Questions from South Molton 26 August
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Al160207osa Market Coastal Towns
EEC/07/63/HQ Environment, Economy and Culture Overview/Scrutiny Committee 5 March 2007 Market and Coastal Towns Report of the Director of Environment, Economy and Culture 1. Summary In January 2006, members received a report on the draft Devon Sites and Premises Strategy and as a result expressed concern about the shortage of premises for smaller businesses. It was resolved that a further report be submitted, which covered economic development issues relating to Market Towns, including the availability of sites for relocation of small businesses and the Market and Coastal Town initiative (MCTi). This report concentrates on work undertaken in association with the MCTi pending further analysis of specific matters relevant to business premises. 2. Background In the South West, the MCTi commenced in 2000 and was led by the Regional Development Agency, Countryside Agency and English Heritage, with support from many other bodies. The scheme received greater emphasis following the incidence of Foot and Mouth Disease and a number of towns adversely affected were included in the programme. Since October 2004, delivery of the initiative has been charged to the Market and Coastal Towns Association (MCTA). This is an independent organisation largely funded by the Regional Development Agency, English Heritage and Big Lottery Fund. The initiative is a community based regeneration programme focusing on the preparation, by local people, of a long term Community Strategic Plan covering the social, economic, environmental and cultural features of their town and its hinterland. The MCTA delivers capacity building support to communities, enabling them to prepare the plans and develop their skills and organisational capacity while sharing good practice with others. -

Northern Devon in the Domesday Book
NORTHERN DEVON IN THE DOMESDAY BOOK INTRODUCTION The existence of the Domesday Book has been a source of national pride since the first antiquarians started to write about it perhaps four hundred years ago. However, it was not really studied until the late nineteenth century when the legal historian, F W Maitland, showed how one could begin to understand English society at around the time of the Norman Conquest through a close reading and analysis of the Domesday Book (Maitland 1897, 1987). The Victoria County Histories from the early part of the twentieth century took on the task of county-wide analysis, although the series as a whole ran out of momentum long before many counties, Devon included, had been covered. Systematic analysis of the data within the Domesday Book was undertaken by H C Darby of University College London and Cambridge University, assisted by a research team during the 1950s and 1960s. Darby(1953), in a classic paper on the methodology of historical geography, suggested that two great fixed dates for English rural history were 1086, with Domesday Book, and circa 1840, when there was one of the first more comprehensive censuses and the detailed listings of land-use and land ownership in the Tithe Survey of 1836-1846. The anniversary of Domesday Book in 1986 saw a further flurry of research into what Domesday Book really was, what it meant at the time and how it was produced. It might be a slight over-statement but in the early-1980s there was a clear consensus about Domesday Book and its purpose but since then questions have been raised and although signs of a new shared understanding can be again be seen, it seems unlikely that Domesday Book will ever again be taken as self-evident. -

VICTORIAN RURAL POLICEMAN Mini Project 2017
VICTORIAN RURAL POLICEMAN Mini Project 2017 Rural Constabularies were established following the Royal Commission which met between 1836 and 1839, the County Police Act of 1839 and the amending Act of 1840. In 1856 the County and Borough Police Act made the establishing of a police force mandatory for all counties and boroughs. All the police men in the mini project are listed as Police Constables in the 1881 census. The purpose of the project is to find out more about these rural policemen – who they were, how they lived and do they fit the quotations. FACHRS Ref: WATC01 Researcher Name: Timothy M Clark Policeman’s Name: STEPHEN CLARK Age in 1881 Census: 41 Source: - RG Number: 11 Piece: 2240 Folio: Page: 14 Reg. District: South Molton Parish: Warkleigh County Devon Migration, Employment and Social Status Information from each census about Stephen Clark and the household he lived in: Born 22 November 1839 at Malborough, South Devon, birth registered at Kingsbridge. Second son of William Steer Clark, mariner, and Sarah nee Jarvis, both Devon born, as were the 3 previous generations. YEAR 1841 1851 1861 1871 1881 1891 1901 1911 CENSUS H107 RG 9 RG 10 RG 11 RG 12 RG 13 PIECE 248 1412 2090 2240 1772 2144 FOLIO 92 23 104 PAGE 1 14 7 1 17 REG DIS 6 Upton South Molton South Molton Newport, St PARISH Malborough Tormoham Paignton Warkleigh Chittlehambolt John ADDRESS Buckley 12 Queen Warkleigh Village 20 Victoria 3 Hobbs Cottages Street Villa Street TOWN Salcombe Newton South Molton South Molton Barnstaple Barnstaple Abbot COUNTY Devon Devon Devon -

DEVONSHIRE. ( KELLY's Handsome Modern Building, Pleasantly Situated
til2 ROBOROTTGH. DEVONSHIRE. ( KELLY'S handsome modern building, pleasantly situated. The 4· ro p.m. Postal orders are issued here. but not paid. lord of the manor and the Hon. Mark George Kerr Rolle Bea.ford is the nearest monev order office & telegraph are ihe chief landowners. The soil is clayey; sub;roil, office, 3 miles disrtant stone. The chief crops are cereal. The area is 3,2I2 Public Elementary School (mixed), built in 1854 & en- acres; rateable value, £2,I70; the population in Igor larged in 1872, for go children; average attendance, was 312. 67; & supported in part by a legacy of £-z..;o bequeathed Post Office.-Edwin Pincombe, sub-postmaster. Letters by Miss Maria Horndon in I858; the managers are arrive at 10 a.m.· from Beaford R.S.O.; dispatched at the rector & churchwardens; Waiter Pritchard, master Batson Thomas J.P. Ebberly ill()use Folland Thomas, farmer, Sugworthy Prouse Robert, farmer, Thelbridge May Rev. Edward Henry l!'ox B.A. Friend ATthur, m'<.lson Heed John, farmer, Parkins Rectory Hoppe-r Jn.butcher & frmr.Ea.Rapson Reed Thomas R. farmer & assi:otant' Isaac William, shoe maker overseer, Parkins COMMERCIAL. Lemon Ann & Mary J. (Misses), Richards Thomas, farmer, Rapson Allin Thomas, fail'mer, Cliston farmers, Villavin Rockey "\Villiam, wheelwright Badcock J ame,s, farmer, Coombe Martin Grace (Mrs.), baker Squire Fras. frmr. Gt. & Lit.Wansley Bealey Eli, farmer, Villavin M.aynard John Bealey, New inn & Squi,re Henry, mason BeaJey Richard, blacksmith farmer Squire John, farmer, Hand fords Bealey John, farmer, N ewcombs Maynard J onathan, shoe maker Squire Thomas,farmer, Gt. -
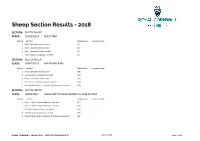
Sheep Section Results - 2018
Sheep Section Results - 2018 SECTION: BELTEX SHEEP CLASS: S0001/0312 AGED RAM Placing Exhibitor Catalogue No. Livestock Name 1 Mrs C L Elworthy, Exeter, Devon (3) 2 Mrs C L Elworthy, Exeter, Devon (4) 3 Miss T Cobbledick, Bude, Cornwall (2) 7 L & V Gregory, Launceston, Cornwall (5) SECTION: BELTEX SHEEP CLASS: S0001/0313 SHEARLING RAM Placing Exhibitor Catalogue No. Livestock Name 1 Mrs C L Elworthy, Exeter, Devon (10) 2 L & V Gregory, Launceston, Cornwall (12) 3 Mrs C L Elworthy, Exeter, Devon (11) 4 Mr S & Mrs G Renfree, Liskeard, Cornwall (20) 7 Mrs M A Heard & Mr G J Garland, Wiveliscombe, Somerset (15) SECTION: BELTEX SHEEP CLASS: S0001/0314 AGED EWE TO HAVE REARED A LAMB IN 2018 Placing Exhibitor Catalogue No. Livestock Name 1 Miss A H & Mrs S Payne, Newquay, Cornwall (27) 2 Miss A H & Mrs S Payne, Newquay, Cornwall (28) 3 Miss J M Lapthorne, Plymouth, Devon (26) 4 L & V Gregory, Launceston, Cornwall (23) 7 Mrs M A Heard & Mr G J Garland, Wiveliscombe, Somerset (24) ROYAL CORNWALL SHOW 2018 - SHEEP SECTION RESULTS 08 June 2018 Page 1 of 63 SECTION: BELTEX SHEEP CLASS: S0001/0315 SHEARLING EWE Placing Exhibitor Catalogue No. Livestock Name 1 Mr H Williams, Llangadog, Carmarthenshire (49) 2 Mrs M A Heard & Mr G J Garland, Wiveliscombe, Somerset (38) 3 Mr S & Mrs G Renfree, Liskeard, Cornwall (47) 4 Mrs C L Elworthy, Exeter, Devon (34) 5 L & V Gregory, Launceston, Cornwall (36) 6 Mr S & Mrs G Renfree, Liskeard, Cornwall (48) 7 Mr H Williams, Llangadog, Carmarthenshire (50) SECTION: BELTEX SHEEP CLASS: S0001/0316 RAM LAMB Placing Exhibitor Catalogue No. -

Fixtures and Results
Fixtures and Results Matches From: Saturday 22 May, 2021 Matches To: Sunday 22 May, 2022 Tribute Devon 1 04/09/2021 Buckfastleigh Ramblers - Totnes Dartmouth - Torrington Exeter Athletic - Tamar Saracens Exeter Saracens - South Molton Ilfracombe - Salcombe New Cross - Plymouth Argaum Old Plymothian & Mannamedian - Old Technicians 11/09/2021 Buckfastleigh Ramblers - Dartmouth Plymouth Argaum - Old Plymothian & Mannamedian Salcombe - New Cross South Molton - Ilfracombe Tamar Saracens - Exeter Saracens Torrington - Exeter Athletic Totnes - Old Technicians 18/09/2021 Dartmouth - Totnes Exeter Athletic - Buckfastleigh Ramblers Exeter Saracens - Torrington Ilfracombe - Tamar Saracens New Cross - South Molton Old Plymothian & Mannamedian - Salcombe Old Technicians - Plymouth Argaum 25/09/2021 Buckfastleigh Ramblers - Exeter Saracens Dartmouth - Exeter Athletic Salcombe - Old Technicians South Molton - Old Plymothian & Mannamedian Tamar Saracens - New Cross Torrington - Ilfracombe Totnes - Plymouth Argaum 02/10/2021 Exeter Athletic - Totnes Exeter Saracens - Dartmouth Ilfracombe - Buckfastleigh Ramblers New Cross - Torrington Old Plymothian & Mannamedian - Tamar Saracens Old Technicians - South Molton Plymouth Argaum - Salcombe 09/10/2021 Buckfastleigh Ramblers - New Cross Dartmouth - Ilfracombe Exeter Athletic - Exeter Saracens South Molton - Plymouth Argaum Tamar Saracens - Old Technicians Page 1 of 5 Fixtures and Results Matches From: Saturday 22 May, 2021 Matches To: Sunday 22 May, 2022 Torrington - Old Plymothian & Mannamedian Totnes - Salcombe -

South Molton Annual Sheep Fair of Breeding Ewes, Ewe Lambs & Rams
SOUTH MOLTON ANNUAL SHEEP FAIR OF 3000 BREEDING EWES, EWE LAMBS & RAMS ENTRIES INCLUDE 2555 BREEDING EWES 205 EWE LAMBS 240 RAMS, VARIOUS BREEDS rd WEDNESDAY 23 AUGUST 2017 Sale to commence at 10am with the Older Ewes Rams to commence at 12 noon approx SOUTH MOLTON LIVESTOCK OFFICE- 01769 572042 *We would like to thank Mr Gerald Arscott for kindly doing the ballot for this year’s sale* CONDITONS OF SALE The bidding is to be regulated by the Auctioneers and no bid shall be retracted. The highest approved bidder is to be the buyer and if any dispute shall arise, the same shall be referred to the Auctioneers, whose decision shall be final. The Vendor reserves the right to bid. The Purchasers are to give their names and places abode and pay the full purchase price for each lot at the fall of the hammer (if required) in default of which the lot or lots purchased shall be immediately put up again and resold. In every case the whole of the purchase money must be paid to the Auctioneers either during the progress or immediately at the close of the Auction. Every care has been taken to ensure the accuracy of this catalogue, but the Vendors or auctioneers shall not be liable for the incorrect description of any lots. WARANTY OF BREEDING EWES All ewes are sold as right in the udder and fit to breed except where otherwise stated. The Vendor shall correctly describe the teeth of each lot of ewes. Where ewes fail to comply with the above warranty, notification must be made to the Auctioneers in writing within five days of the sale, after which no complaint shall be entered. -

Crangs House, East Street, North Molton, South Molton, Devon, EX36 3JQ
Crangs House, East Street, North Molton, South Molton, Devon, EX36 3JQ A spacious and well-presented period house in a popular village South Molton 4 miles Exmoor National Park 1 mile Barnstaple 14 miles • Superbly Presented • Exmoor Foothills • Sitting Room • Dining Room/Snug • Kitchen/Breakfast Room • 5 Bedrooms (2 En- Suite) • Bathroom • Enclosed Rear Gardens • Guide price £295,000 01769 572263 | [email protected] Cornwall | Devon | Somerset | Dorset | London stags.co.uk Crangs House, East Street, North Molton, South Molton, Devon, EX36 3JQ SITUATION ACCOMMODATION Crangs House is situated in the very much sought after Part glazed stable door to the enclosed PORCH with village of North Molton, which offers an excellent range of useful shelving. The SITTING ROOM has dado panelling, local amenities including primary school, public house, window seat, stone and brick fireplace with slate hearth two churches, excellent post office/stores, garage/petrol and mantel over. The DINING ROOM also has a window station and sports club. The village is easily accessible to seat, storage cupboard and shelving. The KITCHEN/ the A361 North Devon link road which provides a direct BREAKFAST ROOM is an attractive room with large route to the regional centre of Barnstaple to the west and fireplace with timber surround and mantel and is fitted Tiverton to the south east and further on to the M5 (J 27) with a range of painted units with slate worktop over and with Tiverton Parkway railway station on the Paddington matching wall units. Electric cooker point with hood over line. The market town of South Molton is four miles and and Belfast sink with mixer tap. -

Devon Community Equipment Recycling Centres
1 List Of Equipment Recycling Points in Devon Area Location Address Phone Number East Sidmouth Hospital All Saints Road 01395 512482 Sidmouth EX10 8EW East Ottery St Mary Hospital Keegan Close 01404 816000 Ottery St Mary EX11 1DN East Seaton Hospital Valley View Road 01297 23901 Seaton EX12 2UU East Axminster Hospital Chard Street 01297 630400 Axminster EX13 5DU East Honiton Hospital Marlpits Lane 01404 540540 Honiton EX14 2DE East Exmouth Hospital Claremont Grove 01395 279684 Exmouth EX8 2JN East Sidmouth Recycling Bowd 0345 155 1010 Centre Sidmouth EX10 0AX East Sutton Barton Recycling Widworthy 0345 155 1010 Centre Honiton EX14 9SP East Knowle Hill Recycling Salterton Rd 0345 155 1010 Centre Exmouth EX8 5BP Exeter Whipton Hospital Hospital Lane 01392 208333 Whipton Exeter EX1 3RB Exeter Royal Devon & Exeter Royal Devon & Exeter 01392 411611 Hospital Hospital, Barrack Road Exeter EX2 5DW Exeter Exton Road Recycling Exton Road 0345 155 1010 Centre Exeter EX2 8LX Exeter Pinbrook Road Pinbrook Road 0345 155 1010 Recycling Centre Exeter EX4 8HU 2 Exeter Millbrook Healthcare Units 5-8 0330 124 4491 Block B Jacks Way Hill Barton Business Park Clyst St Mary Exeter EX5 1FG Mid Tiverton Hospital Kennedy Way 01884 235400 Tiverton EX16 6NT Mid Crediton Hospital Western Road 01363 775588 Crediton EX17 3NH Mid Ashley Recycling Centre Tiverton 0345 155 1010 EX16 5PD Mid Punchbowl Landfill Site Crediton 0345 155 1010 Devon EX17 5BP Mid Refurnish Crediton Mill Street 01363 774577 Crediton EX17 1EY Mid Okehampton Recycling Exeter Road Industrial 0345 -

Discharge from the Macular Clinic
Discharge from the macular clinic Exmoor Unit Tel: 01271 322770 Other formats If you need this information in another format such as audio tape or computer disk, Braille, high contrast, British Sign Language or translated into another language, please telephone the PALS desk on 01271 314090. This leaflet contains information regarding support services and telephone numbers on how to contact the macular clinic following discharge from the North Devon District Hospital macular clinic. Please keep it in a handy safe place. How to contact the Exmoor Unit If you feel your macular eye condition has deteriorated following your discharge, please contact the Exmoor Unit for further advice. Exmoor Unit reception: 01271 322770 Rehabilitation Officers for the Visually Impaired (ROVI) Rehabilitation Officers for the Visually Impaired or ROVIs are part of Devon Adult and Community Services Sensory Impairment Team. There are two ROVIs in the area; John Wade (Torridge) and Clare Aldrich (North Devon). You may have spoken to them already in the macular clinic. They are available every Wednesday and Thursday morning. Leaflet number: 567 / Version number: 2 / Review due date: July 2021 1 of 6 Northern Devon Healthcare NHS Trust ROVIs can offer practical help and information regarding any day- to-day problems you might have, because of your sight loss; managing in the home or kitchen, getting out and about safely or knowing which organisations can offer you the best support. They can also advise you on the benefits of registration as Sight Impaired or Severely Sight Impaired. To contact John Wade or Clare Aldrich, please call Devon County Council on 01392 38300 and ask for them by name. -

Chittlehamholt, Satterleigh & Warkleigh Report 2007
Exmoor House, Dulverton, Somerset, TA22 9HL Telephone: 01398 322245 Fax: 01398 323150 E-mail: [email protected] Website Address: www.exmoor-nationalpark.gov.uk /Projects/RuralHousingProject/RuralHousingProject.htm Chittlehamholt And Satterleigh and Warkleigh Parishes Housing Needs Survey Report August 2007 Rural Housing Project The Rural Housing Project has been running since 2002 and is a partnership between Exmoor National Park Authority; North Devon District Council; West Somerset District Council; Hastoe Housing Association; Falcon Rural Housing; North Devon Homes Ltd; Magna Housing Association and Defra. It has been working hard to address the shortage of affordable housing within a predominantly rural area. The area covered by the project displays an extreme disparity between incomes and house prices which makes it hard for many to gain any secure footing within the housing market. The Rural Housing Project is designed to help promote and deliver affordable rural housing strategically across the project area and helps deliver Exmoor National Park housing policies within the park. This is being achieved by informing people about affordable rural housing, providing help and advice, carrying out research at a parish level to assess the affordable housing need and bringing together the community and various partners to help deliver housing where it is needed. One of the tasks for the project is to work with the Parish Council and the local community to assist them in carrying out a Housing Needs Survey in order to identify -

NORTH DEVON Easter 2018 Pharmacy Opening Times
NORTH DEVON Easter 2018 Pharmacy Opening Times TRADING NAME ADDRESS 1 ADDRESS 2 POSTCODE TELEPHONE Easter Easter Specialist Good Friday Easter Sunday Minor Emergency NUMBER Saturday Monday Medicines (30.3.18) (1.4.18) Ailments Supply (31.3.18) (2.4.18) Bear Street 49 Bear Street Barnstaple EX32 7DB 01271 342549 No Closed 0900-1200 Closed Closed Yes Yes Pharmacy Boots pharmacy Roundswell Shopping Centre, Barnstaple EX31 3NL 01271 328117 No 0900-1730 0900-1730 1400-1600 Closed Yes Yes Gratton Way Boots pharmacy 69-70 High Street Barnstaple EX31 1HX 01271 326772 No 0830-1800 0830-1800 Closed 1030-1630 Yes Yes Boots pharmacy 6 Higher Road, Fremington Barnstaple EX31 3BG 01271 372407 No 0900-1800 0900-1730 Closed Closed Yes Yes Lloydspharmacy 2 Brannams Square, Kiln Barnstaple EX32 8QB 01271 342076 No Closed Closed Closed Closed No No Lane Lloydspharmacy Sainsbury's, Roundswell Barnstaple EX31 3NH 0127 1392506 No 1000-1600 0700-2200 Closed 1000-1600 Yes Yes Shopping Centre, Gratton Lloydspharmacy The Litchdon Medical Centre, Barnstaple EX32 9LL 01271 342434 No Closed Closed Closed Closed Yes Yes Landkey Road Tesco pharmacy Barnstaple Retail Park, Barnstaple EX31 2AS 01172 918822 Yes 0630-2230 0630-2200 Closed 0900-1800 Yes Yes Station Road, Bickington Arnolds Pharmacy 21 Nelson Road, Westward Bideford EX39 1LF 01237 473829 No Closed 0900-1300 Closed 1900-2200 No No Ho! Asda pharmacy Atlantic Village, Clovelly Road Bideford EX39 3QU 01237 427720 Yes 0900-1800 0700-2200 Closed 0900-1800 No No Boots pharmacy 2 High Street Bideford EX39 2AA 01237