Heavy Menstrual Bleeding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FLOW (Finding Lasting Options for Women) Multicentre Randomized Controlled Trial Comparing Tampons with Menstrual Cups
Research | Web exclusive FLOW (finding lasting options for women) Multicentre randomized controlled trial comparing tampons with menstrual cups Courtney Howard MD CCFP(EM) Caren Lee Rose MSc Konia Trouton MD CCFP MPH Holly Stamm MD CCFP Danielle Marentette MD CCFP Nicole Kirkpatrick MD CCFP(EM) Sanja Karalic MD CCFP MSc Renee Fernandez MD CCFP Julie Paget MD CCFP Abstract Objective To determine whether menstrual cups are a viable alternative to tampons. Design Randomized controlled trial. EDITOR’S KEY POINTS Setting Prince George, Victoria, and Vancouver, BC. • Patients are increasingly asking physicians about more environmentally friendly Participants A total of 110 women aged 19 to 40 years who had previously alternatives to disposable menstrual used tampons as their main method of menstrual management. management products, particularly menstrual cups, and about their Intervention Participants were randomized into 2 groups, a tampon group effectiveness compared with tampons. and a menstrual cup group. Using online diaries, participants tracked 1 Although the safety and efficacy of menstrual cycle using their regular method and 3 menstrual cycles using menstrual cups have been studied the method of their allocated group. previously, a randomized controlled trial comparing cups with tampons has never Main outcome measures Overall satisfaction; secondary outcomes been done. included discomfort, urovaginal infection, cost, and waste. • This study compared the experiences of Results Forty-seven women in each group completed the final survey, 5 of women using only tampons with women whom were subsequently excluded from analysis (3 from the tampon group using only menstrual cups over a period and 2 from the menstrual cup group). -

Why Menstrual Hygiene Products Should Be Provided for Free in Restrooms
University of Miami Law Review Volume 73 Number 1 Fall 2018 Article 10 10-30-2018 The Bring Your Own Tampon Policy: Why Menstrual Hygiene Products Should Be Provided for Free in Restrooms Elizabeth Montano Follow this and additional works at: https://repository.law.miami.edu/umlr Part of the Human Rights Law Commons Recommended Citation Elizabeth Montano, The Bring Your Own Tampon Policy: Why Menstrual Hygiene Products Should Be Provided for Free in Restrooms, 73 U. Miami L. Rev. 370 (2018) Available at: https://repository.law.miami.edu/umlr/vol73/iss1/10 This Note is brought to you for free and open access by the Journals at University of Miami School of Law Institutional Repository. It has been accepted for inclusion in University of Miami Law Review by an authorized editor of University of Miami School of Law Institutional Repository. For more information, please contact [email protected]. The Bring Your Own Tampon Policy: Why Menstrual Hygiene Products Should Be Provided for Free in Restrooms ELIZABETH MONTANO* Like toilet paper, menstrual hygiene products,1 such as tampons and pads, are necessities for managing natural and unavoidable bodily functions. However, menstrual hygiene products widely receive separate treatment in restrooms across the globe. While it would be absurd today to carry a roll of toilet paper at all times, it is considered necessary and common sense for all menstruators to carry menstrual hy- giene products at all times, for approximately forty years, in case of an emergency. This is the “Bring Your Own * Editor-in-Chief, University of Miami Law Review, Volume 73; J.D. -

Epidemiology of Menstrual Disorders in Developing Countries: a Systematic Review
BJOG: an International Journal of Obstetrics and Gynaecology DOI: 10.1046/j.1471-0528.2003.00012.x January 2004, Vol. 111, pp. 6–16 REVIEW Epidemiology of menstrual disorders in developing countries: a systematic review Introduction Information on the prevalence of menstrual complaints in the past three months was obtained in seven countries In developing countries, priority setting in the health (Table 1). These data permit cross national comparisons sector traditionally focuses on the principal causes of mor- in so far as similar questions with a similar time reference tality. More recently, the Global Burden of Disease approach were asked. However, no definitions were provided and incorporates assessment of morbidity and quality of life in considerable variation in the interpretation of questions identifying priorities. Yet, although investigations in various among individuals and across cultures is likely. developing countries reveal that women are concerned by Approximately a dozen subsequent surveys, including menstrual disorders, little attention is paid to understanding community-based, clinic-based and one national census, or ameliorating women’s menstrual complaints.1 Menstrual include some information on menstrual morbidities6–29 dysfunction, like other aspects of sexual and reproductive (Table 2). A few health surveys of special populations, health, is not included in the Global Burden of Disease such as factory workers in Vietnam17 and medical students estimates2,3 and, even as reproductive health programs in Venezuela,27,28 have also included relevant questions expand their focus to address gynaecologic morbidity, the on menstrual disorders. These surveys vary consider- utility of evaluating and treating menstrual problems is ably in the definition of and reference period for men- not generally considered. -

Changes Before the Change1.06 MB
Changes before the Change Perimenopausal bleeding Although some women may abruptly stop having periods leading up to the menopause, many will notice changes in patterns and irregular bleeding. Whilst this can be a natural phase in your life, it may be important to see your healthcare professional to rule out other health conditions if other worrying symptoms occur. For further information visit www.imsociety.org International Menopause Society, PO Box 751, Cornwall TR2 4WD Tel: +44 01726 884 221 Email: [email protected] Changes before the Change Perimenopausal bleeding What is menopause? Strictly defined, menopause is the last menstrual period. It defines the end of a woman’s reproductive years as her ovaries run out of eggs. Now the cells in the ovary are producing less and less hormones and menstruation eventually stops. What is perimenopause? On average, the perimenopause can last one to four years. It is the period of time preceding and just after the menopause itself. In industrialized countries, the median age of onset of the perimenopause is 47.5 years. However, this is highly variable. It is important to note that menopause itself occurs on average at age 51 and can occur between ages 45 to 55. Actually the time to one’s last menstrual period is defined as the perimenopausal transition. Often the transition can even last longer, five to seven years. What hormonal changes occur during the perimenopause? When a woman cycles, she produces two major hormones, Estrogen and Progesterone. Both of these hormones come from the cells surrounding the eggs. Estrogen is needed for the uterine lining to grow and Progesterone is produced when the egg is released at ovulation. -

Guide to Menstrual Hygiene Materials May 2019
Guide to menstrual hygiene materials May 2019 First edition Supply Division / Water, Sanitation & Education Centre Programme Division / Water, Sanitation & Hygiene 3 United Nations Plaza New York, NY 10017 USA www.unicef.org Commentaries represent the personal views of the authors and do not necessarily reflect the positions of the United Nations Children’s Fund (UNICEF). The designations employed in this publication and the presentation of the material do not imply on the part of UNICEF the expression of any opinion whatsoever concerning the legal status of any country or territory, or of its authorities or the delimitations of its frontiers. Edited by Phil Poirier and designed by Noha Habaieb Cover illustration credits : © Noha Habaieb For more information on this document, please contact: Anne Cabrera-Clerget, Contracts Manager [email protected] Brooke Yamakoshi, WASH Specialist, [email protected] Guide to menstrual hygiene materials Contents Acknowledgements 6 Key terms 7 Overview 8 Introduction 9 Procuring menstrual hygiene materials and supplies 12 Consulting with girls and women 16 Understanding menstrual hygiene materials 20 Menstrual cloth 22 Reusable pad 24 Disposable sanitary pad 26 Tampon 28 Menstrual Cup 30 Summary of materials 32 Monitoring and learning 34 Annex I: Additional resources 36 Guide to menstrual hygiene materials 5 © UNICEF/UNI132359/Nesbitt Guide to menstrual hygiene materials Acknowledgements This guidance was prepared by Sophia Roeckel, menstrual hygiene management intern, Anne Cabrera-Clerget, -

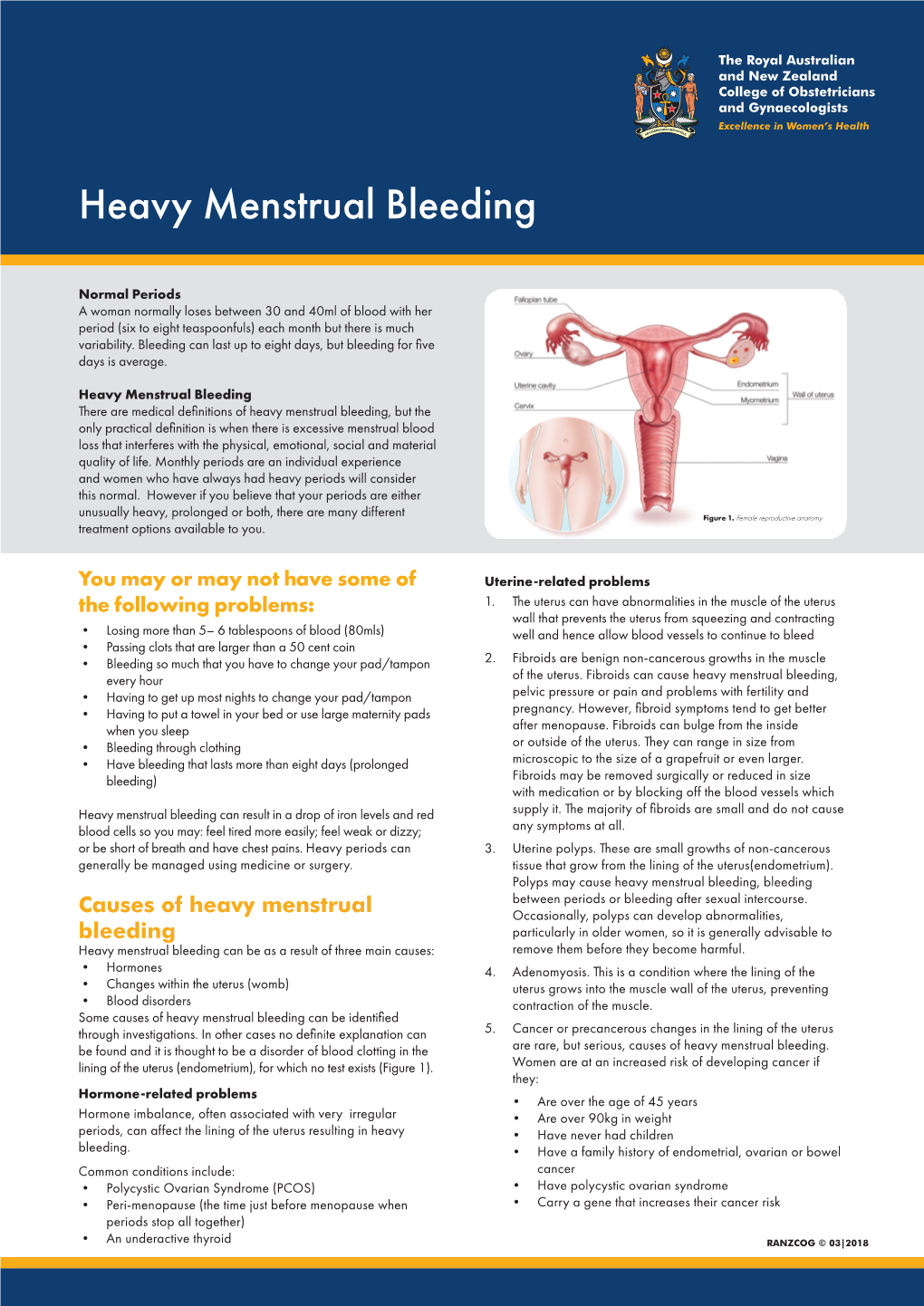
Heavy Menstrual Bleeding
25/06/2018 Definition • Heavy menstrual bleeding (HMB) is defined as excessive menstrual blood loss which interferes with a woman's physical, social, emotional and/or material quality of life. Heavy Menstrual Bleeding (HMB): Replaced ‘menorrhagia’ Objective definition of HMB >80mL/ cycle or duration of >7 days Causes and Management • It can occur alone or in combination with other symptoms (e.g. intermenstrual bleeding, pelvic pain, pressure symptoms) Dr. William (Wee-Liak) Hoo, MD MRCOG Consultant Gynaecologist Prevalence King’s College Hospital NHS FT • The prevalence of HMB in objective studies (9 to 14%) and subjective studies 20 to 52%) in studies based on subjective assessment. • In the UK, almost 1.5 million women consult their General Practitioners UKCPA Women’s Health Group Masterclass (GPs) each year with menstrual complaints and the annual treatment cost Friday 22nd June 2018 exceeds £65 million. Causes • Uterine: Uterine fibroids (dysmenorrhoea, palpable mass, pressure symptoms) Adenomyosis (dysmenorrhoea, subfertility) Endometrial polyps (intermenstrual bleeding) Pelvic inflammatory disease (PID)/ infection (vaginal discharge, pelvic pain, intermenstrual and postcoital bleeding and pyrexia) Malignancy or atypical hyperplasia (irregular/ postcoital/ intermenstrual bleeding, pelvic pain, weight loss). • Ovarian: Polycystic ovary syndrome (acne, hursuitism) • Systemic diseases: Hypothyroidism (fatigue, constipation, cold intolerance and hair and skin changes) Coagulation disorders (e.g. von Willebrand disease) Liver -

Abnormal Uterine Bleeding: a Management Algorithm
J Am Board Fam Med: first published as 10.3122/jabfm.19.6.590 on 7 November 2006. Downloaded from EVIDENCED-BASED CLINICAL MEDICINE Abnormal Uterine Bleeding: A Management Algorithm John W. Ely, MD, MSPH, Colleen M. Kennedy, MD, MS, Elizabeth C. Clark, MD, MPH, and Noelle C. Bowdler, MD Abnormal uterine bleeding is a common problem, and its management can be complex. Because of this complexity, concise guidelines have been difficult to develop. We constructed a concise but comprehen- sive algorithm for the management of abnormal uterine bleeding between menarche and menopause that was based on a systematic review of the literature as well as the actual management of patients seen in a gynecology clinic. We started by drafting an algorithm that was based on a MEDLINE search for rel- evant reviews and original research. We compared this algorithm to the actual care provided to a ran- dom sample of 100 women with abnormal bleeding who were seen in a university gynecology clinic. Discrepancies between the algorithm and actual care were discussed during audiotaped meetings among the 4 investigators (2 family physicians and 2 gynecologists). The audiotapes were used to revise the algorithm. After 3 iterations of this process (total of 300 patients), we agreed on a final algorithm that generally followed the practices we observed, while maintaining consistency with the evidence. In clinic, the gynecologists categorized the patient’s bleeding pattern into 1 of 4 types: irregular bleeding, heavy but regular bleeding (menorrhagia), severe acute bleeding, and abnormal bleeding associated with a contraceptive method. Subsequent management involved both diagnostic and treatment interven- tions, which often occurred simultaneously. -

Download Article (PDF)
DE GRUYTER International Journal of Adolescent Medicine and Health. 2020; 20190179 Miriam R. Singer1 / Nikita Sood1 / Eli Rapoport1 / Haelynn Gim1 / Andrew Adesman1,2 / Ruth Milanaik1,2,3 Pediatricians’ knowledge, attitudes and practices surrounding menstruation and feminine products 1 Department of Pediatrics, Steven and Alexandra Cohen Children’s Medical Center of New York, Lake Success, NY,USA, E- mail: [email protected]. https://orcid.org/0000-0002-2352-702X. 2 Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY,USA, E-mail: [email protected]. https://orcid.org/0000-0002-2352-702X. 3 Division of Developmental and Behavioral Pediatrics, Steven and Alexandra Cohen Children’s Medical Center of New York, 1983 Marcus Avenue, Suite 130, Lake Success, NY 11042, USA, Phone: +516-802-6100, Fax: +516-802-6131, E-mail: [email protected] Abstract: Objective: This study investigates whether primary care pediatricians adhere to the American Academy of Pediatrics (AAP) recommendations by routinely evaluating patients’ menstrual cycles and educating patients about menstruation and feminine products. Additionally, this study examines pediatricians’ knowledge and attitudes surrounding menstrual health topics. Methods: A 53-item online questionnaire was developed to evaluate pediatricians’ knowledge, attitudes and clinical practices regarding menstruation-related topics. The questionnaire was emailed to 2500 AAP mem- bers using a geographically-stratified sampling approach, with pediatricians in each state selected randomly. Mann-Whitney U tests, t-tests, and logistic regressions were used to assess associations between correlates and pediatricians’ knowledge, attitudes and practices. Results: Five hundred and eighteen out of 2500 pediatricians participated (response rate = 20.7%), 462 met inclusion criteria; 78.8% were female, 79.2% were Caucasian. -

Dell Childrens Hospital
DELL CHILDREN’S MEDICAL CENTER EVIDENCE-BASED OUTCOMES CENTER Abnormal Uterine Bleeding Heavy Menstrual Bleeding in Adolescents LEGAL DISCLAIMER: The information provided by Dell Children’s Medical Center of Texas (DCMCT), including but not limited to Clinical Pathways and Guidelines, protocols and outcome data, (collectively the "Information") is presented for the purpose of educating patients and providers on various medical treatment and management. The Information should not be relied upon as complete or accurate; nor should it be relied on to suggest a course of treatment for a particular patient. The Clinical Pathways and Guidelines are intended to assist physicians and other health care providers in clinical decision-making by describing a range of generally acceptable approaches for the diagnosis, management, or prevention of specific diseases or conditions. These guidelines should not be considered inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the same results. The ultimate judgment regarding care of a particular patient must be made by the physician in light of the individual circumstances presented by the patient. DCMCT shall not be liable for direct, indirect, special, incidental or consequential damages related to the user's decision to use this information contained herein. Definition: sexually active, including consensual and coerced sex7. An acute episode of heavy menstrual bleeding is one that, in Specific questions should be asked to determine possibility of the opinion of the clinician, is of sufficient quantity to require bleeding/coagulation disorder (see Table 2 in Addendum 1). immediate intervention to prevent future blood loss1. -

The Unequal Price of Periods Menstrual Equity in the United States
The Unequal Price of Periods Menstrual Equity in the United States as allowable budgetary expenses for publicly funded Introduction schools, shelters, or crisis and emergency centers. They are not provided in a consistent or fully accessible On any given day, there are 800,000,000 people on way in correction and detention facilities. Menstrual the planet who are menstruating, of whom at least products are not covered by public health and 500,000,000 lack adequate resources — basic supplies, nutritional benefits programs, nor made uniformly facilities, information, and support — for managing available in schools or workplaces. And in 33 states, their periods.1 menstrual products are not exempt from sales taxes.5 Until very recently this issue had been given little Equity-based arguments — and the term “menstrual consideration in U.S. policies and laws. It is an equity,” coined by author Jennifer Weiss-Wolf — yield omission that affects everyone, but hits hardest the the most powerful narrative for countering the populations for whom access and agency is most inconsistencies and oversights that currently exist compromised: in American law and public policy. Indeed, this is the • For the nearly one in five American teenagers heart of the formal definition of menstrual equity set who live in poverty,2 lack of menstrual products forth in her book, “Periods Gone Public”: and support can lead to lost educational In order to have a fully equitable and opportunity. participatory society, we must have laws and • Those experiencing homelessness report policies that ensure menstrual products are infection caused by using tampons and pads for safe and affordable for everyone who needs longer than recommended or by improvising them. -

FAQ049 -- Your First Period
AQ The American College of Obstetricians and Gynecologists FREQUENTLY ASKED QUESTIONS FAQ049 fESPECIALLY FOR TEENS Your First Period • What is puberty? • What is a menstrual period? • When will I start my period? • How long do periods last? • How often will I get my period? • Why is it a good idea to track my period? • How can I track my period on a calendar? • What personal care products are available for me during my menstrual period? • How are pads used? • How often should I change my pad? • How are tampons used? • How do I choose a tampon? • How often should I change my tampon? • What are menstrual cups? • Does having a period cause pain or discomfort? • What is amenorrhea? • What if I am having heavy bleeding? • What if I have irregular periods? • Glossary What is puberty? Puberty is a time when your body begins to change to become more like an adult’s. Starting your menstrual period is one of these changes. What is a menstrual period? When puberty begins, your brain signals your body to produce hormones. Some of these hormones prepare your body each month for a possible pregnancy. This is called the menstrual cycle. Hormones cause the lining of the uterus to become thicker with extra blood and tissue. One of your ovaries then releases an egg. This is called ovulation. The egg moves down one of the two fallopian tubes toward the uterus. If the egg is not fertilized with a man’s sperm, pregnancy does not occur. The lining of the uterus breaks down and flows out of the body through your vagina. -

Dysmenorrhea
Pediatric & Adolescent Gynecology & Obstetrics Dysmenorrhea (Painful Periods) Defining Dysmenorrhea Painful menstruation — dysmenorrhea — is the most common menstrual disorder, with up to 90 percent of adolescent women experiencing pain with menses. Dysmenorrhea can be both primary and secondary in cause, and both forms are amenable to treatment. Primary dysmenorrhea is defined as painful menstruation in the absence of specific organic pathology, while secondary dysmenorrhea is related to conditions of the pelvic organs and may become worse over time. When a patient has painful periods, she and her family may be worried that it is a sign of a serious problem, such as cancer, or a threat to their reproductive potential. The vast majority of adolescents presenting with painful menses have primary dysmenorrhea and respond well to medical interventions. Conditions Associated With Secondary Dysmenorrhea Condition Description Endometriosis Tissue that normally lines the inside of the uterus grows outside the uterus, most commonly around the ovaries, intestines or other pelvic organs Müllerian duct anomalies Congenital (developmental) anomalies of the reproductive tract in which menstrual egress may be blocked Adenomyosis Tissue that normally lines the inside of the uterine cavity grows into the muscular wall of the uterus Fibroids Noncancerous growths of the uterus Salpingitis Inflammation of the fallopian tubes Pelvic adhesions Bands of scar tissue that can cause internal organs to be stuck together when they are not supposed to be Determining a Cause Referral Note: For any tests, procedures or imaging that are outside the scope of your regular pediatric or general practice, please refer the patient to Pediatric and Adolescent Gynecology at Nationwide Children’s Hospital.