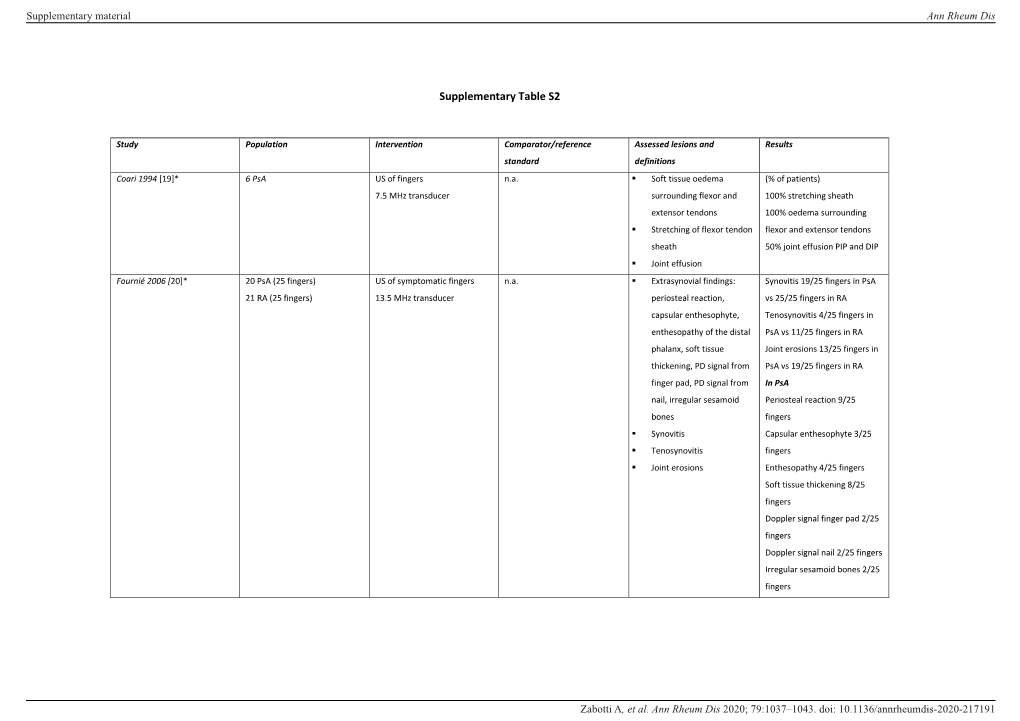
Supplementary Table S2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bioarchaeological Implications of Calcaneal Spurs in the Medieval Nubian Population of Kulubnarti
Bioarchaeological Implications of Calcaneal Spurs in the Medieval Nubian Population of Kulubnarti Lindsay Marker Department of Anthropology Primary Thesis Advisor Matthew Sponheimer, Department of Anthropology Defense Committee Members Douglas Bamforth, Department of Anthropology Patricia Sullivan, Department of English University of Colorado at Boulder April 2016 1 Table of Contents List of Figures ............................................................................................................................. 4 Abstract …................................................................................................................................... 6 Chapter 1: Introduction …........................................................................................................... 8 Chapter 2: Anatomy …................................................................................................................ 11 2.1 Chapter Overview …................................................................................................. 11 2.2 Bone Composition …................................................................................................ 11 2.3 Plantar Foot Anatomy …........................................................................................... 12 2.4 Posterior Foot Anatomy …........................................................................................ 15 Chapter 3: Literature Review and Background of Calcaneal Enthesophytes ............................. 18 3.1 Chapter Overview …................................................................................................ -

9 Impingement and Rotator Cuff Disease
Impingement and Rotator Cuff Disease 121 9 Impingement and Rotator Cuff Disease A. Stäbler CONTENTS Shoulder pain and chronic reduced function are fre- quently heard complaints in an orthopaedic outpa- 9.1 Defi nition of Impingement Syndrome 122 tient department. The symptoms are often related to 9.2 Stages of Impingement 123 the unique anatomic relationships present around the 9.3 Imaging of Impingement Syndrome: Uri Imaging Modalities 123 glenohumeral joint ( 1997). Impingement of the 9.3.1 Radiography 123 rotator cuff and adjacent bursa between the humeral 9.3.2 Ultrasound 126 head and the coracoacromial arch are among the most 9.3.3 Arthrography 126 common causes of shoulder pain. Neer noted that 9.3.4 Magnetic Resonance Imaging 127 elevation of the arm, particularly in internal rotation, 9.3.4.1 Sequences 127 9.3.4.2 Gadolinium 128 causes the critical area of the cuff to pass under the 9.3.4.3 MR Arthrography 128 coracoacromial arch. In cadaver dissections he found 9.4 Imaging Findings in Impingement Syndrome alterations attributable to mechanical impingement and Rotator Cuff Tears 130 including a ridge of proliferative spurs and excres- 9.4.1 Bursal Effusion 130 cences on the undersurface of the anterior margin 9.4.2 Imaging Following Impingement Test Injection 131 Neer Neer 9.4.3 Tendinosis 131 of the acromion ( 1972). Thus it was who 9.4.4 Partial Thickness Tears 133 introduced the concept of an impingement syndrome 9.4.5 Full-Thickness Tears 134 continuum ranging from chronic bursitis and partial 9.4.5.1 Subacromial Distance 136 tears to complete tears of the supraspinatus tendon, 9.4.5.2 Peribursal Fat Plane 137 which may extend to involve other parts of the cuff 9.4.5.3 Intramuscular Cysts 137 Neer Matsen 9.4.6 Massive Tears 137 ( 1972; 1990). -

Rotator Cuff and Subacromial Impingement Syndrome: Anatomy, Etiology, Screening, and Treatment
Rotator Cuff and Subacromial Impingement Syndrome: Anatomy, Etiology, Screening, and Treatment The glenohumeral joint is the most mobile joint in the human body, but this same characteristic also makes it the least stable joint.1-3 The rotator cuff is a group of muscles that are important in supporting the glenohumeral joint, essential in almost every type of shoulder movement.4 These muscles maintain dynamic joint stability which not only avoids mechanical obstruction but also increases the functional range of motion at the joint.1,2 However, dysfunction of these stabilizers often leads to a complex pattern of degeneration, rotator cuff tear arthropathy that often involves subacromial impingement.2,22 Rotator cuff tear arthropathy is strikingly prevalent and is the most common cause of shoulder pain and dysfunction.3,4 It appears to be age-dependent, affecting 9.7% of patients aged 20 years and younger and increasing to 62% of patients of 80 years and older ( P < .001); odds ratio, 15; 95% CI, 9.6-24; P < .001.4 Etiology for rotator cuff pathology varies but rotator cuff tears and tendinopathy are most common in athletes and the elderly.12 It can be the result of a traumatic event or activity-based deterioration such as from excessive use of arms overhead, but some argue that deterioration of these stabilizers is part of the natural aging process given the trend of increased deterioration even in individuals who do not regularly perform overhead activities.2,4 The factors affecting the rotator cuff and subsequent treatment are wide-ranging. The major objectives of this exposition are to describe rotator cuff anatomy, biomechanics, and subacromial impingement; expound upon diagnosis and assessment; and discuss surgical and conservative interventions. -

IGHS Poster 01: History of the Australian Hand Surgery Society
IGHS Poster 01: History of the Australian Hand Surgery Society Category: Other Keyword: Other Not a clinical study ♦ Michael Tonkin, MD ♦ Richard Honner, MD Hypothesis: The Australian Hand Club was established in 1972, following discussion between members of the New South Wales Hand Surgery Association and the plastic surgeons of Melbourne under the direction of Sir Benjamin Rank, who became the first President. The other elected Office Bearers were: President Elect - Alan McJannet Secretary - Frank Harvey Treasurer - Richard Honner Committee Members - Peter Millroy, Don Robinson, Bernard O’Brien In 1990 the name was changed to the Australian Hand Surgery Society. This now has 159 active members, 18 overseas members, 28 honorary members and 9 provisional members. The current Board consists of: President - Randall Sach President Elect - David Stabler Ex-officio President - Stephen Coleman Secretary - Philip Griffin Treasurer - Douglass Wheen Executive Committee - Anthony Beard, David McCombe, Jeffrey Ecker An Annual Scientific Meeting with overseas Guest Professors is conducted each year, often associated with a separate two day program in hand surgery for Registrars on surgical training schemes in Australia and New Zealand. The AHSS also convenes hand surgery programmes for the Annual Scientific Meetings of the Australian Orthopaedic Association and the Royal Australasian College of Surgeons. Combined meetings with other hand surgery societies have been held, including with New Zealand, Singapore and most recently with the ASSH in Kauai, USA, March 2012. The AHSS became a member of the International Federation of Societies for Surgery of the Hand (IFSSH) in 1977 and was a founding member of the Asia-Pacific Federation of Societies for Surgery of the Hand (APFSSH) in 1997. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

Bilateral Simultaneous Rupture of the Quadriceps Tendons in Healthy Individuals Takuro Moriya1,2* and Abe Yoshihiro1
Moriya et al. Trauma Cases Rev 2016, 2:043 Volume 2 | Issue 3 ISSN: 2469-5777 Trauma Cases and Reviews Case Report: Open Access Bilateral Simultaneous Rupture of the Quadriceps Tendons in Healthy Individuals Takuro Moriya1,2* and Abe Yoshihiro1 1Department of Orthopaedic Surgery, Chiba Rosai Hospital, Japan 2Department of Orthopaedic Surgery, Chiba Kaihin Municipal Hospital, Japan *Corresponding author: Takuro Moriya, Department of Orthopaedic Surgery, Chiba Rosai Hospital, 2-16 Tatsumidai- higashi, Ichihara 290-0003, Japan, Tel: +81-436-74-1111, Fax: +81-436-74-1151, E-mail: [email protected] Abstract Quadriceps tendon rupture is an uncommon injury in healthy individuals. This paper presents two case reports of patients of bilateral quadriceps tendon rupture, who were misdiagnosed as muscle weakness of quadriceps with contusion of the knee joint. Subsequent physical examination showed a supra-patellar gap, moderate hemarthrosis of both knees, and failure of active knee extension. MRI showed bilateral rupture of the quadriceps tendons at the osteotendinous junction. Radiographs described the depression in the suprapatellar soft tissue, patella baja and an avulsion bony fragment on the patella. Surgery confirmed the MRI observation, so transosseous suturing and augmentation were undertaken. Both patients returned to a normal life with useful function. Adequate physical examination and correct understanding of both radiograph and MRI were required to prevent misdiagnosis. Keywords Bilateral quadriceps tendon ruptures, Healthy individuals Figure 1: Suprapatellar gap in Case 1. Introduction avulsion fragment on the patella (Figure 3). The patellar heights of his right and left knees were 0.89 and 0.68, respectively, using the Insall- Rupture of the quadriceps tendon is an uncommon injury, and Saivati method. -

ESSR 2013 | 1 2 | ESSR 2013 Essrsport 2013 Injuries Musculoskeletal Radiology June 13–15, MARBELLA/SPAIN
Final Programme property of Marbella City Council ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN Content 3 Welcome 4–5 ESSR Committee & Invited Speakers 6 General Information 11/13 Programme Overview ESSR 2013 | 1 2 | ESSR 2013 ESSRSport 2013 Injuries MUSCULOSKELETAL RADIOLOGY JUNE 13–15, MARBELLA/SPAIN from the ESSR 2013 Congress President ME Welcome LCO On behalf of the ESSR it is a pleasure to invite you to participate in the 20th Annual Scientific Meeting WE of the European Skeletal Society to be held in Marbella, Spain, on June 13–15, 2013, at the Palacio de Congresos located in the center of the city. The scientific programme will focus on “Sports Lesions”, with a refresher course lasting two days dedicated to actualised topics. The programme will include focus sessions and hot topics, as well as different sessions of the subcommittees of the society. There will be a special session on Interventional Strategies in Sports Injuries. The popular “hands on” ultrasound workshops in MSK ultrasound will be held on Thursday 13, 2013, during the afternoon, with the topic of Sports Lesions. Basic and advanced levels will be offered. A state-of-the-art technical exhibition will display the most advanced technical developments in the area of musculoskeletal pathology. The main lobby will be available for workstations for the EPOS as well as technical exhibits. Marbella is located in the south of Spain, full of life and with plenty of cultural and tourist interest, with architectural treasures of the traditional and popular Andalusian culture. -

Rotator Cuff Tears
OrthoInfo Basics Rotator Cuff Tears What is a rotator cuff? One of the Your rotator cuff helps you lift your arm, rotate it, and reach up over your head. most common middle-age It is made up of muscles and tendons in your shoulder. These struc- tures cover the head of your upper arm bone (humerus). This “cuff” complaints is holds the upper arm bone in the shoulder socket. shoulder pain. Rotator cuff tears come in all shapes and sizes. They typically occur A frequent in the tendon. source of that Partial tears. Many tears do not completely sever the soft tissue. Full thickness tears. A full or "complete" tear will split the soft pain is a torn tissue into two, sometimes detaching the tendon from the bone. rotator cuff. Rotator Cuff Bursa A torn rotator cuff will Tendon Clavicle (Collarbone) Humerus weaken your shoulder. (Upper Arm) This means that many Normal shoulder anatomy. daily activities, like combing your hair or Scapula getting dressed, may (Shoulder Blade) become painful and difficult to do. Rotator Cuff Tendon A complete tear of the rotator cuff tendon. 1 OrthoInfo Basics — Rotator Cuff Tears What causes rotator cuff tears? There are two main causes of rotator cuff repeating the same shoulder motions again and tears: injury and wear. again. Injury. If you fall down on your outstretched This explains why rotator cuff tears are most arm or lift something too heavy with a jerking common in people over 40 who participate in motion, you could tear your rotator cuff. This activities that have repetitive overhead type of tear can occur with other shoulder motions. -

Open Fracture As a Rare Complication of Olecranon Enthesophyte in a Patient with Gout Rafid Kakel, MD, and Joseph Tumilty, MD
A Case Report & Literature Review Open Fracture as a Rare Complication of Olecranon Enthesophyte in a Patient With Gout Rafid Kakel, MD, and Joseph Tumilty, MD has been reported in the English literature. The patient Abstract provided written informed consent for print and elec- Enthesophytes are analogous to osteophytes of osteo- tronic publication of this case report. arthritis. Enthesopathy is the pathologic change of the enthesis, the insertion site of tendons, ligaments, and CASE REPORT joint capsules on the bone. In gout, the crystals of mono- A 50-year-old man with chronic gout being treated with sodium urate monohydrate may provoke an inflamma- tory reaction that eventually may lead to ossification at allopurinol (and indomethacin on an as-needed basis) those sites (enthesophytes). Here we report the case of presented to the emergency department. He reported a man with chronic gout who sustained an open fracture of an olecranon enthesophyte when he fell on his left elbow. To our knowledge, no other case of open fracture of an enthesophyte has been reported in the English literature. nthesophytes are analogous to osteophytes of osteoarthritis. Enthesopathy is the pathologic change of the enthesis, the insertion site of ten- dons, ligaments, and joint capsules on the bone. EEnthesopathy occurs in a wide range of conditions, notably spondyloarthritides, crystal-induced diseases, and repeated minor trauma to the tendinous attach- ments to bones. Enthesopathy can be asymptomatic or symptomatic. In gout, crystals of monosodium urate are found in and around the joints—the cartilage, epiphyses, synovial membrane, tendons, ligaments, and enthesis. Figure 1. Small wound at patient’s left elbow. -
Heel Enthesopathy of Diffuse Idiopathic Skeletal Hyperostosis
Images in Rheumatology Heel Enthesopathy of Diffuse Idiopathic Skeletal Hyperostosis Resembling Enthesitis of Spondyloarthritis IGNAZIO OLIVIERI, MD, SALVATORE D’ANGELO, MD, Rheumatology Department of Lucania, San Carlo Hospital, Contrada Macchia Romana, 85100 Potenza, Italy; and Madonna delle Grazie Hospital; FRANCESCO BORRACCIA, Researcher, Radiology Department, San Carlo Hospital; ANGELA PADULA, MD, Senior Researcher, Rheumatology Department of Lucania, San Carlo Hospital, and Madonna delle Grazie Hospital, Matera, Italy. Address correspondence to Dr. Olivieri; E-mail: [email protected]. J Rheumatol 2010;37:192–3; doi.10.3899/jrheum.090514 Diffuse idiopathic skeletal hyperostosis (DISH) and anky- tendons, resembling the typical fusiform soft tissue swelling losing spondylitis (AS) are 2 clearly different disease enti- of Achilles enthesitis of spondyloarthritis5 (Figure 1). ties having in common the involvement of the axial skeleton However, palpation of the region did not reveal any inflam- and the peripheral entheses1,2. Both diseases produce bone matory findings of enthesitis but did reveal bone prolifera- proliferation in the spine and at the extraspinal entheseal tion due to large spurs, a condition confirmed by radio- sites in the later phases of their course. Although the aspects graphs (Figure 2). A sacroiliac joint computed tomography of the bone proliferations of the 2 diseases are dissimilar, (CT) scan showed the normal aspect of joint space and bony confusion of radiographic differential diagnosis between the margins together with the presence of capsular ossifications 2 diseases exists, partly as a consequence of a lack of aware- (Figure 3). ness of their respective characteristic features2,3. It has been pointed out that the differential diagnosis between DISH and REFERENCES longstanding advanced AS is not limited to the radiologic 1. -

Clinical and Imaging Assessment of Peripheral Enthesitis in Ankylosing Spondylitis
Special RepoRt Clinical and imaging assessment of peripheral enthesitis in ankylosing spondylitis Enthesitis, defined as inflammation of the origin and insertion of ligaments, tendons, aponeuroses, annulus fibrosis and joint capsules, is a hallmark of ankylosing spondylitis. The concept of entheseal organ prone to pathological changes in ankylosing spondylitis and other spondyloarthritis is well recognized. The relevant role of peripheral enthesitis is supported by the evidence that this feature, on clinical examination, has been included in the classification criteria of Amor (heel pain or other well-defined enthesopathic pain), European Spondiloarthropathy Study Group and Assessment in SpondyloArthritis International Society for axial and peripheral spondyloarthritis. Nevertheless, the assessment of enthesitis has been improved by imaging techniques to carefully detect morphological abnormalities and to monitor disease activity. 1 Keywords: ankylosing spondylitis n clinical assessment n enthesitis n MrI Antonio Spadaro* , n spondyloarthritis n ultrasound Fabio Massimo Perrotta1, In primary ankylosing spondylitis (AS) the fre- has proven to be a highly sensitive and nonin- Alessia Carboni1 quency of peripheral enthesitis has been found vasive tool to assess the presence of enthesitis, & Antongiulio Scarno1 to be between 25 and 58% [1], however, the real characterized by hypoechogenicity with loss 1Dipartimento di Medicina Interna e prevalence of this feature depends on the type of tendon fibrillar pattern, tendon thickening, Specialità -

Acute Management of Soft Tissue Injuries
www.acpsm.org Acute Management of Soft Tissue Injuries Protection, Rest, Ice, Compression, and Elevation Guidelines www.acpsm.org Management of acute soft tissue injury using Protection Rest Ice Compression and Elevation: Recommendations from the Association of Chartered Physiotherapists in Sports and Exercise Medicine (ACPSM) Chris M Bleakley1, Philip D Glasgow2, Nicola Phillips2, Laura Hanna2, Michael J Callaghan2, Gareth W Davison3, Ty J Hopkins3, Eamonn Delahunt3 1Lead author and guarantor 2ACPSM consensus panel 3External authors and contributors Acknowledgements to other ACPSM contributors: Lynn Booth, Nicola Combarro, Sian Knott, Chris McNicholl and Colin Paterson for their assistance with literature searching, data extraction, and interpretation of outcomes. This work was funded by the Association of Chartered Physiotherapists in Sports and Exercise Medicine (ACPSM). The guidelines are endorsed by the Chartered Society of Physiotherapy’s Supporting Knowledge in Physiotherapy Practice Programme (SKIPP), after peer review from their Good Practice Panel in October 2010. CONTENTS Chapter 1: Project methods Chapter 2: What is the magnitude and depth of cooling associated with ice? Chapter 3: Can PRICE decrease the infl ammatory response after acute soft tissue injury? Chapter 4: What effect does mechanical loading have on infl ammation and soft tissue healing after acute injury? Chapter 5: Do the physiological effects of local tissue cooling affect function, sporting performance and injury risk? Chapter 6: Which components of PRICE are effective in the clinical management of acute soft tissue injury? Chapter 7: Executive summary Chapter 8: Appendices Chapter 1 Project methods Background The need for guidelines Soft tissue injury is a common problem in sport, recreational and physical activities.