Expression Patterns of T1R3 in Duodenal Epithelial Cells with Some Gastrointestinal Hormone*
Total Page:16
File Type:pdf, Size:1020Kb
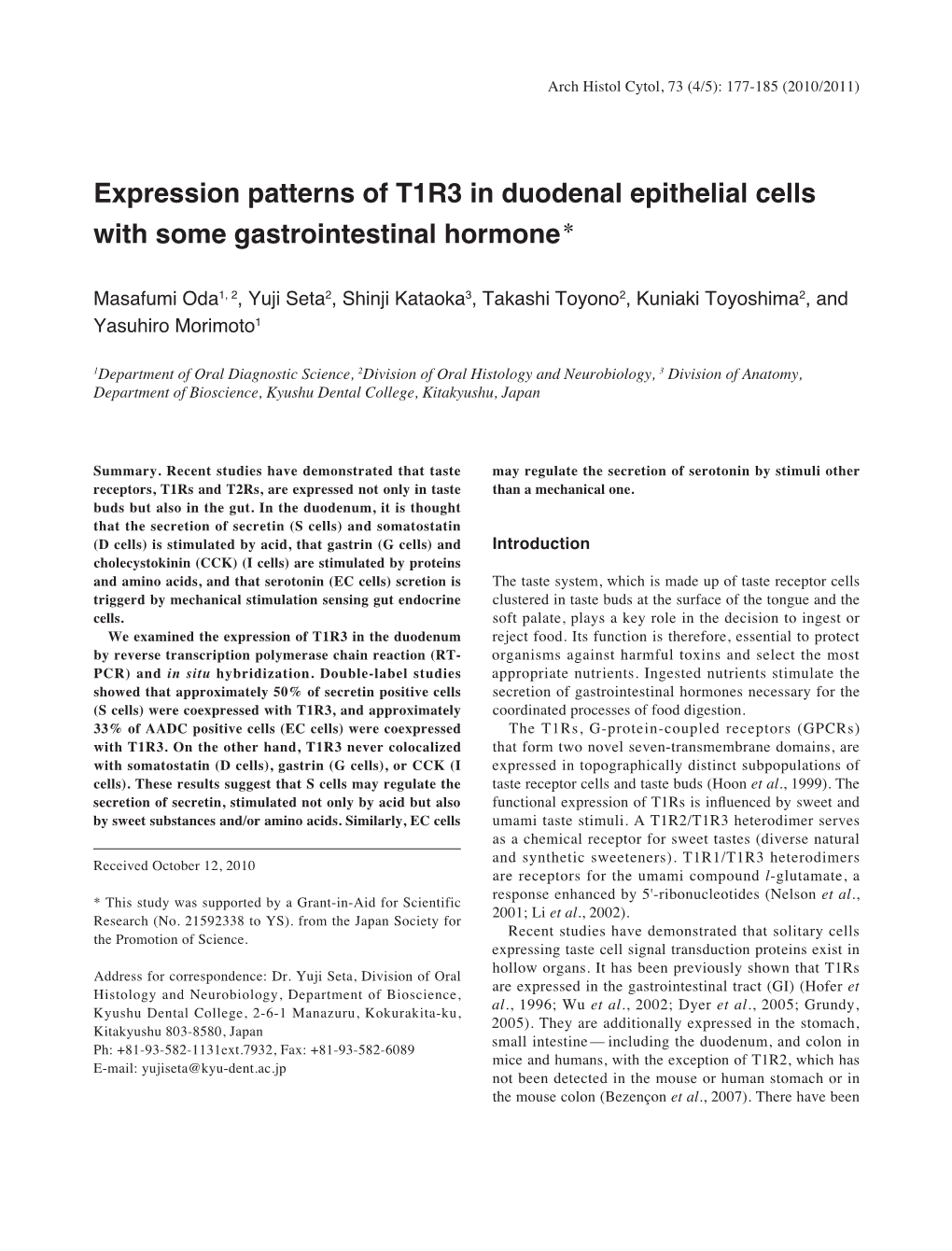
Load more
Recommended publications
-

Cells Using Gene Expression Profiling and Insulin Gene Methylation
RESEARCH ARTICLE Comparison of enteroendocrine cells and pancreatic β-cells using gene expression profiling and insulin gene methylation ☯ ☯ Gyeong Ryul Ryu , Esder Lee , Jong Jin Kim, Sung-Dae MoonID, Seung-Hyun Ko, Yu- Bae Ahn, Ki-Ho SongID* Division of Endocrinology & Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea ☯ These authors contributed equally to this work. a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 a1111111111 Abstract Various subtypes of enteroendocrine cells (EECs) are present in the gut epithelium. EECs and pancreatic β-cells share similar pathways of differentiation during embryonic develop- ment and after birth. In this study, similarities between EECs and β-cells were evaluated in OPEN ACCESS detail. To obtain specific subtypes of EECs, cell sorting by flow cytometry was conducted Citation: Ryu GR, Lee E, Kim JJ, Moon S-D, Ko S- from STC-1 cells (a heterogenous EEC line), and each single cell was cultured and pas- H, Ahn Y-B, et al. (2018) Comparison of saged. Five EEC subtypes were established according to hormone expression, measured enteroendocrine cells and pancreatic β-cells using by quantitative RT-PCR and immunostaining: L, K, I, G and S cells expressing glucagon-like gene expression profiling and insulin gene methylation. PLoS ONE 13(10): e0206401. https:// peptide-1, glucose-dependent insulinotropic polypeptide, cholecystokinin, gastrin and doi.org/10.1371/journal.pone.0206401 secretin, respectively. Each EEC subtype was found to express not only the corresponding Editor: Wataru Nishimura, International University gut hormone but also other gut hormones. Global microarray gene expression profiles of Health and Welfare School of Medicine, JAPAN revealed a higher similarity between each EEC subtype and MIN6 cells (a β-cell line) than Received: March 29, 2018 between C2C12 cells (a myoblast cell line) and MIN6 cells, and all EEC subtypes were highly similar to each other. -

Enteric Nervous System (ENS): 1) Myenteric (Auerbach) Plexus & 2
Enteric Nervous System (ENS): 1) Myenteric (Auerbach) plexus & 2) Submucosal (Meissner’s) plexus à both triggered by sensory neurons with chemo- and mechanoreceptors in the mucosal epithelium; effector motors neurons of the myenteric plexus control contraction/motility of the GI tract, and effector motor neurons of the submucosal plexus control secretion of GI mucosa & organs. Although ENS neurons can function independently, they are subject to regulation by ANS. Autonomic Nervous System (ANS): 1) parasympathetic (rest & digest) – can innervate the GI tract and form connections with ENS neurons that promote motility and secretion, enhancing/speeding up the process of digestion 2) sympathetic (fight or flight) – can innervate the GI tract and inhibit motility & secretion by inhibiting neurons of the ENS Sections and dimensions of the GI tract (alimentary canal): Esophagus à ~ 10 inches Stomach à ~ 12 inches and holds ~ 1-2 L (full) up to ~ 3-4 L (distended) Duodenum à first 10 inches of the small intestine Jejunum à next 3 feet of small intestine (when smooth muscle tone is lost upon death, extends to 8 feet) Ileum à final 6 feet of small intestine (when smooth muscle tone is lost upon death, extends to 12 feet) Large intestine à 5 feet General Histology of the GI Tract: 4 layers – Mucosa, Submucosa, Muscularis Externa, and Serosa Mucosa à epithelium, lamina propria (areolar connective tissue), & muscularis mucosae Submucosa à areolar connective tissue Muscularis externa à skeletal muscle (in select parts of the tract); smooth muscle (at least 2 layers – inner layer of circular muscle and outer layer of longitudinal muscle; stomach has a third layer of oblique muscle under the circular layer) Serosa à superficial layer made of areolar connective tissue and simple squamous epithelium (a.k.a. -

S41467-019-14258-Z.Pdf
ARTICLE https://doi.org/10.1038/s41467-019-14258-z OPEN Erythroid differentiation regulator-1 induced by microbiota in early life drives intestinal stem cell proliferation and regeneration Hirohito Abo1, Benoit Chassaing 1,2,3,4, Akihito Harusato 1, Miguel Quiros5, Jennifer C. Brazil5, Vu L. Ngo1, Emilie Viennois6, Didier Merlin6,7, Andrew T. Gewirtz1, Asma Nusrat5 & Timothy L. Denning1* 1234567890():,; Gut microbiota and their metabolites are instrumental in regulating intestinal homeostasis. However, early-life microbiota associated influences on intestinal development remain incompletely understood. Here we demonstrate that co-housing of germ-free (GF) mice with specific-pathogen free (SPF) mice at weaning (exGF) results in altered intestinal gene expression. Our results reveal that one highly differentially expressed gene, erythroid dif- ferentiation regulator-1 (Erdr1), is induced during development in SPF but not GF or exGF mice and localizes to Lgr5+ stem cells and transit amplifying (TA) cells. Erdr1 functions to induce Wnt signaling in epithelial cells, increase Lgr5+ stem cell expansion, and promote intestinal organoid growth. Additionally, Erdr1 accelerates scratch-wound closure in vitro, increases Lgr5+ intestinal stem cell regeneration following radiation-induced injury in vivo, and enhances recovery from dextran sodium sulfate (DSS)-induced colonic damage. Col- lectively, our findings indicate that early-life microbiota controls Erdr1-mediated intestinal epithelial proliferation and regeneration in response to mucosal damage. 1 Center for Inflammation, Immunity & Infection, Institute for Biomedical Sciences, Georgia State University, 100 Piedmont Ave, Atlanta, GA 30303, USA. 2 Neuroscience Institute and Institute for Biomedical Sciences, Georgia State University, Atlanta, Georgia, USA. 3 INSERM, U1016, Paris, France. 4 Université de Paris, Paris, France. -
Neural and Neuroendocrine Control of Digestion: Regulation of Gastrointestinal Hormone Secretion
Neural and Neuroendocrine Control of Digestion: Regulation of Gastrointestinal Hormone Secretion (Chapter 15 in “Eckert Animal Physiology) (Chapter 4 in Hill, Wise & Anderson: “Animal Physiology”) (Chapter 10 in Hadley: “Endocrinology”) General Concepts Covered: — neural and neuroendocrine integration of a complex physiological process — co-ordination of endocrine and exocrine secretion — exocrine secretion affecting endocrine status — endocrine influences on neural, muscle and secretory functions — paracrine and autocrine effects — local influences — positive and negative “feed-back” actions — enzymatic cascades — integration of carbohydrate, fat and protein digestion and appetite control General Introduction — digestion requires co-ordination of movement of food particles, mechanical and chemical digestion of food — opening and closing of sphincter muscles to contain food particles in certain gut compartments for appropriate processing, also control passage through compartments — proper sequential enzymatic processing General Introduction (cont.) — peristaltic action to move food through gut — kneading movement to mix food particles with enzymes and to expose new surfaces for digestion, as well as for absorption From Eckert Secretin - first proposed hormone — 1902, WM Baylist and EH Starling (observations in dogs) — addition of food or acid in stomach is usually followed by pancreatic enzyme secretion into intestine — dennervate and tie off duodenum from stomach, then 1) add acid to stomach - no pancreatic enzyme secretion 2) add acid to -

Pancreatic Amylase
1. Functional Anatomy • The pancreas which lies parallel to and beneath the stomach is composed of: 1. The endocrine islets of Langerhans which secrete: Hormone Type of cell % of secretion Insulin Beta cells 60% crucial for normal regulation of glucose, Glucagon Alpha cells ~25% lipid & protein metabolism Somatostatin delta cells ~10% 1. Acinar gland tissues which produce pancreatic juice (the main source of digestive enzymes). • The pancreatic digestive enzymes are secreted by pancreatic acini. • Large volumes of sodium Bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini. • Pancreatic juice is secreted in Response to the presence of Chyme in the upper portions of the small intestine. 2. Major Components of Pancreatic Secretion and Their Physiologic Roles & 5. Activation of Pancreatic Enzymes • The major functions of pancreatic secretion: 1. To neutralize the acids in the duodenal chyme to optimum range (pH= 7.0-8.0) for activity of pancreatic enzymes. 2. To prevent damage to duodenal mucosa by acid & pepsin. 3. To produce enzymes involved in the digestion of dietary carbohydrate, fat, and protein. Pancreatic Enzymes: The pancreas secrests enzymes that act on all major types of food stuffs. 1. Pancreatic Proteolytic Enzymes (Trypsin, Chymotrypsin, Carboxypolypeptidase, Elastase) • Trypsin & Chymotrypsin split whole and partially digested proteins into peptides of various sizes but do not cause release of individual amino acids. • Carboxypolypeptidase splits some peptides into individual amino acids, thus completing digestion of some proteins to amino acids. • When first synthesized in the pancreatic cells, digestive enzymes are in the inactive forms; these enzymes become activated only after they are secreted into the intestinal tract. -

Secretin Stimulates the Secretion of Bile from the Liver. It Also Increases Watery Bicarbonate Solution from Pancreatic Duct Epithelium
Name Secretin acetate Cat # PP-1670 Size 1 g, 10 g, 100, g and bulk custom packages CAS# 17034-35-4 Mol. Mass 3055.47 Formula C130H220N44O41 Sequence H-His-Ser-Asp-Gly-Thr-Phe-Thr-Ser-Glu-Leu-Ser-Arg-Leu-Arg-Asp-Ser- Ala-Arg-Leu-Gln-Arg-Leu-Leu-Gln-Gly-Leu-Val-NH2 Purity >95% Secretin is a peptide hormone produced in the S cells of the duodenum in the crypts of Lieberkühn. Its primary effect is to regulate the pH of the duodenal contents via the control of gastric acid secretion and buffering with bicarbonate. Secretin stimulates the secretion of bile from the liver. It also increases watery bicarbonate solution from pancreatic duct epithelium. Pancreatic acinar cells have secretin receptors in their plasma membrane. As secretin binds to these receptors, it stimulates adenylate cyclase activity and converts ATP to cyclic AMP.[12] Cyclic AMP acts as second messenger in intracellular signal transduction and leads to increase in release of watery carbonate.It is known to promote the normal growth and maintenance of the pancreas. Secretin increases water and bicarbonate secretion from duodenal Brunner's glands in order to buffer the incoming protons of the acidic chyme.[13] It also enhances the effects of cholecystokinin to induce the secretion of digestive enzymes and bile from pancreas and gallbladder, respectively. It counteracts blood glucose concentration spikes by triggering increased insulin release from pancreas, following oral glucose intake.<[14] It also reduces acid secretion from the stomach by inhibiting gastrin release from G cells.[citation needed] This helps neutralize the pH of the digestive products entering the duodenum from the stomach, as digestive enzymes from the pancreas (eg, pancreatic amylase and pancreatic lipase) function optimally at neutral pH.[citation needed] In addition, secretin simulates pepsin secretion which can help break down proteins in food digestion. -
Cellular Localization of Gastric Inhibitory Polypeptide in the Duodenum and Jejunum
Gut: first published as 10.1136/gut.14.4.284 on 1 April 1973. Downloaded from Gut, 1973, 14, 284-288 Cellular localization of gastric inhibitory polypeptide in the duodenum and jejunum JULIA M. POLAK, S. R. BLOOM', MARION KUZIO, J. C. BROWN, AND A. G. E. PEARSE From the Department ofHistochemistry, Royal Postgraduate Medical School, Hammersmith Hospital, London, and the Department ofPhysiology, University ofBritish Columbia, Vancouver, Canada SUMMARY Indirect immunofluorescence studies using an antiserum to purified porcine gastric inhibitory polypeptide indicate, in the gastrointestinal tract of dog and man, that this polypeptide is present in cells situated predominantly in the mid-zone of the glands in the duodenum and, to a lesser extent, in the jejunum. Absolute correlation of the gastric inhibitory polypeptide cell with one or other of the known endocrine-like cells identified by electron microscopy awaits confirmation by electron immunocytochemistry. It is here identified as an endocrine polypeptide cell of the APUD series and, provisionally, as the D, cell. While the hormonal status of a given polypeptide depends ultimately on physiological experiments the present results strengthen the view that gastric inhibitory polypeptide is indeed a hormone. In 1969 Brown, Pederson, Jorpes, and Mutt described We report here the results of immunofluorescence an enterogastrone, extractable from porcine intestine, studies on the localization of GIP in human and http://gut.bmj.com/ which strongly inhibited gastric acid secretion. The canine intestine. purification of an apparently similar enterogastrone was reported in the same year by Lucien, Itoh, Sun, Material and Methods Meyer, Carlton, and Schally. The first of these poly- peptides, named gastric inhibitory polypeptide Operative samples of duodenal and jejunal mucosa (GIP) by Brown, Mutt, and Pederson (1970), was from seven human subjects were studied. -

Stomach, Duodenum, and Jejunum
Gut, 1970, 11, 649-658 The endocrine polypeptide cells of the human Gut: first published as 10.1136/gut.11.8.649 on 1 August 1970. Downloaded from stomach, duodenum, and jejunum A. G. E. PEARSE, I. COULLING, B. WEAVERS, AND S. FRIESEN' From the Department of Histochemistry, Royal Postgraduate Medical School, London SUMMARY Thirty specimens of stomach, duodenum, and jejunum, removed at operation, were examined by optical microscopical, cytochemical, and electron microscopical techniques. The overall distribution of four types of endocrine polypeptide cell in the stomach, and three in the intestine, was determined. The seven cell types are described by names and letters belonging to a scheme for nomenclature agreed upon at the 1969 Wiesbaden conference o* gastrointestinal hormones. The gastrin-secreting G cell was the only cell for which firm identification with a known hormone was possible. Although there was wide variation in the distribution of the various cells, from one case to another, striking differences were never- theless observable, with respect to the G cell, between antra from carcinoma and from ulcer cases. http://gut.bmj.com/ This study was undertaken with a view to estab- tive shorthand terminology. Correlation with the lishing the overall topographical distribution of terminology used by Solcia, Vassallo, and Capella the various types of endocrine polypeptide cells (1969b) and by Vassallo, Solcia, and Capella in the human stomach and upper intestine. (1969) had to be equated, if possible, with the Adequate sampling was regarded as a pre- scheme used by Forssmann, Orci, Pictet, Renold, on September 28, 2021 by guest. Protected copyright. -

19780525 Gr Im.Pdf
0 0 0 2 TABLE OF CONTENTS I INTRODUCTION II HISTORICAL BACKGROUND III ORIGIN AND NATURE OF GI HORMONES: NEUROENDOCRINE SECRETION AND RELEASE OF PEPTIDES IV ANATOMIC AND CELLULAR DISTRIBUTION OF GI HORMONES V CHEMICAL AND BIOLOGICAL FEATURES OF GI HORMONES: STRUCTURE AS A GUIDE TO BIOLOGICAL ACTION VI GI HORMONES IN PHYSIOLOGY 1. Secretin 7. Pancreatic Polypeptide 2 .. Gastrin 8. Vasoactive Intestinal Polypeptide 3. Cholecystokinin-Pancreozymin 9. Somatostatin 4. Gastric Inhibitory Polypeptide 1o. Substance P 5. Motilin 11. Bombesin 6. Glucagon, Enteroglucagon 12. Other Peptides VII GI HORMONES IN DISEASE A. GI Hormone-Secreting Tumors: Gastrinoma (Zollinger-Ellison Syndrome), and other causes of Hypergastrinemia; MEA Syndromes; VIP-oma (Watery Diarrhea, WDHH or Werner-Morrison Syndrome); Glucagonoma; Somatostatinoma; Pancreatic Polypeptide in Tumors; Substance P (Carcinoid). B. GI Hormones in Other Pathologic States. C. Diagnostic & Therapeutic Uses. VIII CONCLUSION 3 GLOSSARY ACTH - Corticotropin (adrenocorticotropic hormone) AMP - Adenosine monophosphate APUD - Amine precursor uptake and decarboxylation CCK, CCK- PZ - Cholecystokinin-pancreozymin EC - Enterochromaffin EG - Enteroglucagon GI - Gastrointestinal GIP - Gastric-inhibitory polypeptide LES - Lower esophageal sphincter MEA - Multiple endocrine adenomatosis MSH - Melanocyte-stimulating hormone (melanotropin) PP - Pancreatic polypeptide PZ - Pancreozymin RIA - Radioimmunoassay SP - Substance P STM - Standard test meal VIP - Vasoactive intestinal polypeptide WDHH (or WDHA) - Watery -

Pancreas and Fat/Lipid Digestion
Exocrine Pancreas Physiology Pancreatic Anatomy Pancreatic secretion Pancreatic enzymes Daniel S. Kamin MD Boston Children’s Hospital [email protected] Content Reviewers: Sohail Z. Husain, MD Veronique Morinville MD, FRCP(C) NASPGHAN Physiology Education Series Series Editors: Christine Waasdorp Hurtado, MD, MSCS, FAAP [email protected] Daniel Kamin, MD [email protected] Learning Objectives • Understand the normal development and anatomy of the pancreas • Understand the stimuli and cellular factors giving rise to pancreatic secretion • Know the mechanisms by which pancreatic enzymes are activated and remain functional • Be aware of age-related deficiency in exocrine pancreatic function Night blindness • A young man with morbid obesity undergoes roux-en-y gastric bypass. • 1 year later he notices that in the evening he falls down his stairs. • Vitamin A deficiency is diagnosed. Understanding the physiology of pancreatic and bile secretion, Used with permission intraluminal lipolysis, and micellar function explains why this happens! http://www.citelighter.com/science/surgery/knowledgecards/gastric-bypass Pancreas Physiology Overview • Bulk of bicarbonate secretion (more than what secreted in bile and from duodenum) • Enzymes for intra- luminal digestion • Secretin and CCK regulate • Maturational pancreatic insufficiency Used with permission Image from http://www.aboutcancer.com/pancreas1.htm Pancreatic Development • See Embryology and Anatomy of the Gastrointestinal Tract Pancreatic Microanatomy Pancreatic Acinar Secretory Products A • Proteases • Trypsinogen* • Chymotrypsinogen* A • Proelastase* • Procarboxypeptidase* • Procarboxypeptidase B* • Amylolytic enzyme • Amylase A • Lipases • Lipase • B Nonspecific esterase • Prophospholipase A2* • Nucleases • Deoxyribonuclease • Ribonuclease • Others • Pro-colipase* • Trypsin inhibitors A. Exocrine pancreas-- ascinar cells filled • Monitor peptid with secretory granules, cuboidal duct Stored and secreted in inactive form cells secrete bicarbonate-rich fluid B. -

Secretin: Structure of the Precursor and Tissue Distribution of the Mrna (Intestine/Preprohormone/Cdna/Polymerase Chain Reaction) ALAN S
Proc. Nati. Acad. Sci. USA Vol. 87, pp. 2299-2303, March 1990 Biochemistry Secretin: Structure of the precursor and tissue distribution of the mRNA (intestine/preprohormone/cDNA/polymerase chain reaction) ALAN S. KoPIN*, MICHAEL B. WHEELER, AND ANDREW B. LEITER Division of Gastroenterology, Department of Medicine, New England Medical Center, Boston, MA 02111 Communicated by Donald F. Steiner, January 5, 1990 (receivedfor review, November 17, 1989) ABSTRACT Secretin is a 27-amino acid gastrointestinal denum, while the levels reported for hypothalamus, thala- hormone that stimulates the secretion of bicarbonate-rich mus, and olfactory lobe were comparable to those in small pancreatic fluid. The unusually high number ofserine, leucine, intestine (9). Others report that brain contains either small and arginine residues in secretin has precluded the use of amounts (10, 11) or no secretin-like immunoreactivity (12). oligonucleotides to screen cDNA libraries to isolate a secretin In the present study, we have isolated cDNAs encoding the cDNA. In the present study, a short cDNA encoding porcine rat and porcine secretin precursors.t The deduced amino acid secretin was amplified from duodenal mucosal first-strand sequence includes a signal peptide, an N-terminal peptide, cDNA template by using 16,384- and 4096-fold degenerate secretin, and a 72-amino acid C-terminal peptide. We have primers in the DNA polymerase chain reaction. From the used the secretin cDNA as a probe in Northern blot hybrid- sequence of the amplified cDNA, an unambiguous oligonucle- izations to address unresolved questions regarding the tissue otide probe was designed to screen a cDNA library. Here we localization of secretin biosynthesis in the rat CNS and report the sequences of cDNAs encoding the porcine and rat gastrointestinal tract. -

Secretin Cells in Coeliac Disease
Gut: first published as 10.1136/gut.14.11.870 on 1 November 1973. Downloaded from Gut, 1973, 14, 870-874 Secretin cells in coeliac disease JULIA M. POLAK, A. G. E. PEARSE, SUSAN VAN NOORDEN, S. R. BLOOM, AND MARY A. ROSSITER From the Department of Histochemistry, Royal Postgraduate Medical School, London, the Department of Clinical Research, Middlesex Hospital, London, and the Department of Gastroenterology, Queen Elizabeth Hospital, London SUMMARY Immunofluorescence (anti-secretin), cytochemical, and ultrastructural studies were carried out on jejunal biopsies from 16 children with coeliac disease and from 17 controls with suspected malabsorption but normal jejunal morphology. In 11 of the 16 coeliacs there was generalized hyperplasia of endocrine cells and, specifically, of the secretin (S) cells. Further studies, on adult coeliacs as well as on children, combined with serum secretin assays, may establish whether the S cells are abnormally storing hormone because of inability to release it or because of excess production. Present observations suggest that abnormal secretion children with coeliac disease only minimal changes in of certain gut hormones may be involved in the serum insulin were observed during a glucose toler- malfunction of the intestine in coeliac disease. ance test (Grant, 1973). In this disorder the secretory response of the The evidence summarized above points to the http://gut.bmj.com/ exocrine pancreas to a standard meal is reduced conclusion that the pancreas itself is capable of (Worming, Mullertz, Thaysen, and Bang, 1967), as normal function in coeliac disease but that normal it also is after perfusion of the intestine with amino stimulation by secretin and/or CCK/PZ is not acids (which stimulate cholecystokinin secretion).