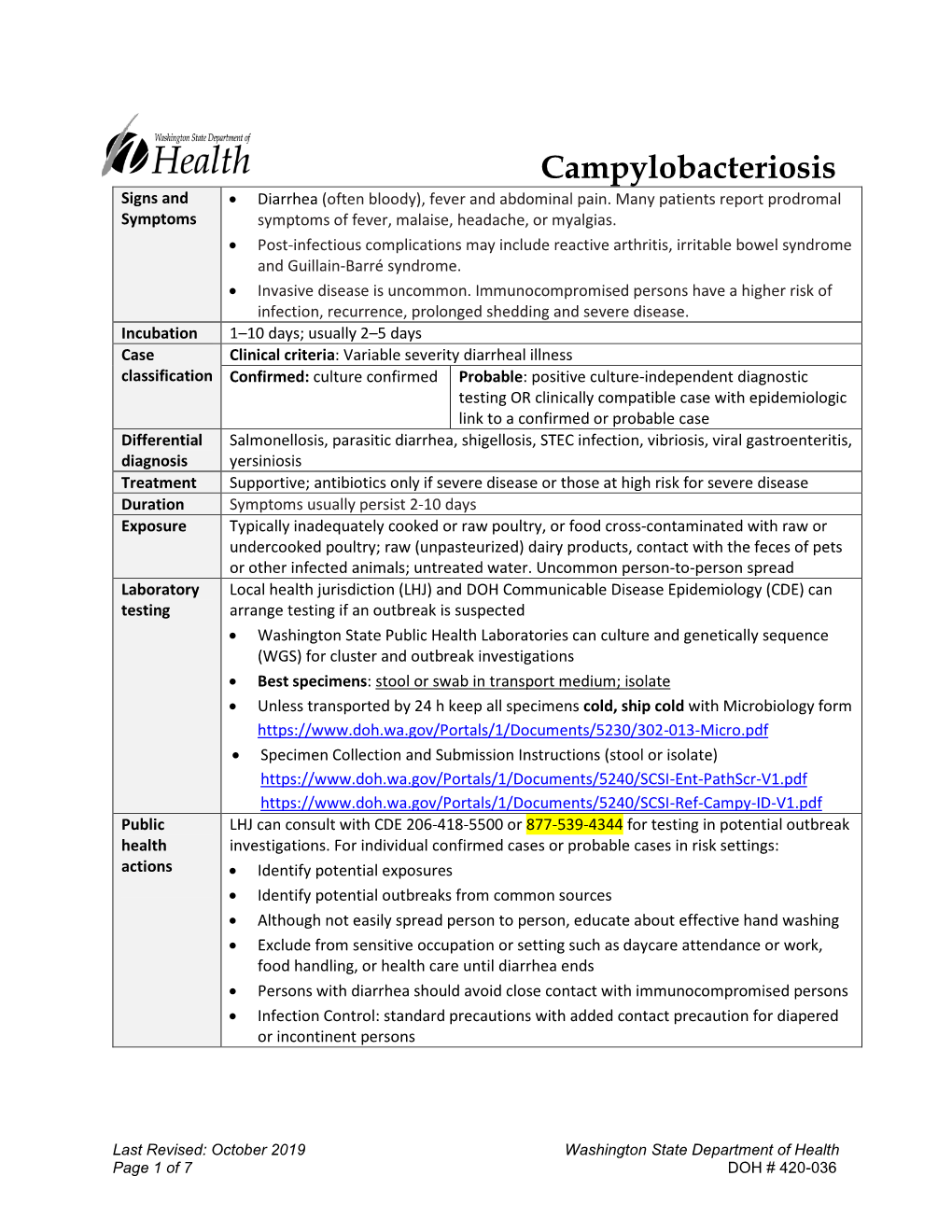
Campylobacteriosis Reporting and Investigation Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Official Nh Dhhs Health Alert
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

Case Definition for Non-Pestis Yersiniosis Check This Box If This Po
19-ID-03 Committee: Infectious Disease Title: Case Definition for Non-pestis Yersiniosis ☒Check this box if this position statement is an update to an existing standardized surveillance case definition: 18-ID-02 Synopsis: This position statement updates the case definition for non-pestis yersiniosis through the clarification of laboratory criteria. I. Statement of the Problem Non-pestis yersiniosis is an infection caused most commonly by the bacteria Yersinia enterocolitica or Yersinia pseudotuberculosis. These bacteria are normal intestinal and oropharyngeal colonizers of swine, and most commonly cause infections in children under 10 years of age, or adults over 70 years of age, through contaminated food. After Salmonella, Shigella, Campylobacter, and Shiga-toxin producing E. coli, th it is the 5 most commonly reported gastrointestinal bacterial illness reported through CDC Foodborne Diseases Active Surveillance Network (FoodNet), which monitors 10 sites in the United States for nine enteric pathogens transmitted through food. The increasing use of culture-independent diagnostic tests (CIDTs) in all parts of clinical medicine, and particularly for gastrointestinal illnesses, has also increased recognition of certain pathogens. Data from 2016 from FoodNet show a 29% increase in culture-confirmed and a 91% increase in CIDT-diagnosed Yersinia infections when compared to the 2013-2015 time frame. Yersinia enterocolitica and/or Yersinia pseudotuberculosis infections are reportable in 38 states, but no standard national definition exists for confirmed and probable cases. This position statement proposes a standardized case definition for non-pestis yersiniosis. II. Background and Justification Yersinia enterocolitica and Yersinia pseudotuberculosis are Gram negative rod-shaped or coccoid organisms that can be isolated from many animals and are most often transmitted to humans from undercooked or contaminated pork. -

Campylobacter:What You Need to Know
Queensland Health Campylobacter: what you need to know Campylobacter is one of the most Age groups most at risk common causes of foodborne illness Under in Australia. 60+ You can’t see it, smell it or even taste it on food, but if 5s it affects you, you won’t forget it. What is Campylobacter? Campylobacter is a little known foodborne bacteria similar to Salmonella. * In some cases Campylobacter can also lead to irritable 230,000 bowel syndrome, reactive arthritis and in rare cases cases a year Guillain-Barré syndrome—a type of paralysis. How do you get it? Most cases of Campylobacter infection are associated ** with eating raw or undercooked poultry or by cross 3200 contamination. hospitalisations as It is important to keep raw poultry and their juices a result of foodborne away from any already cooked or ready-to-eat foods illness caused by and fresh produce. Campylobacter Who is at risk? Anyone can be affected by Campylobacter but certain $1.25 billion people are at a greater risk for severe illness including annual total cost to society young children (under 5 years), older adults (over 60 for foodborne illness in years) and people with weakened immunity. Australia How to prevent it The easiest way to protect yourself and your family is to follow our four food safety tips every time you prepare raw poultry. ! Symptoms of Campylobacter Campylobacter infections cause gastroenteritis Follow these four safety tips (commonly known as gastro) diarrhoea, abdominal pains, cramping and fever. to prevent foodborne illness Symptoms usually start two to five days after from Campylobacter infection, and can last for one to three weeks. -

Astroviruses As Causative Agents of Gastroenteritis
Under the Microscope Astroviruses as causative agents of gastroenteritis with other enteric pathogens, especially rotaviruses, are known. Most infections in adults are asymptomatic. In other mammalian species, infection results in diarrhoea and gastroenteritis, while infection in birds leads to extraintestinal diseases, including Enzo A Palombo interstitial nephritis in young chicks and acute hepatitis in Environment and Biotechnology ducklings2. Centre Faculty of Life and Social Sciences Swinburne University of Epidemiology Technology Hawthorn VIC 3122 The first description of astrovirus came in 1975 after electron microscopic analysis of diarrhoeal stool samples from infants3,4. Astroviruses were first identified over 30 years ago and The unusual appearance of the virion particles (10% show a the virus was soon established as an important cause of characteristic five- or six-pointed star pattern on their surface) gastroenteritis, particularly in young children. Human indicated a previously unrecognised virus. Astroviruses have astrovirus disease was thought to result from infection since been reported worldwide in samples from infants and by a limited number of serotypes. However, recent young children with gastroenteritis. Soon after the first report in studies have indicated that the extent of genetic diversity humans, astrovirus-like particles were observed in domesticated is greater than previously assumed. In addition, the animals. There is now abundant evidence that astroviruses are widespread occurrence among animals and reports of widespread among domestic, synanthropic and wild animals, avian recombination and possible cross-species transmission and mammalian species in terrestrial and aquatic environments1. suggest that astroviruses have zoonotic potential. The list of animal species from which astroviruses have been Astroviruses are small (28–30 nm), non-enveloped viruses identified (chronologically) includes sheep, cattle, chickens, belonging to the family Astroviridae. -

Inflammatory Bowel Disease Irritable Bowel Syndrome
Inflammatory Bowel Disease and Irritable Bowel Syndrome Similarities and Differences 2 www.ccfa.org IBD Help Center: 888.MY.GUT.PAIN 888.694.8872 Important Differences Between IBD and IBS Many diseases and conditions can affect the gastrointestinal (GI) tract, which is part of the digestive system and includes the esophagus, stomach, small intestine and large intestine. These diseases and conditions include inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). IBD Help Center: 888.MY.GUT.PAIN 888.694.8872 www.ccfa.org 3 Inflammatory bowel diseases are a group of inflammatory conditions in which the body’s own immune system attacks parts of the digestive system. Inflammatory Bowel Disease Inflammatory bowel diseases are a group of inflamma- Causes tory conditions in which the body’s own immune system attacks parts of the digestive system. The two most com- The exact cause of IBD remains unknown. Researchers mon inflammatory bowel diseases are Crohn’s disease believe that a combination of four factors lead to IBD: a (CD) and ulcerative colitis (UC). IBD affects as many as 1.4 genetic component, an environmental trigger, an imbal- million Americans, most of whom are diagnosed before ance of intestinal bacteria and an inappropriate reaction age 35. There is no cure for IBD but there are treatments to from the immune system. Immune cells normally protect reduce and control the symptoms of the disease. the body from infection, but in people with IBD, the immune system mistakes harmless substances in the CD and UC cause chronic inflammation of the GI tract. CD intestine for foreign substances and launches an attack, can affect any part of the GI tract, but frequently affects the resulting in inflammation. -

Acute Pancreatitis Associated with Rotavirus Infection and Review Of
Case Report/Olgu Sunumu İstanbul Med J 2020; 21(1): 78-81 DO I: 10.4274/imj.galenos.2020.88319 Acute Pancreatitis Associated with Rotavirus Infection and Review of The Literature Rotavirüs Enfeksiyonuna Bağlı Akut Pankreatit Olguları ve Literatürün Gözden Geçirilmesi Kamil Şahin, Güzide Doğan University of Health Sciences, Haseki Training and Research Hospital, Department of Pediatrics, İstanbul, Turkey ABSTRACT ÖZ Agents causing acute gastroenteritis are not common causes of Çocuklarda pankreatit etiyolojisinde akut gastroenterit etkenleri pancreatitis etiology in children. Pancreatitis associated with sık görülen sebeplerden değildir. Rotavirüs enfeksiyonuna rotavirus infection is very rare. Cases with acute pancreatitis bağlı görülen pankreatit ise oldukça nadirdir. Rotavirüs during rotavirus gastroenteritis are reported due to rare gastroenteriti sırasında akut pankreatit gelişen olgular, associations. In this article, the causes of acute pancreatitis rotavirüs enfeksiyonuna bağlı akut pankreatitin nadir olması and cases of acute pancreatitis due to rotavirus infection were nedeniyle sunulmuştur. Bu yazıda, akut pankreatit sebepleri ve investigated. Clinical findings were mild, and complications rotavirüse bağlı gelişen akut pankreatit olguları incelenmiştir. were not observed in both of our patients, including a two- İki yaş kız ve üç yaşındaki erkek iki olgumuzda ve literatürde year-old female and a three-year-old male, and other cases değerlendirilen diğer olgularda klinik bulgular hafif seyretmiş, evaluated in the literature. The -

Hepatitis C – Screening, Diagnosis, Management & Treatment
12 Osteopathic Family Physician (2019) 12 - 19 Osteopathic Family Physician | Volume 11, No. 1 | January/February, 2019 Review ARTICLE Hepatitis C – Screening, Diagnosis, Management & Treatment Michael Ferraro, DO & Matthew StantsPainter, DO Washington Health System Family Medicine Residency Program, Washington, PA KEYWORDS: Abstract: Hepatitis C virus (HCV) infection is a major cause of chronic liver disease, hepatocellular carcinoma and cirrhosis with at least 185 million people infected worldwide, causing 399,000 deaths Disease Prevention annually. HCV is transmitted through blood or body fluids. Transmission most commonly occurs and Wellness through sharing of injection drug, occupational exposure through needlestick injuries in healthcare Hepatitis C settings, and birth to an HCV infected mother. There are seven known genotypes of HCV, 1a, 1b, 2, 3, 4, 5, and 6, with the most common genotypes in the U.S. being 1a, 1b, 2, and 3, which comprise Infectious Disease approximately 97% of all U.S. HCV infections. Risks for disease progression include baseline liver histology, age, ethnicity, gender, alcohol use, comorbidities and immune response. There are Jaundice multiple screening recommendations currently in place, some of which are based on risk factors, Transaminitis with others based on legislation. The screening test of choice is the anti-Hepatitis C virus antibody, with a confirmatory HCV RNA PCR with genotyping. Once the diagnosis is made, assessing the level of fibrosis and/or cirrhosis is an important step in determining the pathway to treatment. There are multiple new options for treatment with improved efficacy and less side effects. Patient being treated for HCV should be monitored and assessed for compliance with therapy and adverse effects, including new or worsening psychiatric illness and screened for alcohol and substance abuse. -

Acute Gastroenteritis
Article gastrointestinal disorders Acute Gastroenteritis Deise Granado-Villar, MD, Educational Gap MPH,* Beatriz Cunill-De Sautu, MD,† Andrea In managing acute diarrhea in children, clinicians need to be aware that management Granados, MDx based on “bowel rest” is outdated, and instead reinstitution of an appropriate diet has been associated with decreased stool volume and duration of diarrhea. In general, drug therapy is not indicated in managing diarrhea in children, although zinc supplementation Author Disclosure and probiotic use show promise. Drs Granado-Villar, Cunill-De Sautu, and Objectives After reading this article, readers should be able to: Granados have disclosed no financial 1. Recognize the electrolyte changes associated with isotonic dehydration. relationships relevant 2. Effectively manage a child who has isotonic dehydration. to this article. This 3. Understand the importance of early feedings on the nutritional status of a child who commentary does has gastroenteritis. contain a discussion of 4. Fully understand that antidiarrheal agents are not indicated nor recommended in the an unapproved/ treatment of acute gastroenteritis in children. investigative use of 5. Recognize the role of vomiting in the clinical presentation of acute gastroenteritis. a commercial product/ device. Introduction Acute gastroenteritis is an extremely common illness among infants and children world- wide. According to the Centers for Disease Control and Prevention (CDC), acute diarrhea among children in the United States accounts for more than 1.5 million outpatient visits, 200,000 hospitalizations, and approximately 300 deaths per year. In developing countries, diarrhea is a common cause of mortality among children younger than age 5 years, with an estimated 2 million deaths each year. -

Treating Opportunistic Infections Among HIV-Infected Adults and Adolescents
Morbidity and Mortality Weekly Report Recommendations and Reports December 17, 2004 / Vol. 53 / No. RR-15 Treating Opportunistic Infections Among HIV-Infected Adults and Adolescents Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/ Infectious Diseases Society of America INSIDE: Continuing Education Examination department of health and human services Centers for Disease Control and Prevention MMWR CONTENTS The MMWR series of publications is published by the Epidemiology Program Office, Centers for Disease Introduction......................................................................... 1 Control and Prevention (CDC), U.S. Department of How To Use the Information in This Report .......................... 2 Health and Human Services, Atlanta, GA 30333. Effect of Antiretroviral Therapy on the Incidence and Management of OIs .................................................... 2 SUGGESTED CITATION Initiation of ART in the Setting of an Acute OI Centers for Disease Control and Prevention. Treating (Treatment-Naïve Patients) ................................................. 3 Management of Acute OIs in the Setting of ART .................. 4 opportunistic infections among HIV-infected adults and When To Initiate ART in the Setting of an OI ........................ 4 adolescents: recommendations from CDC, the National Special Considerations During Pregnancy ........................... 4 Institutes of Health, and the HIV Medicine Association/ Disease Specific Recommendations .................................... -
Food Safety Labelling of Chicken to Prevent Campylobacteriosis: Consumer Expectations and Current Practices Philip D
Allan et al. BMC Public Health (2018) 18:414 https://doi.org/10.1186/s12889-018-5322-z RESEARCH ARTICLE Open Access Food safety labelling of chicken to prevent campylobacteriosis: consumer expectations and current practices Philip D. Allan†, Chloe Palmer†, Fiona Chan, Rebecca Lyons, Olivia Nicholson, Mitchell Rose, Simon Hales and Michael G. Baker* Abstract Background: Campylobacter is the leading cause of bacterial gastroenteritis worldwide, and contaminated chicken is a significant vehicle for spread of the disease. This study aimed to assess consumers’ knowledge of safe chicken handling practices and whether their expectations for food safety labelling of chicken are met, as a strategy to prevent campylobacteriosis. Methods: We conducted a cross-sectional survey of 401 shoppers at supermarkets and butcheries in Wellington, New Zealand, and a systematic assessment of content and display features of chicken labels. Results: While 89% of participants bought, prepared or cooked chicken, only 15% knew that most (60–90%) fresh chicken in New Zealand is contaminated by Campylobacter. Safety and correct preparation information on chicken labels, was rated ‘very necessary’ or ‘essential’ by the majority of respondents. Supermarket chicken labels scored poorly for the quality of their food safety information with an average of 1.7/5 (95% CI, 1.4–2.1) for content and 1.8/ 5 (95% CI, 1.6–2.0) for display. Conclusions: Most consumers are unaware of the level of Campylobacter contamination on fresh chicken and there is a significant but unmet consumer demand for information on safe chicken preparation on labels. Labels on fresh chicken products are a potentially valuable but underused tool for campylobacteriosis prevention in New Zealand. -

Campylobacteriosis: a Global Threat
ISSN: 2574-1241 Volume 5- Issue 4: 2018 DOI: 10.26717/BJSTR.2018.11.002165 Muhammad Hanif Mughal. Biomed J Sci & Tech Res Review Article Open Access Campylobacteriosis: A Global Threat Muhammad Hanif Mughal* Homeopathic Clinic, Rawalpindi, Islamabad, Pakistan Received: : November 30, 2018; Published: : December 10, 2018 *Corresponding author: Muhammad Hanif Mughal, Homeopathic Clinic, Rawalpindi-Islamabad, Pakistan Abstract Campylobacter species account for most cases of human gastrointestinal infections worldwide. In humans, Campylobacter bacteria cause illness called campylobacteriosis. It is a common problem in the developing and industrialized world in human population. Campylobacter species extensive research in many developed countries yielded over 7500 peer reviewed articles. In humans, most frequently isolated species had been Campylobacter jejuni, followed by Campylobactercoli Campylobacterlari, and lastly Campylobacter fetus. C. jejuni colonizes important food animals besides chicken, which also includes cattle. The spread of the disease is allied to a wide range of livestock which include sheep, pigs, birds and turkeys. The organism (5-18.6 has% of been all Campylobacter responsible for cases) diarrhoea, in an estimated 400 - 500 million people globally each year. The most important Campylobacter species associated with human infections are C. jejuni, C. coli, C. lari and C. upsaliensis. Campylobacter colonize the lower intestinal tract, including the jejunum, ileum, and colon. The main sources of these microorganisms have been traced in unpasteurized milk, contaminated drinking water, raw or uncooked meat; especially poultry meat and contact with animals. Keywords: Campylobacteriosis; Gasteritis; Campylobacter jejuni; Developing countries; Emerging infections; Climate change Introduction of which C. jejuni and 12 species of C. coli have been associated with Campylobacter cause an illness known as campylobacteriosis is a common infectious problem of the developing and industrialized world. -

Preventing Foodborne Illness: Yersiniosis1 Aswathy Sreedharan, Correy Jones, and Keith Schneider2
FSHN12-09 Preventing Foodborne Illness: Yersiniosis1 Aswathy Sreedharan, Correy Jones, and Keith Schneider2 What is yersiniosis? Yersiniosis is an infectious disease caused by the con- sumption of contaminated food contaminated with the bacterium Yersinia. Most foodborne infections in the US resulting from ingestion of Yersinia species are caused by Y. enterocolitica. Yersiniosis is characterized by common symptoms of gastroenteritis such as abdominal pain and mild fever (8). Most outbreaks are associated with improper food processing techniques, including poor sanitation and improper sterilization techniques by food handlers. The dis- ease is also spread by the fecal–oral route, i.e., an infected person contaminating surfaces and transmitting the disease to others by not washing his or her hands thoroughly after Figure 1. Yersinia enterocolitica bacteria growing on a Xylose Lysine going to the bathroom. The bacterium is prevalent in the Sodium Deoxycholate (XLD) agar plate. environment, enabling it to contaminate our water and Credits: CDC Public Health Image Library (ID# 6705). food systems. Outbreaks of yersiniosis have been associated with unpasteurized milk, oysters, and more commonly with What is Y. enterocolitica? consumption of undercooked dishes containing pork (8). Yersinia enterocolitica is a small, rod-shaped, Gram- Yersiniosis incidents have been documented more often negative, psychrotrophic (grows well at low temperatures) in Europe and Japan than in the United States where it is bacterium. There are approximately 60 serogroups of Y. considered relatively rare. According to the Centers for enterocolitica, of which only 11 are infectious to humans. Disease Control and Prevention (CDC), approximately Of the most common serogroups—O:3, O:8, O:9, and one confirmed Y.