Patellar Tendon Tear
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: a Theoretical Perspective
The Influence of Altered Lower-Extremity Kinematics on Patellofemoral Joint Dysfunction: A Theoretical Perspective Christopher M. Powers, PT, PhD 1 Although patellofemoral pain (PFP) is recognized as being one of the most common disorders of It has been recognized by sev- the lower extremity, treatment guidelines and underlying rationales remain vague and controver- eral authors that the patel- sial. The premise behind most treatment approaches is that PFP is the result of abnormal patellar lofemoral joint may be influenced CLINICAL COMMENTARY tracking and/or patellar malalignment. Given as such, interventions typically focus on the joint by the segmental interactions of itself and have traditionally included strengthening the vastus medialis oblique, taping, bracing, the lower extremity.6,7,21,27,34,45 Ab- soft tissue mobilization, and patellar mobilization. More recently, it has been recognized that the normal motion(s) of the tibia and patellofemoral joint and, therefore, PFP may be influenced by the interaction of the segments and femur in the transverse and frontal joints of the lower extremity. In particular, abnormal motion of the tibia and femur in the transverse and frontal planes may have an effect on patellofemoral joint mechanics. With this in planes are believed to have an mind, interventions aimed at controlling hip and pelvic motion (proximal stability) and ankle/foot effect on patellofemoral joint me- motion (distal stability) may be warranted and should be considered when treating persons with chanics and therefore PFP. An un- patellofemoral joint dysfunction. The purpose of this paper is to provide a biomechanical derstanding of how lower- overview of how altered lower-extremity mechanics may influence the patellofemoral joint. -

Closure of Patellar Tendon Defect in ACL Reconstruction
Systematic Review Closure of Patellar Tendon Defect in Anterior Cruciate Ligament Reconstruction With BoneePatellar TendoneBone Autograft: Systematic Review of Randomized Controlled Trials Rachel M. Frank, M.D., Randy Mascarenhas, M.D., Marc Haro, M.D., Nikhil N. Verma, M.D., Brian J. Cole, M.D., M.B.A., Charles A. Bush-Joseph, M.D., and Bernard R. Bach Jr., M.D. Purpose: This study aimed to systematically review the highest level of evidence on anterior cruciate ligament (ACL) reconstruction with boneepatellar tendonebone (BPTB) autografts with patellar tendon defect closure versus no closure after surgery. Methods: We performed a systematic review of multiple medical databases using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Level I and Level II randomized controlled trials comparing patellar tendon defect closure to no closure during ACL reconstruction with BPTB autografts were included. Two inde- pendent reviewers analyzed all studies. Descriptive statistics were calculated. Study methodological quality was analyzed using the Modified Coleman Methodology Score (MCMS) and Jadad scale. Results: Four studies with a combined 221 patients (154 male patients and 67 female patients) with an average age of 26.6 Æ 2.4 years (range, 17 to 54 years) were included. All studies randomized patients before surgery into ACLR with BPTB autografts either with patellar tendon defect closure or without closure. There were no differences in clinical outcomes (Lysholm score, Tegner scale, International Knee Documentation Committee [IKDC] classification, modified Larsen score, and Lauridsen rating) between groups. There were no significant differences in knee pain between groups. All studies reported imaging findings of the patellar tendon defect, with 2 studies showing no difference in appearance between groups, one study showing excessive scar formation with defect repair, and one study showing improved restoration of normal tendon appearance with defect repair. -

Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions
Review Article Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions Abstract Robert D. Bronstein, MD The knee is one of the most commonly injured joints in the body. Its Joseph C. Schaffer, MD superficial anatomy enables diagnosis of the injury through a thorough history and physical examination. Examination techniques for the knee described decades ago are still useful, as are more recently developed tests. Proper use of these techniques requires understanding of the anatomy and biomechanical principles of the knee as well as the pathophysiology of the injuries, including tears to the menisci and extensor mechanism, patellofemoral conditions, and osteochondritis dissecans. Nevertheless, the clinical validity and accuracy of the diagnostic tests vary. Advanced imaging studies may be useful adjuncts. ecause of its location and func- We have previously described the Btion, the knee is one of the most ligamentous examination.1 frequently injured joints in the body. Diagnosis of an injury General Examination requires a thorough knowledge of the anatomy and biomechanics of When a patient reports a knee injury, the joint. Many of the tests cur- the clinician should first obtain a rently used to help diagnose the good history. The location of the pain injured structures of the knee and any mechanical symptoms were developed before the avail- should be elicited, along with the ability of advanced imaging. How- mechanism of injury. From these From the Division of Sports Medicine, ever, several of these examinations descriptions, the structures that may Department of Orthopaedics, are as accurate or, in some cases, University of Rochester School of have been stressed or compressed can Medicine and Dentistry, Rochester, more accurate than state-of-the-art be determined and a differential NY. -

Patellar Tendinopathy: Some Aspects of Basic Science and Clinical Management
346 Br J Sports Med 1998;32:346–355 Br J Sports Med: first published as 10.1136/bjsm.32.4.346 on 1 December 1998. Downloaded from OCCASIONAL PIECE Patellar tendinopathy: some aspects of basic science and clinical management School of Human Kinetics, University of K M Khan, N MaVulli, B D Coleman, J L Cook, J E Taunton British Columbia, Vancouver, Canada K M Khan J E Taunton Tendon injuries account for a substantial tendinopathy, and the remainder to tendon or Victorian Institute of proportion of overuse injuries in sports.1–6 tendon structure in general. Sport Tendon Study Despite the morbidity associated with patellar Group, Melbourne, tendinopathy in athletes, management is far Victoria, Australia 7 Anatomy K M Khan from scientifically based. After highlighting The patellar tendon, the extension of the com- J L Cook some aspects of clinically relevant basic sci- mon tendon of insertion of the quadriceps ence, we aim to (a) review studies of patellar femoris muscle, extends from the inferior pole Department of tendon pathology that explain why the condi- of the patella to the tibial tuberosity. It is about Orthopaedic Surgery, tion can become chronic, (b) summarise the University of Aberdeen 3 cm wide in the coronal plane and 4 to 5 mm Medical School, clinical features and describe recent advances deep in the sagittal plane. Macroscopically it Aberdeen, Scotland, in the investigation of this condition, and (c) appears glistening, stringy, and white. United Kingdom outline conservative and surgical treatment NMaVulli options. BLOOD SUPPLY Department of The blood supply has been postulated to con- 89 Medicine, University tribute to patellar tendinopathy. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

Bilateral Simultaneous Rupture of the Quadriceps Tendons in Healthy Individuals Takuro Moriya1,2* and Abe Yoshihiro1
Moriya et al. Trauma Cases Rev 2016, 2:043 Volume 2 | Issue 3 ISSN: 2469-5777 Trauma Cases and Reviews Case Report: Open Access Bilateral Simultaneous Rupture of the Quadriceps Tendons in Healthy Individuals Takuro Moriya1,2* and Abe Yoshihiro1 1Department of Orthopaedic Surgery, Chiba Rosai Hospital, Japan 2Department of Orthopaedic Surgery, Chiba Kaihin Municipal Hospital, Japan *Corresponding author: Takuro Moriya, Department of Orthopaedic Surgery, Chiba Rosai Hospital, 2-16 Tatsumidai- higashi, Ichihara 290-0003, Japan, Tel: +81-436-74-1111, Fax: +81-436-74-1151, E-mail: [email protected] Abstract Quadriceps tendon rupture is an uncommon injury in healthy individuals. This paper presents two case reports of patients of bilateral quadriceps tendon rupture, who were misdiagnosed as muscle weakness of quadriceps with contusion of the knee joint. Subsequent physical examination showed a supra-patellar gap, moderate hemarthrosis of both knees, and failure of active knee extension. MRI showed bilateral rupture of the quadriceps tendons at the osteotendinous junction. Radiographs described the depression in the suprapatellar soft tissue, patella baja and an avulsion bony fragment on the patella. Surgery confirmed the MRI observation, so transosseous suturing and augmentation were undertaken. Both patients returned to a normal life with useful function. Adequate physical examination and correct understanding of both radiograph and MRI were required to prevent misdiagnosis. Keywords Bilateral quadriceps tendon ruptures, Healthy individuals Figure 1: Suprapatellar gap in Case 1. Introduction avulsion fragment on the patella (Figure 3). The patellar heights of his right and left knees were 0.89 and 0.68, respectively, using the Insall- Rupture of the quadriceps tendon is an uncommon injury, and Saivati method. -

Patellar Tendon Debridement Surgery
175 Cambridge Street, 4th floor Boston, MA 02114 Tel: 617-726-7500 PATELLAR TENDON DEBRIDEMENT SURGERY PREOPERATIVE INSTRUCTIONS Here are guidelines that will help you prepare for surgery: WITHIN ONE MONTH BEFORE SURGERY: The doctor will see you in the office. The doctor or his associate will do a preoperative history and physical examination and complete the necessary paperwork. He will write preoperative hospital orders and order laboratory tests. These tests usually include a complete blood count (and also electrocardiogram for patients over 40 years old.) SEVERAL DAYS BEFORE SURGERY: Wash the knee several times a day to get it as clean as you can. This decreases the risk of infection. Be careful not to get any scratches, cuts, sunburn, poison ivy, etc. The skin has to be in very good shape to prevent problems. You do not need to shave the knee. THE DAY BEFORE SURGERY: Please contact the doctor’s office to get the exact time you should report to the hospital for surgery. You can have nothing to eat or drink after midnight on the evening before surgery. It is very important to have a completely empty stomach prior to surgery for anesthesia safety reasons. If you have to take medication, you can take the medication with a sip of water early in the morning prior to surgery (but later tell the anesthesiologist you have done so). THE DAY OF SURGERY: Surgery is performed in the Wang building at MGH and at the Orthopedic Ambulatory Surgery Center at Mass General West in Waltham. • nothing to eat or drink • For surgery at MGH main campus in Boston: Report directly to the 12th floor of the Lunder Building, Center for Preoperative Care at Massachusetts General Hospital, two hours prior to surgery. -

Rotator Cuff Tears
OrthoInfo Basics Rotator Cuff Tears What is a rotator cuff? One of the Your rotator cuff helps you lift your arm, rotate it, and reach up over your head. most common middle-age It is made up of muscles and tendons in your shoulder. These struc- tures cover the head of your upper arm bone (humerus). This “cuff” complaints is holds the upper arm bone in the shoulder socket. shoulder pain. Rotator cuff tears come in all shapes and sizes. They typically occur A frequent in the tendon. source of that Partial tears. Many tears do not completely sever the soft tissue. Full thickness tears. A full or "complete" tear will split the soft pain is a torn tissue into two, sometimes detaching the tendon from the bone. rotator cuff. Rotator Cuff Bursa A torn rotator cuff will Tendon Clavicle (Collarbone) Humerus weaken your shoulder. (Upper Arm) This means that many Normal shoulder anatomy. daily activities, like combing your hair or Scapula getting dressed, may (Shoulder Blade) become painful and difficult to do. Rotator Cuff Tendon A complete tear of the rotator cuff tendon. 1 OrthoInfo Basics — Rotator Cuff Tears What causes rotator cuff tears? There are two main causes of rotator cuff repeating the same shoulder motions again and tears: injury and wear. again. Injury. If you fall down on your outstretched This explains why rotator cuff tears are most arm or lift something too heavy with a jerking common in people over 40 who participate in motion, you could tear your rotator cuff. This activities that have repetitive overhead type of tear can occur with other shoulder motions. -

Open Fracture As a Rare Complication of Olecranon Enthesophyte in a Patient with Gout Rafid Kakel, MD, and Joseph Tumilty, MD
A Case Report & Literature Review Open Fracture as a Rare Complication of Olecranon Enthesophyte in a Patient With Gout Rafid Kakel, MD, and Joseph Tumilty, MD has been reported in the English literature. The patient Abstract provided written informed consent for print and elec- Enthesophytes are analogous to osteophytes of osteo- tronic publication of this case report. arthritis. Enthesopathy is the pathologic change of the enthesis, the insertion site of tendons, ligaments, and CASE REPORT joint capsules on the bone. In gout, the crystals of mono- A 50-year-old man with chronic gout being treated with sodium urate monohydrate may provoke an inflamma- tory reaction that eventually may lead to ossification at allopurinol (and indomethacin on an as-needed basis) those sites (enthesophytes). Here we report the case of presented to the emergency department. He reported a man with chronic gout who sustained an open fracture of an olecranon enthesophyte when he fell on his left elbow. To our knowledge, no other case of open fracture of an enthesophyte has been reported in the English literature. nthesophytes are analogous to osteophytes of osteoarthritis. Enthesopathy is the pathologic change of the enthesis, the insertion site of ten- dons, ligaments, and joint capsules on the bone. EEnthesopathy occurs in a wide range of conditions, notably spondyloarthritides, crystal-induced diseases, and repeated minor trauma to the tendinous attach- ments to bones. Enthesopathy can be asymptomatic or symptomatic. In gout, crystals of monosodium urate are found in and around the joints—the cartilage, epiphyses, synovial membrane, tendons, ligaments, and enthesis. Figure 1. Small wound at patient’s left elbow. -

Recurrent Unremitting Patellar Tendonitis/ Tendonosis Rehabilitation Program
Page 1 of 3 Recurrent Unremitting Patellar Tendonitis/ Tendonosis Rehabilitation Program I. Phase I Goals: Diminish pain and inflammation Promote tendon healing Improve quadriceps strength Enhance flexibility Control functional stresses Treatment Regimen: • Hot packs applied to knee • Ultrasound to patellar tendon • Transverse friction massage • Warm-up bicycle (10-12 min.) • Stretch (hamstrings quadriceps, gastroc) • Application of pain stimulation to each side of patella tendon or infra-patellar fat pad x 10 minutes • Electrical stimulation parameters • Waveform: Russian • Frequency: 2500 H2 pulse; width: 200 MS; Rate: 50/sec • 60 pulses per second (pps) • duty cycle 10 on/10 off; ramp of 1 second • pad placement- 1”x1” electrodes placed on each side of inflamed/painful tendon (After 3 minutes, palpate tendon, should be less painful and becoming numb, if not, move electrodes) • Quadriceps strengthening program (Level I) • E-stim to quadriceps* • Quad sets* • SLR flexion* • Hip adduction/abduction* • Vertical squats (tilt board) • Hip flexion/extension • Toe-calf raises • Bicycle (15-20 min.) *Monitor subjective pain level response (goal level 5-7) • Pool program • Stretch (aggressive stretching) • Laser • Cryotherapy II. Phase II Emphasize eccentric training for quadriceps Goals: Gradual increase stress to patellar tendon Enhance quadriceps strength Improve flexibility Gradual increase functional activities Copyright © by the Advanced Continuing Education Institute, LLC. AdvancedCEU.com. All Rights Reserved. Any redistribution, alteration, -

Heel Enthesopathy of Diffuse Idiopathic Skeletal Hyperostosis
Images in Rheumatology Heel Enthesopathy of Diffuse Idiopathic Skeletal Hyperostosis Resembling Enthesitis of Spondyloarthritis IGNAZIO OLIVIERI, MD, SALVATORE D’ANGELO, MD, Rheumatology Department of Lucania, San Carlo Hospital, Contrada Macchia Romana, 85100 Potenza, Italy; and Madonna delle Grazie Hospital; FRANCESCO BORRACCIA, Researcher, Radiology Department, San Carlo Hospital; ANGELA PADULA, MD, Senior Researcher, Rheumatology Department of Lucania, San Carlo Hospital, and Madonna delle Grazie Hospital, Matera, Italy. Address correspondence to Dr. Olivieri; E-mail: [email protected]. J Rheumatol 2010;37:192–3; doi.10.3899/jrheum.090514 Diffuse idiopathic skeletal hyperostosis (DISH) and anky- tendons, resembling the typical fusiform soft tissue swelling losing spondylitis (AS) are 2 clearly different disease enti- of Achilles enthesitis of spondyloarthritis5 (Figure 1). ties having in common the involvement of the axial skeleton However, palpation of the region did not reveal any inflam- and the peripheral entheses1,2. Both diseases produce bone matory findings of enthesitis but did reveal bone prolifera- proliferation in the spine and at the extraspinal entheseal tion due to large spurs, a condition confirmed by radio- sites in the later phases of their course. Although the aspects graphs (Figure 2). A sacroiliac joint computed tomography of the bone proliferations of the 2 diseases are dissimilar, (CT) scan showed the normal aspect of joint space and bony confusion of radiographic differential diagnosis between the margins together with the presence of capsular ossifications 2 diseases exists, partly as a consequence of a lack of aware- (Figure 3). ness of their respective characteristic features2,3. It has been pointed out that the differential diagnosis between DISH and REFERENCES longstanding advanced AS is not limited to the radiologic 1. -
Knee Extensor Tendonitis
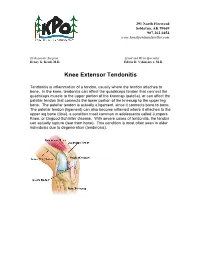
291 North Fireweed Soldotna, AK 99669 907-262-6454 www.kenaipeninsulaortho.com ______________________________________________________________________________________ Orthopaedic Surgeon: Hand and Wrist Specialist: Henry G. Krull, M.D. Edwin D. Vyhmeister, M.D. Knee Extensor Tendonitis Tendonitis is inflammation of a tendon, usually where the tendon attaches to bone. In the knee, tendonitis can affect the quadriceps tendon that connect the quadriceps muscle to the upper portion of the kneecap (patella), or can affect the patellar tendon that connects the lower portion of the kneecap to the upper leg bone. The patellar tendon is actually a ligament, since it connects bone to bone. The patellar tendon (ligament) can also become inflamed where it attaches to the upper leg bone (tibia), a condition most common in adolescents called Jumpers Knee, or Osgood-Schlatter disease. With severe cases of tendonitis, the tendon can actually rupture (tear from bone). This condition is most often seen in older individuals due to degeneration (tendinosis). 291 North Fireweed Soldotna, AK 99669 907-262-6454 www.kenaipeninsulaortho.com Symptoms: Pain is the hallmark of extensor tendonitis, and is located either just above the patella (quadriceps tendonitis), or just below the patella (patellar tendonitis). Sometimes there is an injury, but tendonitis is more common with overuse and under-conditioning. There is occasionally swelling and warmth over the inflamed tendon. The joint may become stiff, but range of motion is often reduced due to pain. Tenderness is present over the affected tendon. Cause: Extensor tendonitis is often caused by injury, particularly sports injuries, or overuse. Tendonitis can often be caused by inadequate stretching prior to exercise, or increasing an exercise program too rapidly.