NINA SARJA: [ F]Fluoride
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![Arxiv:2001.06745V2 [Nucl-Th] 6 Jun 2021 Osrit Nteeuto Fsaeo Eto-Ihncermat Nuclear [5–9]](https://docslib.b-cdn.net/cover/8390/arxiv-2001-06745v2-nucl-th-6-jun-2021-osrit-nteeuto-fsaeo-eto-ihncermat-nuclear-5-9-118390.webp)
Arxiv:2001.06745V2 [Nucl-Th] 6 Jun 2021 Osrit Nteeuto Fsaeo Eto-Ihncermat Nuclear [5–9]
Neutron drip line of Z =9 − 11 isotopic chains Rong An,1 Guo-Fang Shen,1 Shi-Sheng Zhang,1, ∗ and Li-Sheng Geng1, 2, 3, 4, † 1School of Physics, Beihang University, Beijing 100191, China 2Beijing Key Laboratory of Advanced Nuclear Materials and Physics, Beihang University, Beijing 100191, China 3Beijing Advanced Innovation Center for Big Data-based Precision Medicine, Beihang University, Beijing100191, China 4School of Physics and Microelectronics, Zhengzhou University, Zhengzhou, Henan 450001, China A recent experimental breakthrough identified the last bound neutron-rich nuclei in fluorine and neon isotopes. Based on this finding, we perform a theoretical study of Z = 9, 10, 11, 12 isotopes in the relativistic mean field (RMF) model. The mean field parameters are assumed from the PK1 parameterization, and the pairing correlation is described by the particle number conservation BCS (FBCS) method recently formulated in the RMF model. We show that the FBCS approach plays an essential role in reproducing experimental results of fluorine and neon isotopes. Furthermore, we predict 39Na and 40Mg to be the last bound neutron-rich nuclei in sodium and magnesium isotopes. I. INTRODUCTION Properties of neutron-rich nuclei, in particular, the location of the neutron drip line, play an important role not only in understanding nuclear stability with respect to the isospin in hereto unexplored regions of the nuclear chart [1], but also in numerous related scientific issues of current interests. For instance, the r-process nucleosynthesis of heavy elements in stellar evolution crucially depends on the values of beta decay rates and neutron capture cross sections in neutron-rich nuclei that do not exist in terrestrial conditions [2–4]. -

Fluorine-18 Labelled Compounds
I fluoríne-18 labelled compounds 3 rM. lá i I •'•$ i 3 ;? 7Í5 %• 2! % tekeningen J.R. Eykenduyn, L.F. van Rooij en E. Zeeman I fotografisch werk W.C. van Sijpveld 'i'l r. English proofreader Scott Rollins P typewerk Stance Mulders I ODslagontwerp G.J. Lijnzaad VRIJE UNIVERSITEIT TE AMSTERDAM fluorine-18 labelled compounds ACADEMISCH PROEFSCHRIFT ter verkrijging van de graad van doctor in de wiskunde en natuurwetenschappen aan de Vrije Universiteit te Amsterdam, •I op gezag van de conrector dr. H. Verheul, hoogleraar in de faculteit der wiskunde en natuurwetenschappen, in het openbaar te veYdedigen I op vrijdag 17 maart 1978 te 15.30 uur ¡n het hoofdgebouw der universiteit, De Boelelaan 1105 doos- Jacob Pieter de Kleijn geboren te '»Gravenhage i I 1978 Centrale Reproductie Dienst Vrije Universiteit I ¿rC--''&¿ Promotor : Dr. B.van Zanten Coreferent: Prof.dr. M.G.WoWring Í1 I 1 if I- 5- I I 1 I /nuil^ ti-. s -if I V5| ^!.ia^^^ STELLINGEN I De op papier aantrekkelijke methode van 'general labelling' van organische verbindingen door middel van de reactie met 14CO¿ in aanwezigheid van mag- nesium onder invloed van 7-straling verdient een serieuze experimentele aan- pak. J. P. H. Brown. Int. J. Appl. Rad. Isot. 27. 719 (1976). II Het verdient aanbeveling dat bij dierexperimenten waarbij radiofarmaca wor- den toegediend, de activiteitsaccumulatie in een orgaan wordt beschreven in samenhang met het gewicht van het betreffende orgaan. R.P. Spencer, J.Nucl.Med. 17.1110(1976). Ill De omzetting: benzaldehyde + magnesium -*• benzit -1- magnesiumhydride is slechts waarschijnlijk onder katalyserende reactie-omstandigheden. -

Isotope and Nuclear Chemistry Division Annual Report, FY 1990, October 1, 1989
LA12143-PR Progren Report Isotope dnd Nuclecqr Chemistry Division Ann vial Report FY 1990^ .. •• %-•-' V \ ? L«>Alaa^Natkif^'ljri>oratoryk operated by the UnhrcnUy of Colitbr^ Geologists inspect the Devil's Thumb Sinkhole, which is located in travertine at the base of the Mammoth Hot Springs Terraces, before injecting multiple tracers to determine flow paths, transit times, and chemical Water from Boiling River (Mammoth Hot reaction processes in a natural aquifer. Hot Springs) was sampled at many intervals during a water from pools on top of this terrace flows multicomponent tracer experiment. Analysis of over the orange travertine and down into the data from this major outflow of the Mammoth sinkhole. Inactive travertine is grey; the oldest system (-40°C and 27 f&ls flow rate) provides deposits support several types of trees. information about the flow path, transit titles, and chemical reaction processes of a natural aquifer. This information is used to test hypotheses and field approaches for characterizing geothermal, petroleum, and environmental reservoirs. A team of geologists collected more than 250 samples over an 18-hr period at Boiling River —one of many remote field sample processing sites—during the multicomponent tracer experiment. In this wilderness area, team members used the environmentally benign transport system (shown in red) to move equipment and samples. Closeup of the Devil's Thumb Sinkhole shows wet, actively depositing travertine in orange and old, degrading travertine in white. These moths caught in the hot springs were fossilized as hydrothermal solutions flowed across the ground surface at Mammoth Hot Springs in Yellowstone National Park. -

Bean Counting Teacher Notes and Materials 1.3: Elements
Developmental Lesson FC #1.3: Bean Counting Teacher Notes and Materials 1.3: Elements Goal Facets: 01 The student understands that in every atom that makes up one kind of element, the number of protons is the same, but the number of neutrons or electrons may vary. 02 The student understands that all substances come from a limited number of elements in our universe. 03 The student knows that the nucleus of an atom does not change easily, which explains why we cannot easily make one element from another element. 04 The student knows that an atom's identity remains the same regardless of the state of matter or the type of matter of which it is a part. Background The entire universe consists of only a limited number of elements, which make up everything that we experience in our daily lives as well as the stars and galaxies, which shine millions of light-years away. An atom of a particular element can be identified by the number of protons in its nucleus. For example, if an atom has 11 protons it is a sodium atom. If the number of protons is not 11, then it is not sodium. For any given element, the number of neutrons or electrons may vary without altering the identity of the element. For example, one fluorine atom may have 9 protons and 9 neutrons while another fluorine atom may have 9 protons and 10 neutrons. These are said to be two different isotopes of fluorine. Isotopes are atoms of an element with different numbers of neutrons. -

SPECTROSCOPY of NEUTRON-UNBOUND FLUORINE by Gregory Arthur Christian a DISSERTATION Submitted to Michigan State University in Pa
SPECTROSCOPY OF NEUTRON-UNBOUND FLUORINE by Gregory Arthur Christian A DISSERTATION Submitted to Michigan State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY PHYSICS 2011 ABSTRACT SPECTROSCOPY OF NEUTRON-UNBOUND FLUORINE by Gregory Arthur Christian Neutron-unbound states in 27F and 28F have been measured using the technique of invariant mass spectroscopy, with the unbound states populated from nucleon knock out reactions, 29Ne(9Be, X). Neutrons resulting from the decay of unbound states were detected in the Modular Neutron Array (MoNA), which recorded their positions and times of flight. Residual charged fragments were deflected by the dipole Sweeper magnet and passed through a series of charged particle detectors that provided position, energy loss, and total kinetic energy measurements. The charged particle measurements were sufficient for isotope separation and identification as well as reconstruction of momentum vectors at the target. In addition to the neutron and charged particle detectors, a CsI(Na) array (CAESAR) surrounded the target, allowing a unique determination of the decay path of the unbound states. In 27F, a resonance was observed to decay to the ground state of 26F with 380 60 keV relative ± energy, corresponding to an excited level in 27F at 2500 220 keV. The 28F relative energy ± spectrum indicates the presence of multiple, unresolved resonances; however, it was possible to +50 27 determine the location of the ground state resonance as 210 60 keV above the ground state of F. − This translates to a 28F binding energy of 186.47 0.20 MeV. ± Comparison of the 28F binding energy to USDA/USDB shell model predictions provides in- sight into the role of intruder configurations in the ground state structure of 28F and the low-Z limit of the “island of inversion” around N = 20. -

Neutron Drip Line of Z = 9–11 Isotopic Chains*
Chinese Physics C Vol. 44, No. 7 (2020) 074101 Neutron drip line of Z = 9–11 isotopic chains* 1 1 1;1) 1,2,3,4;2) Rong An(安荣) Guo-Fang Shen(申国防) Shi-Sheng Zhang(张时声) Li-Sheng Geng(耿立升) 1School of Physics, Beihang University, Beijing 100191, China 2Beijing Key Laboratory of Advanced Nuclear Materials and Physics, Beihang University, Beijing 100191, China 3Beijing Advanced Innovation Center for Big Data-based Precision Medicine, Beihang University, Beijing 100191, China 4School of Physics and Microelectronics, Zhengzhou University, Zhengzhou, Henan 450001, China Abstract: A recent experimental breakthrough identified the last bound neutron-rich nuclei in fluorine and neon iso- topes. Based on this finding, we perform a theoretical study of Z = 9, 10, 11, 12 isotopes in the relativistic mean field (RMF) model. The mean field parameters are assumed from the PK1 parameterization, and the pairing correlation is described by the particle number conservation BCS (FBCS) method recently formulated in the RMF model. We show that the FBCS approach plays an essential role in reproducing experimental results of fluorine and neon isotopes. Fur- thermore, we predict 39Na and 40Mg to be the last bound neutron-rich nuclei in sodium and magnesium isotopes. Keywords: drip line, relativistic mean field theory, particle number conservation DOI: 10.1088/1674-1137/44/7/074101 1 Introduction Numerous theoretical studies on the location of the neutron drip line have been conducted. Table 1 presents a partial list of various theoretical predictions in comparis- Properties of neutron-rich nuclei, in particular, the on with the experimental data. Clearly, not all of the the- location of the neutron drip line, play an important role oretical results agree with those of the experiments and not only in understanding nuclear stability with respect to with each other. -

Dosimety of FDG-18F Produced at the SOREQ Cyclotron CYCLONE 5/10
Production Yield of 18F-FDG at the SOREQ NRC Cyclotron CYCLONE 5/10 G. Haquin, M. B. Goldberg, Y. Ben Meir , T. Arbel and D. Ben Maman Soreq Nuclear Research Center, Yavne 81800, [email protected] Keywords: 18F-FDG, cyclotron, dose calibrator, PET. Abstract The SOREQ NRC proton cyclotron accelerator CYCLONE 5/10 began producing 18F- FDG at the beginning of 2001. 2-Fluoro-2 deoxy D-Glucose (FDG) labelled with radioactive 18F is used for Positron Emission Tomography (PET) imaging in medical diagnostic procedures. The FDG solution is produced at Soreq’s radiopharmacy following proton irradiation 18 18 of heavy water H2 O and chemical synthesis of the F-FDG compound at the cyclotron site. In the present work we have measured the absolute activity of 18F and FDG-18F produced and checked the accuracy of the dose calibrator measurement for 18F. The chemical reactor efficiency for synthetization of FDG was also determined. Introduction The Cyclone 5/10 supplies protons of 10 MeV nominal energy by accelerating hydrogen ions in a cyclotron. The beam is extracted to a Havar window of 25µm 18 18 thickness and bombards a H2 O water target. F is produced via the reaction 18O(p,n)18F, which has a peak in the cross section for proton energies between 5 and 8.5 MeV [1]. The reaction yield can be approximately expressed by the following expression: IA Y ≈ N p ⋅ σ TOT ⋅TTeff (1) Where Y is the reaction yield, Np is the number of protons (given by the beam ΙΑ current), <σΤΟΤ > is the average cross section for the reaction and TTeff is the effective target thickness. -

Imaging with 18F-Based Radiotracers
Am J Nucl Med Mol Imaging 2012;2(1):55-76 www.ajnmmi.us /ISSN:2160-8407/ajnmmi1109002 Review Article Positron emission tomography (PET) imaging with 18F-based radiotracers Mian M Alauddin Department of Experimental Diagnostic Imaging, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA Received September 27, 2011; accepted October 27, 2011; Epub December 15, 2011; Published January 1, 2012 Abstract: Positron Emission Tomography (PET) is a nuclear medicine imaging technique that is widely used in early detection and treatment follow up of many diseases, including cancer. This modality requires positron-emitting iso- tope labeled biomolecules, which are synthesized prior to perform imaging studies. Fluorine-18 is one of the several isotopes of fluorine that is routinely used in radiolabeling of biomolecules for PET; because of its positron emitting property and favorable half-life of 109.8 min. The biologically active molecule most commonly used for PET is 2-deoxy -2-18F-fluoro-β-D-glucose (18F-FDG), an analogue of glucose, for early detection of tumors. The concentrations of tracer accumulation (PET image) demonstrate the metabolic activity of tissues in terms of regional glucose metabolism and accumulation. Other tracers are also used in PET to image the tissue concentration. In this review, information on fluorination and radiofluorination reactions, radiofluorinating agents, and radiolabeling of various compounds and their application in PET imaging is presented. Keywords: Fluorine-18, positron emission tomography (PET), PET radiopharmaceuticals Introduction the polarized atoms. The C-F bond and its char- acteristics have been described extensively in a The chemistry of fluorine has been popular review [2]. -
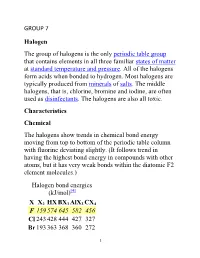
GROUP 7 Halogen the Group of Halogens Is the Only Periodic Table
GROUP 7 Halogen The group of halogens is the only periodic table group that contains elements in all three familiar states of matter at standard temperature and pressure. All of the halogens form acids when bonded to hydrogen. Most halogens are typically produced from minerals of salts. The middle halogens, that is, chlorine, bromine and iodine, are often used as disinfectants. The halogens are also all toxic. Characteristics Chemical The halogens show trends in chemical bond energy moving from top to bottom of the periodic table column with fluorine deviating slightly. (It follows trend in having the highest bond energy in compounds with other atoms, but it has very weak bonds within the diatomic F2 element molecules.) Halogen bond energies (kJ/mol)[4] X X2 HX BX3 AlX3 CX4 F 159 574 645 582 456 Cl 243 428 444 427 327 Br 193 363 368 360 272 1 I 151 294 272 285 239 Halogens are highly reactive, and as such can be harmful or lethal to biological organisms in sufficient quantities. This high reactivity is due to the high electronegativity of the atoms due to their high effective nuclear charge. They can gain an electron by reacting with atoms of other elements. Fluorine is one of the most reactive elements in existence, attacking otherwise-inert materials such as glass, and forming compounds with the heavier noble gases. It is a corrosive and highly toxic gas. The reactivity of fluorine is such that, if used or stored in laboratory glassware, it can react with glass in the presence of small amounts of water to form silicon tetrafluoride (SiF4). -

Nuclear Lattices, Mass and Stability
Open Access Library Journal Nuclear Lattices, Mass and Stability Henry Gu Cao, Zhiliang Cao, Wenan Qiang Northwestern University, Evanston, USA Email: [email protected] Received 20 April 2015; accepted 7 May 2015; published 13 May 2015 Copyright © 2015 by authors and OALib. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract A nucleus has a lattice configuration, a mass, and a half-life. There are many nuclear theories: BCS formalism focuses on Neutron-proton (np) pairing; AB initio calculation uses NCFC model; SEMF uses water drop model. However, the accepted theories give neither précised lattices of lower mass nuclei, nor an accurate calculation of nuclear mass. This paper uses the results of the latest Unified Field Theory (UFT) to derive a lattice configuration for each isotope. We found that a sim- plified BCS formalism can be used to calculate energies of the predicted lattice structure. Fur- thermore, mass calculation results and NMR data can be used to determine the right lattice struc- ture. Our results demonstrate the inseparable relationship among nuclear lattices, mass, and sta- bility. We anticipate that our essay will provide a new method that can predict the lattice of each isotope without the use of advanced mathematics. For example, the lattice of an unknown nucleus can be predicted using trial and error. The mass of the nuclear lattice can be calculated. If the cal- culation result matches the experimental data and NMR pattern supports the lattice as well, then the predicted nuclear lattice configuration is valid. -

A New Study of S-Process Nucleosynthesis in Massive Stars
A New Study of s-Process Nucleosynthesis in Massive Stars I. The Core-Helium Burning Phase L.-S. The,1 M.F. El Eid,2 and B.S. Meyer1 1Department of Physics & Astronomy, Clemson University, Clemson, SC 29634-1911 2Department of Physics, American University of Beirut (AUB), Beirut, Lebanon ABSTRACT We present a comprehensive study of s-process nucleosynthesis in 15, 20, 25, and 30 M⊙ stellar models having solar-like initial composition. The stars are evolved up to ignition of central neon with a 659 species network coupled to the stellar models. In this way, the initial composition from one burning phase to another is consistently determined, especially with respect to neutron capture reactions. The aim of our calculations is to gain a full account of the s-process yield from massive stars. In the present work, we focus primarily on the s-process during central helium burning and illuminate some major uncertainties affecting the calculations. We briefly show how advanced burning can significantly affect the products of the core helium burning s-process and, in particular, can greatly deplete 80Kr that was strongly overproduced in the earlier core helium burning phase; however, we leave a complete analysis of the s-process during the advanced evolutionary phases (especially in shell carbon burning) to a subsequent paper. Our results can help to constrain the yield of the s-process material from massive stars during their pre-supernova evolution. Subject headings: nuclear reactions, nucleosynthesis, abundances –stars: evolution –stars: interiors arXiv:astro-ph/9812238v1 11 Dec 1998 – 2 – 1. INTRODUCTION According to phenomenological analysis (e.g. -
![Arxiv:2007.08529V2 [Hep-Ph] 23 Oct 2020 Nificantly Less Constrained Experimentally Than the Elec- Tromagnetic Charge Distribution](https://docslib.b-cdn.net/cover/6078/arxiv-2007-08529v2-hep-ph-23-oct-2020-ni-cantly-less-constrained-experimentally-than-the-elec-tromagnetic-charge-distribution-4386078.webp)
Arxiv:2007.08529V2 [Hep-Ph] 23 Oct 2020 Nificantly Less Constrained Experimentally Than the Elec- Tromagnetic Charge Distribution
INT-PUB-20-026 Coherent elastic neutrino{nucleus scattering: EFT analysis and nuclear responses Martin Hoferichter,1, 2, ∗ Javier Men´endez,3, 4, y and Achim Schwenk5, 6, 7, z 1Albert Einstein Center for Fundamental Physics, Institute for Theoretical Physics, University of Bern, Sidlerstrasse 5, 3012 Bern, Switzerland 2Institute for Nuclear Theory, University of Washington, Seattle, WA 98195-1550, USA 3Department of Quantum Physics and Astrophysics and Institute of Cosmos Sciences, University of Barcelona, Spain 4Center for Nuclear Study, The University of Tokyo, 113-0033 Tokyo, Japan 5Institut f¨urKernphysik, Technische Universit¨atDarmstadt, 64289 Darmstadt, Germany 6ExtreMe Matter Institute EMMI, GSI Helmholtzzentrum f¨urSchwerionenforschung GmbH, 64291 Darmstadt, Germany 7Max-Planck-Institut f¨urKernphysik, Saupfercheckweg 1, 69117 Heidelberg, Germany The cross section for coherent elastic neutrino{nucleus scattering (CEνNS) depends on the re- sponse of the target nucleus to the external current, in the Standard Model (SM) mediated by the exchange of a Z boson. This is typically subsumed into an object called the weak form factor of the nucleus. Here, we provide results for this form factor calculated using the large-scale nuclear shell model for a wide range of nuclei of relevance for current CEνNS experiments, including ce- sium, iodine, argon, fluorine, sodium, germanium, and xenon. In addition, we provide the responses needed to capture the axial-vector part of the cross section, which does not scale coherently with the number of neutrons, but may become relevant for the SM prediction of CEνNS on target nuclei with nonzero spin. We then generalize the formalism allowing for contributions beyond the SM.