Rooksdown Practice Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Copy of 120611 Southampton Hampshire and Portsmouth PCT GP Practices and Clinical Systems
Jcode Practice Name Main or Building Name House and Road Locality Town Postcode Clinical System Branch J82145 Abbey Mead Surgery Main The Abbey Romsey SO51 8EN INPS Vision Y02838 Adelaide GP Surgery The Adelaide health Centre William Macleod Way Southampton SO16 4XE TPP SystmOne J82053 Adelaide Medical Centre Main Adelaide Road Andover SP10 1HA INPS Vision J82131001 Alderholt Surgery (branch of Fordingbridge) Branch 12 PARK LANE ALDERHOLT FORDINGBRIDGE SP6 3AJ TPP SystmOne J82092 Aldermoor Health Centre Aldermoor Close Lordswood Southampton SO165ST EMIS LV J82120 Alexander House Main 2 Salisbury Road Farnborough GU14 7AW EMIS LV J82122 Alma Medical Centre 68-70 Alma Road Portswood Southampton SO146UX TPP SystmOne J82074 Alma Road Surgery Main Alma Road Romsey SO51 8ED iSOFT Synergy J82124 Alresford Surgery Main Station Road Alresford SO24 9JL Emis Web J82017 Andover Health Centre Medical Practice Main Charlton Road Andover SP10 3LD EMIS PCS J82007 Arnewood Practice Main Milton Medical Centre Avenue Road New Milton BH25 5JP TPP SystmOne J82115 Atherley House Surgery* 143-145 Shirley Road Shirley Southampton SO153FH TPP SystmOne J82130001 Badger Farm Surgery Branch Badger Farm Road Winchester SO22 4QB INPS Vision J82042 Badgerswood Surgery Main Badgerwood Surgery Mill Lane Headley Bordon GU35 8LH EMIS LV J82091 Baffins Surgery* St Cuthbert's Church Hayling Avenue Portsmouth PO3 6BH EMIS LV J82631 Bargate Medical Centre 1 Spa Road Southampton Southampton SO14 2EG TPP SystmOne J82166 Barton Surgery Main 1 Edmunds Close Barton Court AvenueBarton-On-Sea -
The Beggarwood Surgery Newapproachcomprehensive Report
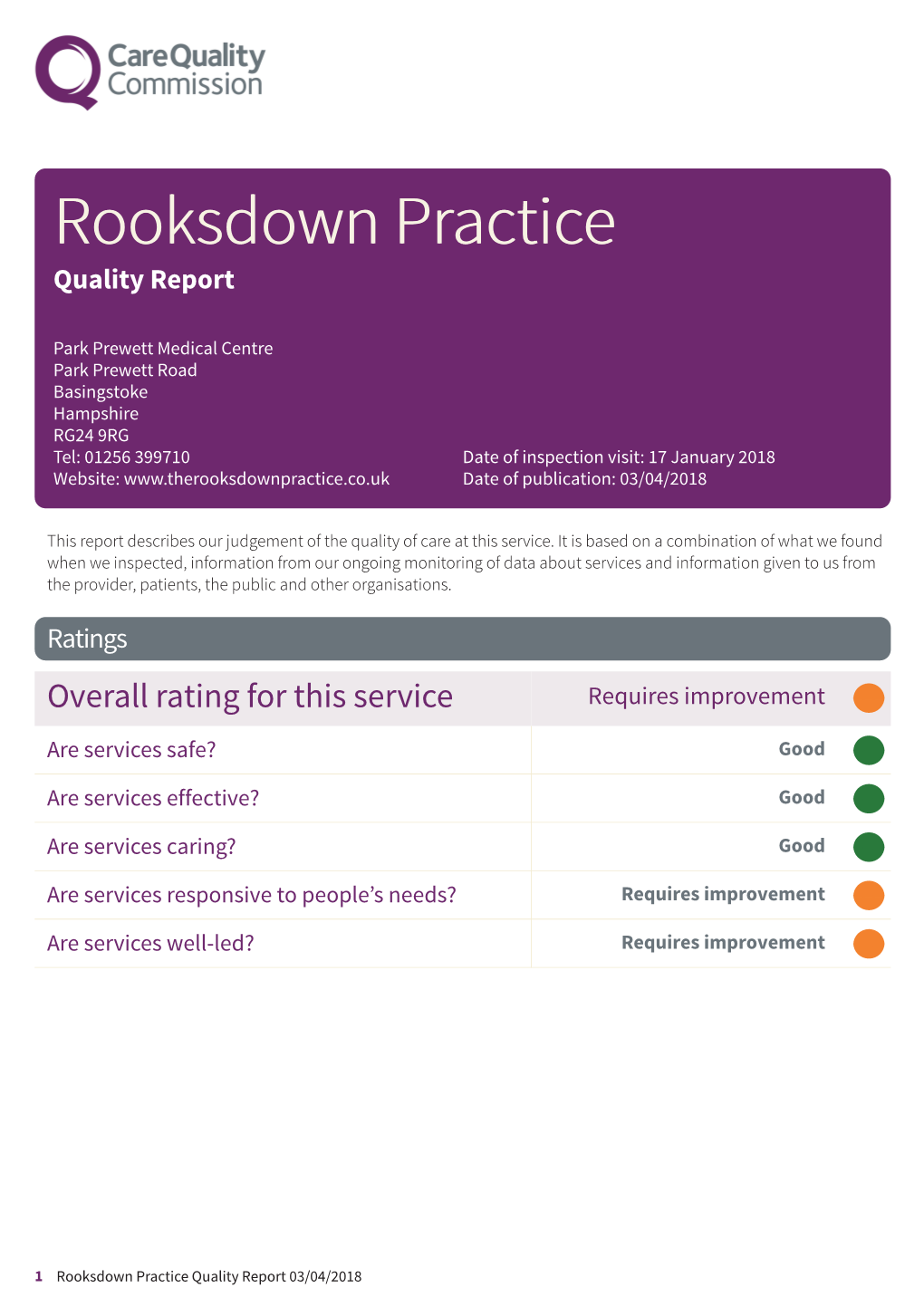
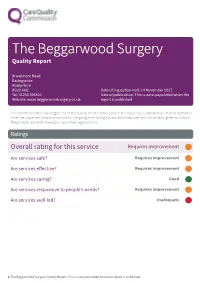
The Beggarwood Surgery Quality Report Broadmere Road Basingstoke Hampshire RG22 4AQ Date of inspection visit: 14 November 2017 Tel: 01256 396500 Date of publication: This is auto-populated when the Website: www.beggarwoodsurgery.co.uk report is published This report describes our judgement of the quality of care at this service. It is based on a combination of what we found when we inspected, information from our ongoing monitoring of data about services and information given to us from the provider, patients, the public and other organisations. Ratings Overall rating for this service Requires improvement ––– Are services safe? Requires improvement ––– Are services effective? Requires improvement ––– Are services caring? Good ––– Are services responsive to people’s needs? Requires improvement ––– Are services well-led? Inadequate ––– 1 The Beggarwood Surgery Quality Report This is auto-populated when the report is published Summary of findings Contents Summary of this inspection Page Overall summary 2 Detailed findings from this inspection Our inspection team 4 Background to The Beggarwood Surgery 4 Detailed findings 5 Action we have told the provider to take 22 Overall summary Letter from the Chief Inspector of General • People whose circumstances may make them Practice vulnerable – Requires improvement At our previous inspection in February 2017 we • People experiencing poor mental health (including found the practice to be inadequate overall. people with dementia) - Requires improvement Following this inspection on 14 November 2017 we Previously we undertook a follow up comprehensive rated the practice as requires improvement overall. inspection of The Beggarwood Surgery on 28 February The key questions are rated as: 2017 under Section 60 of the Health and Social Care Act 2008 as part of our regulatory functions. -

Vebraalto.Com
Belvoir Basingstoke Sales 10 New Street, Basingstoke, Hampshire, RG21 7DE Broadmere Road,Beggarwood, Hampshire RG22 4FP Offers In Excess Of £170,000 Leasehold Call: 01256 811220 belvoir.co.uk Belvoir Basingstoke Sales 10 New Street, Basingstoke, Hampshire, RG21 7DE *LONG LEASE WITH OVER 130 YEARS REMAINING* BELVOIR! ESTATE AGENTS are pleased to offer to the market this recently decorated, modern one bedroom apartment, which would make an ideal first time or investment purchase. Located on the second floor the property comprises a traditional entrance hallway with sensor light and intercom entry system, a dual aspect lounge which benefits from two Juliet balcony's, a fitted kitchen, fitted bathroom and a generous master bedroom with his and hers fitted wardrobes. Further benefits include double glazing, recently replaced electric heating, recently replaced carpets, large loft area for storage, communal bike and bin stores, allocated parking and access to further visitor parking spaces ESTIMATED RENTAL VALUE: The estimated rental income would be in the region of £725 pcm LOCATION: Situated in the Beggarwood area of Basingstoke the property offers easy access to many local amenities including Beggarwood nature reserve, schools, Sainsburys supermarket and Hatch Warren retail park. The area also offers easy access to M3 junction 7 and has a regular bus service into Basingstoke Town Centre where you can find the main line railway station which has a fast train to London-Waterloo taking approximately 45 minutes TENURE: Leasehold LOCAL AUTHORITY: Basingstoke and Deane Borough Council VIEWING DETAILS: Viewings are strictly by appointment only. Please contact Belvoir Estate Agents Call: 01256 811220 belvoir.co.uk Belvoir Basingstoke Sales 10 New Street, Basingstoke, Hampshire, RG21 7DE These particulars are intended as a guide and act as information only. -

The Regular Features Plus and Much More Hatch Warren, Beggarwood and Kempshott Park
RaTHE bbiter Issue 280 July/August 2021 RaTHE bbiter All the regular features plus • BEGGARWOOD SURGERY PPG • ARTWELL PROJECTS • NEW YOUTH WEBSITE and much more The Community Newsletter for Hatch Warren, Beggarwood and Kempshott Park /RRNLQJIRUDWUXVWHG ORFDOEXVLQHVVIRU\RXU QH[WKRPHSURMHFW" :LQGRZV 'RRUV &RQVHUYDWRULHV 2UDQJHULHV *DUDJH'RRUV *XDUDQWHHG:RUN *UHDW3ULFHV )LQDQFH$YDLODEOH &DOOULSWRQZLQGRZVFRXN LQ J V W R D V N H % ï ï ï ï ï :K\QRWYLVLWRXUVKRZURRPLQ&KLQHKDP" ï ï ï :HKDYHORWVRIH[DPSOHFRQVHUYDWRULHVZLQGRZVDQG GRRUVZLWKIUHHSDUNLQJDQGDGHFHQWFXSSD 4XRWHç5$%%,7(5èIRUDSUHIHUHQWLDOTXRWH Printed on recycled or sustainably sourced paper using ecoprint-system4 by Greenhouse Graphics. Hampshire’s only EMAS accredited print center. 5DEELWHU$GYHUW5LSWRQ:LQGRZVLQGG The Rabbiter - July/August 2021 THE EDITORIAL Here comes summer! Our gardens are blooming – I’ve had the best display of roses Rabbiter this year and there are bumper crops coming from the allotment. Many of us have had INSIDE THIS ISSUE more time for our outside spaces and the recent sunshine has certainly encouraged 5 MENTALTHE HEALTH AWARENESS us to ‘dibble and hoe’. Trips to the Garden Centre for a little retail therapy plus tea BRIGHTON HILL and cake outside have been enjoyed by many. Keep gardening everyone as next year Rabbiter COMMUNITY SCHOOL the Rabbiter are hoping to hold a Best Front Garden competition. WHAT NEXT GROUP As many of you will now be aware, Rev May has now moved to another church and 6 PHILLIPS SOLICITORS our Parish is going to merge with Kempshott. This will not change the Church status of St Mark’s school or stop services being held at Immanuel – see page 19 for more 8 COUNCILLOR’S UPDATE information. -

Hampshire Bus, Train and Ferry Guide 2014-2015
I I I I NDEX F LACES ERVED I I O P S To Newbury To Newbury To Tilehurst To Reading To Reading, To Reading To Wokingham I To Windsor I I Oxford and I and Reading I Bracknell 103 I Abbotts Ann. D3 Fyfield . D2 ABC D E F G H JI K Portsmouth & Southsea a . G8 the NorthI Three Mile I X2 I Adanac Park . D6 Wash Comon The Link I 194 Portsmouth Harbour a. G8 I Cross I Alderbury. B4 Glendene Caravan Park, Bashley . C8 104 2A I I Poulner . B7 Burghfield 2 I 72 I Alderholt . .A . A6 Godshill . B6 I I Pound Green . G1 Common I Aldermaston . G1 Godwinscroft . B8 u I 7 BERKSHIRE I 82 I Privett, Gosport . F8 103 Greenham I Aldershot a . K3 Golden Pot Inn . H3 I Inkpen 7 21 22 The Link Brimpton I Purbrook . G7 Ball Hill Aldermaston I I Allbrook . E5 Golf Course, Nr Alton . H3 Common I Beacon Crookham I PUBLIC TRANSPORT MAP OF I I h Allington . C3 Goodworth Clatford . D3 Wash 2 I t I I 194 a Alton a . H4 Gosport . G8 Quarley . D3 104 I 22 I P Water I 103 Spencers Wood I s Queen Alexander Hospital,Cosham. G7 2A I Great Hollands e Alton Hospital and Sports Centre . H4 Grange Park. F6 24 I I tl 21 The Link Bishopswood I a I s Amesbury . B3 Grateley . D3 Quetta Park . J3 7u Bishop’s Green I G X2 I a 21 22A I Broadlaying 23 Road Shops X2 I 194 C Ampfield . -

Farleigh Wallop
point your feet on a new path Farleigh Wallop Distance: 14½ km=9 miles or 13 km=8 miles easy walking Region: Hampshire Date written: 2-apr-2016 Author: Cascarrabias Refreshments: Ellisfield Map: Explorer 144 (Basingstoke) but the maps in this guide should be sufficient Problems, changes? We depend on your feedback: [email protected] Public rights are restricted to printing, copying or distributing this document exactly as seen here, complete and without any cutting or editing. See Principles on main webpage. Village, isolated church, valley trail, views, woodland In Brief This is a walk through typical Hampshire countryside, with several surprises, beginning at the very start of the walk. The terrain varies from a beautiful long surfaced path in the valley, to a driveway through parkland, a forest trail and an old trackway. Views change constantly. There are no nettles or undergrowth on this walk. Boots are recommended because of mud in the wood and one very stony path. This walk would be fine for your dog too. The walk begins at St Andrews Church, Farleigh Wallop , near Basing- stoke, Hampshire, postcode RG25 2HH . The church stands in a field in splendid isolation from its home village. The approach is along a narrow lane and the “parking area” is a dirt space with room for about six cars at a pinch. A service is held here only every fifth Sunday at 11am and on all other occasions you should find the space all but empty. The roster starts at Easter, so if Easter Sunday was, for example, on the 27 th March, there will be a service on 1 st May, 5 th June, 10 th July, 14 th Aug, 18 th Sep, 23 rd Oct and you should not park there on those days for the sake of the parish- ioners. -

The Regular Features Plus and Much More Hatch Warren, Beggarwood and Kempshott Park
RaTHE bbiter The Rabbiter - June 2016 RaTHE bbiter Issue 232 June 2016 All the regular features plus • DIGESTER UPDATE • BEAVERS, CUBS AND SCOUTS • HATCH WARREN SUMMER FESTIVAL and much more The Community Newsletter for Hatch Warren, Beggarwood and Kempshott Park 1 The Rabbiter - June 2016 All Seasons Window Cleaning Reliably serving the Hatchwarren / Beggarwood community for over 20 years Additional services include: • Driveway cleaning • • Cladding/signage cleaning • • Gutter/fascia/soffit cleaning • • Conservatory roof cleaning • • Pure water - no chemicals • Call STEVE on 01256 353727 Email: [email protected] Web: www.allseasonswindowcleaning.com www.facebook.com/allseasonswindowcleaninguk Printed on recycled or sustainably sourced paper using ecoprint-system4 by Greenhouse Graphics. Hampshire’s only EMAS accredited print center. THE EDITORIAL The first Rabbiter was published in August 1992 to mark the opening of the Hatch Warren Rabbiter Community Centre and to publicise the Grand Opening Event and Ceilidh which were INSIDE THIS ISSUE held on 5 September. There was bunting, food, games in the afternoon and I remember THE dancing the night away to a wonderful folk band in the evening. On 9 July there is going to 4 HATCH WARREN NATURE GROUP be a grand Summer Festival on the Hatch Warren Playing Fields with lots of exciting events OLD DOWN AND BEGGARWOOD including the arrival of a Chinook helicopter! It is going to be a wonderful day so please Ra WILDLIFEbbi GROUP ter make sure you have the date in your diary. 5 ANAEROBIC DIGESTER Another important local event is the Hatch Warren Community Association AGM which HATCH WARREN W.I. will be held on 8 June at 7.30pm. -

Local Government Commission for England A0 CUST POR with the Permission of the Controller of Her Majesty's Stationery Office, © Crown Copyright
D A O R N O Monk Sherborne Wood IX CALLEVAD WARD E Monk SHERFIELD ON LOCAL GOVERNMENT COMMISSIONAN FOR ENGLAND L LN Sherborne BRAMLEY CP KI LODDON CP Kiln Green Monk Sherborne A House 3 4 Lower Farm 0 SHERBORNE ST JOHN WARD TAYLORS FARM PARISH WARD D D Queen's A A O O R House R E N Cowdry Fieldgate Y E V House R O Razor's Farm M N A H Collett's Copse PERIODIC ELECTORAL REVIEW OF BASINGSTOKE AND DEANE Long Swains Row Petty's Copse E CL YM Rookery Weybrook TH Sherfield Hall Farm Farm W F e E y N Br N oo E k Hampshire International L A J Business Park C A D C u X Final Recommendations for Ward Boundaries in Basingstoke f L N a E C u L T d S e E Thames Dale L T W a H n O Little R July 2000 e NH Baker's IL SAFFRON CL L All Saints' Sherborne St John Kestrel Court Martin's Bushes Copse Church Grub Close Plantation W Manor AY Farm The Grange WAY Crane's D A (Nursing Home) O Farm R M N PE A TT W Y'S B R ROOK E O RD D N L N L Y ' IE V S Marl's Copse E F R C S SHERBORNEBob's ST Farm JOHN CP L RA NE A NE A N B S R E O Chapel R C W D M S A P Cemetery Chute N R R I Recreation Ground O N A Guinea Copse G C D R Church A Chalk Pit OOK P N MAYBR Spier's Copse Four Acre Piece e E t C Russell's ty L S Five Acre Piece 's O Copse B S r E School Y o A R o R k D D D W A E W O Five Acre E E R I 3 R Plantation V 3 T N Upper Parrott's Copse Seven A O E M T D Acre Piece M R S I A L A A R Basing Forest F C K M RA R NE Allot E S Gdns L D Chineham School A L N A R Inner Maynard's Maynard's and MONK SHERBORNE CP O E Business AD Copse Piece Community Centre Allot Park -

2018 - Easter Bank Holiday; Pharmacy Cover - NHS England (Wessex)
2018 - Easter Bank Holiday; Pharmacy Cover - NHS England (Wessex) Good Friday - Easter Monday - Easter Sunday - ODS Code Pharmacy Name Address 1 Address 2 Town County Postcode Friday 30 March Monday 02 April Sunday 01 April 2018 2018 2018 09:00 - 17:30 Closed 10:00 - 16:00 FD490 Boots The Chemists 52 High Street Alton Hampshire GU34 1ET Closed 13:00 - 15:00 Closed FDC67 Anstey Road Pharmacy Alton Health Centre Anstey Road Alton Hampshire GU34 2QX Your Local Boots Chawton Park Closed Closed Closed FQM29 Pharmacy Surgery Chawton Park Road Alton Hampshire GU34 1RJ Closed Closed Closed FYX99 Lloyds Pharmacy 68 High Street Alton Hampshire GU34 1ET Boots The Chemists Chineham District 09:00 - 18:00 Closed 09:00 - 18:00 FAW77 Boots Ltd Centre Basingstoke Hampshire RG24 8BQ 09:00 - 18:00 09:00 - 18:00 09:00 - 18:00 FCC36 Lloyds Pharmacy 34 Guinea Court Chineham North Basingstoke Hampshire RG24 8XJ Closed Closed Closed FCL84 Cohens Chemist Essex House Essex Road Basingstoke Hampshire RG21 8SU Closed Closed Closed FEX31 Overton Pharmacy 4 Winchester Street Overton Basingstoke Hampshire RG25 3HS 3, Winklebury Closed Closed Closed FFF85 Pharmacy Link Centre Winklebury Way Basingstoke Hampshire RG23 8BU The New Medical Shakespeare Road, Closed Closed Closed FH259 Lloyds Pharmacy Centre Popley Basingstoke Hampshire RG24 9DT 09:00 - 18:00 Closed 10:00 - 16:00 FHA97 Boots The Chemists 15 Old Basing Mall Basingstoke Hampshire RG21 7LW Closed Closed Closed FHE37 Rooksdown Pharmacy Park Prewett Road Basingstoke Hampshire RG24 9RG 4 Kings Furlong Closed -

Farnham Ramblers Car Park Database 20210629.Xlsx Page 1 of 17 Grid Ref 6 Figure Explorer Nearest Post Code Location and Directions Other Info E.G
Grid Ref 6 Figure Explorer Nearest Post Code Location and Directions Other Info e.g. Size if < 20 cars; for 10km Grid Ref Map Post Code to Car Park Contact Person; Charge or only square Distance m suitable on some days of week SU53 SU 585 361 132 SO24 9DT 866 Abbotstone Down off B3046 north out of Old Alresford Restricted < 15. Overflow on other side of road TQ14 TQ 132 456 146 RH5 6JY 271 Abinger Common Broadmoor Hill CP, Sheephouse Lane, a single track road with passing places TQ14 TQ 111 480 146 RH5 6BF 261 Abinger Roughs NT CP TQ26 TQ 207 609 161 KT19 8LF 685 Across the road from Epsom Station. TQ04 TQ 059 470 145 GU5 9DA 323 Albury Cricket Ground corner of New and Park Roads TQ04 TQ 049 479 145 GU5 9AB 32 Albury Drummond Arms Permission Required TQ04 TQ 061 467 145 GU5 9DD 220 Albury Heath car park SU66 SU 603 672 159 RG7 4JS 42 Aldermarston Wharf SU85 SU 888 538 145 GU12 5PT 182 Aldershot Carrington rec ground (Behind North Camp station) SU85 SU 850 503 145 GU11 3NS 39 Aldershot Heath (Lay-by opposite garage on A325 between Cranmore Lane and Pavilion Rd.) SU85 SU 874 535 145 GU14 6EF 72 Aldershot North Camp Napier car park SU84 SU 878 491 145 GU12 4BP 95 Aldershot Park CP. Turn into Guildford Rd Off B3208 Lower Farnham Rd. CP is at far end on left SU84 SU 811 411 145 GU10 4HA 390 Alice Holt Forest Abbotswood Inclosure Restricted SU84 SU 803 434 145 GU10 4LQ 536 Alice Holt Gravel Hill CP SU84 SU 813 418 145 GU10 4LS 295 Alice Holt Visitors Centre Charge SU53 SU 585 326 132 SO24 9BW 49 Alresford Community CP SU53 SU 582 316 132 SO24 9LW 32 Alresford The Cricketers pub CP SU74 SU 737 410 144 GU34 4HG 27 Alton (White Hart Pub use car park if eating otherwise use road) SU73 SU 724 395 133 GU34 2SZ 13 Alton : Kings Pond CP. -

8 Bus Time Schedule & Line Route
8 bus time schedule & line map 8 Town Centre - Kempshott Park View In Website Mode The 8 bus line (Town Centre - Kempshott Park) has 2 routes. For regular weekdays, their operation hours are: (1) Basingstoke: 5:20 AM - 11:25 PM (2) Hatch Warren: 5:31 AM - 11:10 PM Use the Moovit App to ƒnd the closest 8 bus station near you and ƒnd out when is the next 8 bus arriving. Direction: Basingstoke 8 bus Time Schedule 38 stops Basingstoke Route Timetable: VIEW LINE SCHEDULE Sunday 8:24 AM - 8:53 PM Monday 5:20 AM - 11:25 PM Magnus Drive, Hatch Warren Octavian Close, Basingstoke Tuesday 5:20 AM - 11:25 PM Alderney Avenue, Hatch Warren Wednesday 5:20 AM - 11:25 PM Solent Drive, Basingstoke Thursday 5:20 AM - 11:25 PM Centurion Way, Hatch Warren Friday 5:20 AM - 11:25 PM Petworth Close, Basingstoke Saturday 6:33 AM - 11:25 PM St Mark's Primary School, Hatch Warren Inglewood Drive, Hatch Warren The Cornƒelds, Hatch Warren 8 bus Info Danebury Road, Basingstoke Direction: Basingstoke Stops: 38 Whitestones, Hatch Warren Trip Duration: 31 min Danebury Road, Basingstoke Line Summary: Magnus Drive, Hatch Warren, Alderney Avenue, Hatch Warren, Centurion Way, Highdowns, Hatch Warren Hatch Warren, St Mark's Primary School, Hatch Warren, Inglewood Drive, Hatch Warren, The Belmont Heights, Hatch Warren Cornƒelds, Hatch Warren, Whitestones, Hatch Belmont Heights, Basingstoke Warren, Highdowns, Hatch Warren, Belmont Heights, Hatch Warren, Garlic Lane, Kempshott Park, Garlic Lane, Kempshott Park Wedderburn Avenue, Kempshott Park, Priestdown, Grosvenor Close, Basingstoke -

Service Town Centre - Kempshott Park 12 Monday - Friday (Not Bank Holidays)
Service Town Centre - Kempshott Park 12 Monday - Friday (not Bank Holidays) Operated by: HBC Stagecoach in Hampshire Timetable valid from 4 Apr 2021 until further notice Service: 12 12 12 12 12 12 12 12 12 12 Notes: Prd1 XPrd2 Prd3 XPrd4 Operator: HBC HBC HBC HBC HBC HBC HBC HBC HBC HBC Basingstoke, Bus Station (Stop F) Depart: 07:05 08:17 08:23 09:10 10:10 11:10 12:10 12:10 13:10 14:10 Basingstoke, Queen Marys College .... 08:25 .... .... .... .... .... .... .... .... Cranbourne, Stratton Road Arrive: .... 08:33 08:33 .... .... .... .... .... .... .... Cranbourne, Morley Road 07:13 .... .... 09:18 10:18 11:18 12:18 12:18 13:18 14:18 Brighton Hill, Brighton Hill Centre 07:18 .... .... 09:23 10:23 11:23 12:23 12:23 13:23 14:23 Brighton Hill, Heathfield 07:22 .... .... 09:27 10:27 11:27 12:27 12:27 13:27 14:27 Hatch Warren, Community Centre 07:26 .... .... 09:33 10:33 11:33 12:33 12:33 13:33 14:33 Hatch Warren, Sainsburys .... .... .... .... .... .... .... .... .... .... Kempshott Park, Broadmere Road .... .... .... .... .... .... .... .... .... .... Hatch Warren, Long Cross Lane Arrive: .... .... .... .... .... .... .... .... .... .... Service: 12 12 12 12 12 Notes: Operator: HBC HBC HBC HBC HBC Basingstoke, Bus Station (Stop F) Depart: 15:10 16:10 17:15 18:15 19:15 Basingstoke, Queen Marys College .... .... .... .... .... Cranbourne, Stratton Road Arrive: .... .... .... .... .... Cranbourne, Morley Road 15:18 16:18 17:23 18:23 19:23 Brighton Hill, Brighton Hill Centre 15:23 16:23 17:28 18:28 19:28 Brighton Hill, Heathfield 15:27 16:27 17:32 18:32 19:32 Hatch Warren, Community Centre 15:33 16:33 17:38 18:38 19:37 Hatch Warren, Sainsburys ...