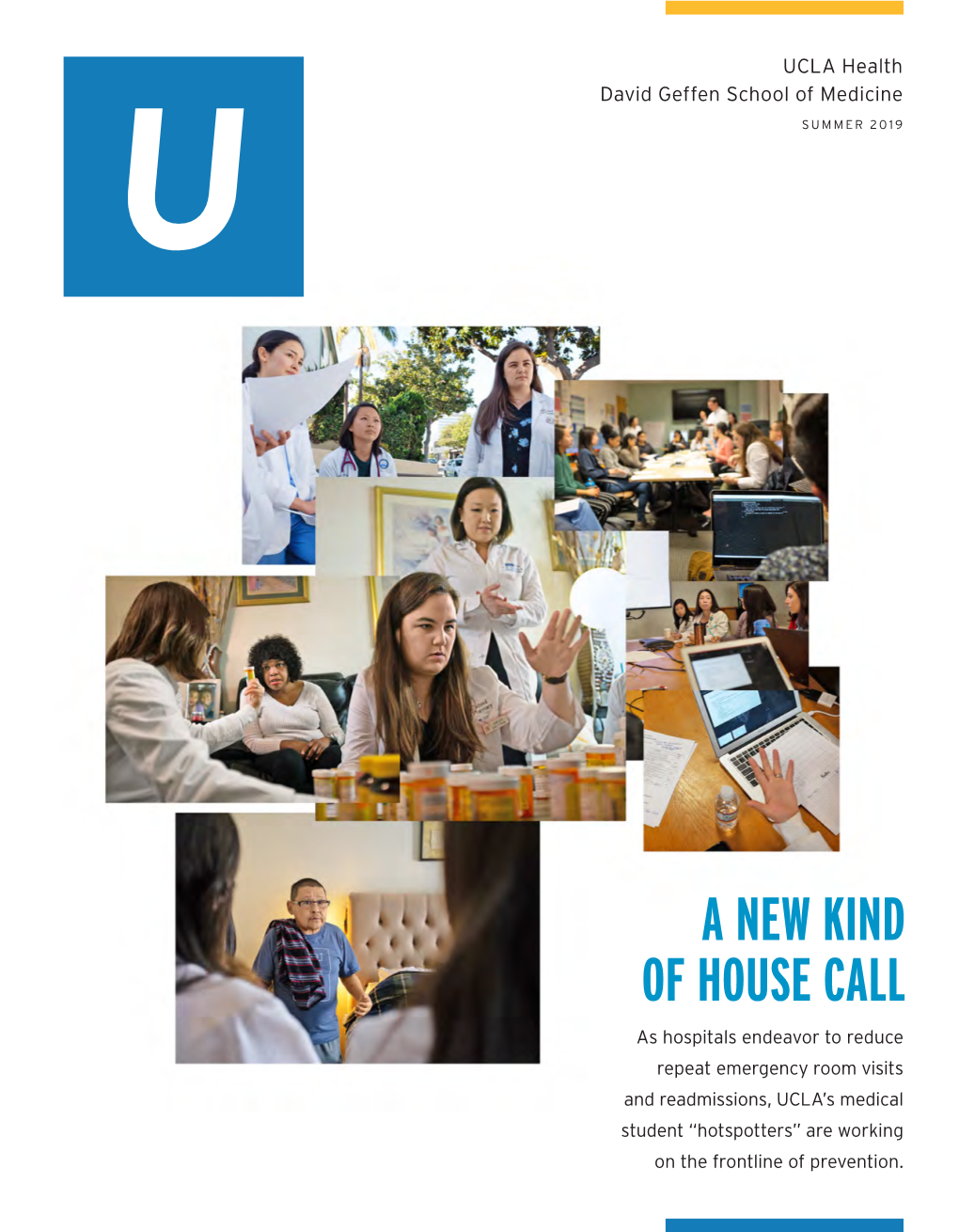
A New Kind of House Call
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UCSF UC San Francisco Previously Published Works
UCSF UC San Francisco Previously Published Works Title "The Way We Were" Ken Warren's Legacy and Modern Investments in Global Health. Permalink https://escholarship.org/uc/item/4m40t0nv Journal The American journal of tropical medicine and hygiene, 97(6) ISSN 0002-9637 Authors Dunavan, Claire Panosian Rosenthal, Philip J Publication Date 2017-12-01 DOI 10.4269/ajtmh.17-0829 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Am. J. Trop. Med. Hyg., 97(6), 2017, pp. 1955–1957 doi:10.4269/ajtmh.17-0829 Copyright © 2017 by The American Society of Tropical Medicine and Hygiene The Tropical Bookshelf “The Way We Were” Ken Warren’s Legacy and Modern Investments in Global Health Dateline 1981. NYU medical student Phil Rosenthal had other overseas sites—mirrored this hope. After leaving recently done clinical work in Kenya and would soon go to Cleveland, Warren was also uniquely positioned to attract India, both overseas rotations spurring his interest in tropical fresh talent to the “new” tropical medicine. After creating the medicine and malaria. Rockefeller-funded “Great Neglected Diseases” (GND) net- Claire Panosian was a newbie Leishmania researcher at work, for example, he also launched the yearly “Biology of Tufts. That its Division of Geographic Medicine existed at all Parasitism” course which continues to this day at the Marine was thanks to Ken Warren, a man who, four years earlier, had Biological Laboratory in Woods Hole, Massachusetts. arrived at the Rockefeller Foundation with a bold, new vision. In 1979, a seminal paper in the New England Journal of In 1981, Warren gave the 46th Charles Franklin Craig Lec- Medicine marked Warren’s brave foray into the high-stakes ture at the ASTMH meeting in Atlanta. -

2017 Report to the Community
HERE AND Report to the Community | 2017 NOW LEADERSHIP CONTENTS MESSAGE Leadership Message 1 crucial neighborhood caregivers. When added Patient Care 2 to our longstanding partnerships with local schools, homeless shelters and other community Research 16 organizations, we are doing more than ever to It all began with the spark of an idea. In aid all those who need quality healthcare. Community 1902, a growing Los Angeles community was Outreach 30 struggling to get quality healthcare, so a group Meanwhile, locally and throughout the nation, of civic leaders came together to create the consumers, payers and employers are asking for Education 38 the forerunner of Cedars-Sinai, the 12-bed better coordination of care to help people get Kaspare Cohn Hospital in the Angelino Heights and stay healthy, ensure that patients always The Campaign neighborhood east of downtown Los Angeles. get the right amount of care and help keep for Cedars-Sinai 44 healthcare affordable for all. You will see many Much has changed in medicine and healthcare examples in this report of how Cedars-Sinai is The Numbers 52 over the past 115 years, yet Cedars-Sinai is still pioneering new ways to provide healthcare that driven every day by the same fundamental is not only of the highest quality, but also has Where We Are 54 question: “What does the community need?” the value and efficiency that the public wants. Leadership 2016 56 One of our top priorities today is to respond Throughout these pages, you also will see to the demand for more accessible, convenient how our pioneering biomedical research and healthcare. -

The Tropical Bookshelf Uncomfortable Truths About Modern Epidemics: a Review of the Pandemic Century and Interview with Author Mark Honigsbaum
Am. J. Trop. Med. Hyg., 101(3), 2019, pp. 724–725 doi:10.4269/ajtmh.19-0388 Copyright © 2019 by The American Society of Tropical Medicine and Hygiene The Tropical Bookshelf Uncomfortable Truths about Modern Epidemics: A Review of The Pandemic Century and Interview with Author Mark Honigsbaum In December 2017, then-ASTMH President Regina Rabinovich life—think roads and transportation; urbanization and calmly read the tea leaves for the coming year. Her first crowding; healthcare facilities; religious and ethnic tensions; observation—“There will be epidemics...”— became a tag-line media; climate change, and the list goes on—have helped to for our 2018 meeting. In the meantime, Gina’s unblinking forecast fuel modern pandemics. made me wonder just a little harder about the next blight to strike. Of course, if we’re going to think big about social determi- And the next. The exercise was both useful and disturbing, be- nants of pandemics, why not think really big? One of the uber- cause it forced me to ponder not only microbes but modern life. morals of The Fever Trail is how people and organizations Reading Mark Honigsbaum’s latest book, one learns that often seek selfish gain over collective good. Remember looking back at epidemics can be equally useful and disturb- Charles Markham, the third man in pursuit of the life-giving tree ing. In The Pandemic Century: One Hundred Years of Panic, with the cinnamon bark and crimson-lined leaves? His vision Hysteria, and Hubris (W.W. Norton, 2019), the journalist and (shared by Florence Nightingale, no less) was to right the author-turned-infectious diseases historian not only revisits wrongs inflicted on Britain’s colonial subjects by providing important global outbreaks but interrogates their social and them with better sanitation and low-cost malaria treatment. -

Annual Report for Generations to Come 2009
Non-Profit Org. The Huntington US Postage Library, Art Collections, and Botanical Gardens PAID Pasadena, CA 1151 Oxford Road • San Marino, California 91108 Permit No. 949 annual report For Generations to Come 2009 www.huntington.org THE HUNTINGTON LIBRARY, ART COLLECTIONS, AND BOTANI CAL GARDENS 2009 ANNUAL REPORT For Generations to Come July 1, 2008—June 30, 2009 BOARD OF TRUSTEES 2008–09 TRUSTEES TRUSTEES EMERITI Stewart R. Smith, Chair Robert F. Erburu, Chair Peter K. Barker MaryLou Boone Paul G. Haaga Jr. Philip M. Hawley Anne F. Rothenberg Peter W. Mullin Geneva H. Thornton Nancy B. Munger Ruth B. Shannon Lawrence R. Tollenaere Robert E. Wycoff BOARD OF OVERSEERS 2008–09 Kenneth S. McCormick, Chair Barry H. Herlihy Robert S. Warren Russel I. Kully, Vice Chair Claudia Huntington Sally K. Wenzlau Ashwin Adarkar Sally Hurt J. Patrick Whaley David Alexander Maurice H. Katz Alyce de Roulet Williamson Gwen Babcock Peter D. Kaufman Norman B. Williamson Merle H. Banta Jennie Kiang E. Eugene Yeager Olin Barrett John R. Light Kwang-I Yu Andrew F. Barth Francis D. Logan Helen L. Bing James B. Lovelace OVERSEERS EMERITI John E. Bryson Mona Mapel Edward M. Carson, Chair Joan Caillouette Lary J. Mielke Norman Barker Jr. Susan Chandler George E. Moss Dorrie Braun Milton Chang Wendy Munger Frances L. Brody Bruce Coffey Harlyne Norris Nancy B. Call Don R. Conlan Kay S. Onderdonk Anne L. Crotty Lloyd E. Cotsen Gregory A. Pieschala Eunice E. Goodan (as of Dec. 1, 2008) Joseph H. Coulombe Lynn P. Reitnouer Boyd Hight Judith Danner Margaret C. Richards Louise Jones Kelvin L. -

Tackling Malaria
Tackling Mal aria Interventions available today could lead to decisive gains in prevention and treatment—if only the world would apply them By Claire Panosian Dunavan Long ago in the Gambia, West Africa, a two-year-old boy named Ebrahim almost died of malaria. Decades later Dr. Ebrahim Samba is still reminded of the fact when he looks in a mirror. That is because his mother—who had already buried several children by the time he got sick—scored his face in a last-ditch effort to save his life. The boy not only survived but eventually became one of the most well-known leaders in Africa: Regional Director of the World Health Organization. Needless to say, scarification is not what rescued Ebrahim Samba. The question is, What did? Was it the particular strain of parasite in his blood that day, his individual genetic or immunological makeup, his nutritional state? After centuries of fighting ma- laria—and conquering it in much of the world—it is amazing what we still do not know about the ancient scourge, including what determines life and death in severely ill chil- dren in its clutches. Despite such lingering questions, however, today we stand on the threshold of hope. Investigators are studying malaria survivors and tracking many other leads in efforts to develop vaccines. Most important, proven weapons—princi- pally, insecticide-treated bed nets, other antimosquito strategies, and new combination drugs featuring an ancient Chinese herb—are moving to the front lines. In the coming years the world will need all the malaria weapons it can muster. -

VENICE FAMILY CLINIC: Improving Capacity and Managing Patient Lead Times
CASE STUDY, 4/2012 VENICE FAMILY CLINIC: Improving capacity and managing patient lead times PREPARED BY Professor Kumar Rajaram, UCLA Anderson School of Management Karen Conner, MD, UCLA David Geffen School of Medicine A case by the Johnson & Johnson/UCLA Health Care Executive Program and the UCLA Anderson School of Management Dr. Susan Fleishman, Medical Director at the Venice Family Clinic (VFC) returned to the clinic after her early morning meeting with CEO, Elizabeth Forer. It was a typically warm and sunny Southern California day as she approached the front door of the clinic. She walked past a line of six to eight people waiting to check in at security and then proceeded upstairs to the waiting room. Almost every seat was taken. The room was full of elderly people, homeless men and women, young mothers, babies, toddlers with runny noses, school-aged children watching TV and adult men and women dressed for work. Some clutched papers indicating they had been seen by either registration or a provider, but most were holding only their color-coded cards given to them as they passed through security. As she headed towards the patient rooms, she noticed two resident doctors holding charts and chatting about their upcoming ski trips, one attending physician talking to a medical assistant about lab work and another on the telephone impatiently waiting on hold. A quick walk by the patient rooms showed that despite the crowd in the waiting room, only about half of the rooms had patients in them. She knew that many of the patients seen by the clinic spent hours there each visit, and that most of that time was spent waiting. -

Venice Family Clinic 2012 Audit Report
VENICE FAMILY CLINIC (A NONPROFIT ORGANIZATION) CONSOLIDATED FINANCIAL STATEMENTS FOR THE YEAR ENDED JUNE 30, 2012 AND SUPPLEMENTAL SCHEDULES REQUIRED BY OMB CIRCULAR A-133 AND THE STATE OF CALIFORNIA DEPARTMENT OF EDUCATION FOR THE YEAR ENDED JUNE 30, 2012 VENICE FAMILY CLINIC (A NONPROFIT ORGANIZATION) CONTENTS June 30, 2012 Page INDEPENDENT AUDITOR’S REPORT 1 -- 2 FINANCIAL STATEMENTS Consolidated Statement of Financial Position 3 Consolidated Statement of Activities 4 Consolidated Statement of Functional Expenses 5 Consolidated Statement of Cash Flows 6 Notes to the Consolidated Financial Statements 7 – 32 SUPPLEMENTAL INFORMATION – CONSOLIDATING SCHEDULES Consolidating Statement of Financial Position by Entity 33 Consolidating Statement of Activities by Entity 34 SUPPLEMENTAL INFORMATION – OMB CIRCULAR A-133 Independent Auditor’s Report on Internal Control over Financial Reporting and on Compliance and Other Matters Based on an Audit of Financial Statements Performed in Accordance with Government Auditing Standards 35 – 36 Independent Auditor’s Report on Compliance with Requirements That Could Have a Direct and Material Effect on Each Major Program and Internal Control Over Compliance in Accordance with OMB Circular A-133 37 – 38 Schedule of Expenditures of Federal and State Awards 39 – 40 Notes to Schedule of Expenditures of Federal and State Awards 41 Schedule of Findings and Questioned Costs 42 – 43 Schedule of Prior Year Audit Findings 44 VENICE FAMILY CLINIC (A NONPROFIT ORGANIZATION) CONTENTS June 30, 2012 Page SUPPLEMENTAL -

WHO Funding Letter
April 24, 2020 President Donald Trump The White House 1600 Pennsylvania Avenue NW Washington, D.C. 20500 Dear President Trump: During this unprecedented global crisis, it is imperative for the U.S. to demonstrate leadership by working with the global community not only to stop the spread of COVID-19, but also to help strengthen the global public health architecture to mitigate a crisis of this magnitude from happening again. Therefore, we, the undersigned organizations, urge the U.S. Administration to continue to fund the World Health Organization (WHO) to end this pandemic. The United States cannot rid this insidious virus from the country, nor around the world, without WHO. WHO is the only organization with the technical capacity and global mandate to support the public health response of all countries during this critical time. China first alerted WHO to the possibility of a novel type of coronavirus on December 31, 2019. WHO worked closely with U.S. public health institutions like the U.S. Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH), as well as the global community, to collect, analyze, and disseminate public health information about COVID-19. These actions equipped countries with advance warning and guided states’ efforts to prepare for the spread of the virus. Just one day after receiving the alert from China, WHO alerted the CDC and by January 10, WHO issued guidance to countries on how to detect, test, and manage potential cases of the novel virus, and best practices to protect health workers delivering care on the frontlines of the response. -

Awakening to Global Health
Narrative Matters Awakening To Global Health It’sbeenlonelyinthetropicalmedicinetrenches,butmoreandmoreAmericans are discussing and growing passionate about the need to improve global health. by Claire Panosian Dunavan ot long ago, the personal assistant to PREFACE: What we used to call “in- an actress left me a voicemail message. In ternational health” (suggesting some- the past, I had provided travel care—vac- thingthatwenton“overthere”)hasnow N cines and malaria pills, treatments for pesky been renamed and reenergized as “global rashes and other overseas ills—to the actress, her health.” Travel, communications, and husband, and members of their entourage. Two the resurgent power of microorganisms or three years had passed since our last visit, but, make the health of populations in Asia of course, I remembered the glamorous crew. The or Africa mainline concerns in the aging celebrity—still beautiful. The business- United States. Both epidemiology and tycoon husband who adored and indulged her. humanitarianism argue for a global And, last but not least, the butler, secretaries, and view of world health. In her essay, tropi- other helpers who kept the couple’s lives running cal medicine specialist Claire Panosian in true, Hollywood-fairytale style. Dunavan discusses the path that led the As an occasional doctor to the household, I United States to this new level of aware- even knew bits and pieces of its Upstairs, Down- ness about the importance of world stairs dramas. Some staff members—for various health and the realization that, as she reasons—didn’t last. But something in this assis- puts it, “the health of others touches all of tant’svoicetoldmethatshewasaseasonedpro. -

AAMS' 13Th Annual CME & CDE Las Vegas Getaway
AAMS' 13th Annual CME & CDE Las Vegas Getaway The Armenian American Medical Society has organized a full day of educational and networking opportunities to take place at the beautiful Caesars Palace in Las Vegas. Attendees will be eligible to receive a maximum of (10) AMA PRA Category 1 CME Credit(s) and (6) CDE Credit(s). Below is another example of one of the exceptional talks we have lined up for you: Claire Panosian Dunavan, MD, DTM&H, FIDSA is a professor of medicine and infectious diseases at UCLA School of Medicine who attended Stanford University, Northwestern University Medical School, and the London School of Hygiene and Tropical Medicine. She completed her residency in internal medicine at Northwestern and her fellowship in infectious diseases and geographic medicine at Tufts- New England Medical Center. Dr. Dunavan is a well-known expert in infectious diseases, tropical medicine, and global health policy, having worked both as a senior consultant for the Board on Global Health at the National Academies of Science and a visiting professor in many countries. In 2008, she served as President of the American Society of Tropical Medicine and Hygiene. Claire Panosian Dunavan's second career in medical journalism includes 6 years as a medical editor, reporter, and co-anchor for Lifetime Television. In recent years, she has written for Scientific American, Discover magazine, and the Los Angeles Times. Her work has also been published in the New York Times, Washington Post, International Herald Tribune, Baltimore Sun, and Chicago Tribune as well as the New England Journal of Medicine, Nature, JAMA and Health Affairs. -

COVID-19 CHRONICLES Stories from the Frontline of the Pandemic
UCLA Health David Geffen School of Medicine FALL 2020 COVID-19 CHRONICLES Stories from the frontline of the pandemic. Departments Features A publication of UCLA Health and David Geffen School of Medicine at UCLA VICE CHANCELLOR, UCLA HEALTH SCIENCES CEO, UCLA HEALTH John C. Mazziotta, MD (RES ’81, FEL ’83), PhD Photo: Courtesy of Dr. Judith S. Currier PRESIDENT, UCLA HEALTH CEO, UCLA HOSPITAL SYSTEM 02 ASSOCIATE VICE CHANCELLOR, UCLA HEALTH SCIENCES Johnese Spisso, MPA Perspective Research is the path out of the COVID-19 pandemic. DEAN, DAVID GEFFEN SCHOOL OF MEDICINE AT UCLA BY JUDITH S. CURRIER, MD Kelsey C. Martin, MD, PhD CHIEF OF COMMUNICATIONS Rhonda L. Curry 04 Illustration: Davide Bonazzi CHIEF OF MARKETING Reflection 20 Tanya E. Andreadis It is time for creative compassion. BY THANH H. NEVILLE, MD ’05 (RES ’08, FEL ’11), MSHS EDITOR Command and Control How UCLA Health confronted the COVID-19 pandemic. David Greenwald BY DAN GORDON DESIGN & ART DIRECTION 06 Donenfeld & Associates The Cutting Edge CONTRIBUTING WRITERS Patients with cancer communicate heart-to-heart. Judith S. Currier, MD Veronique de Turenne Marrecca Fiore David Geffner 14 Dan Gordon Julie Kirst Conversation Thanh H. Neville, MD ’05 (RES ’08, FEL ’11), MSHS What the COVID-19 pandemic will mean for medical education. Claire Panosian Dunavan, MD Katherine A. Van Story Natasha B. Wheaton, MD 18 EDITORIAL ADVISORY CO-CHAIRS Spotlight Clarence H. Braddock III, MD Dr. Gay M. Crooks answers a few questions. Patrick T. Dowling, MD EDITORIAL ADVISORY COMMITTEE Benjamin J. Ansell, MD ’92 (RES ’95) Sherin U. Devaskar, MD Steven M. -

8 Tpm096-3S Former Presidents.Indd
MEMBERSHIP DIRECTORY 137 FORMER PRESIDENTS OF THE PARENT SOCIETIES The National Malaria Society *W.H.W. Kemp ............................................1951–1952 *Mark F. Boyd .............................................1945–1946 *Justin M. Andrews .................................... 1950–1951 *H. A. Johnson ............................................ 1944–1945 *Paul F. Russell ...........................................1949–1950 *George H. Bradley ..................................... 1943–1944 *Wendell Gingrich .......................................1948–1949 *James S. Simmons ...................................1942–1943 *E. Harold Hinman ......................................1947–1948 *John H. O’Neill ..........................................1941–1942 *Mark D. Hollis ............................................1946–1947 The American Society of Tropical Medicine *William A. Sodeman ..................................1951–1952 *Kenneth M. Lynch .....................................1929–1930 *Paul F. Russell ...........................................1950–1951 *William E. Deeks ....................................... 1928–1929 *Hamilton H. Anderson ...............................1949–1950 *Charles C. Butler .......................................1927–1928 *Norman H. Topping ...................................1948–1949 *Joseph E. Siler ..........................................1925–1926 *Joseph S. D’Antoni ................................... 1947–1948 *Samuel T. Darling ......................................1924–1925 *Edward J. Salisbury