Hypermagnesemia Is Associated with All-Cause Mortality in Patients With
Total Page:16
File Type:pdf, Size:1020Kb
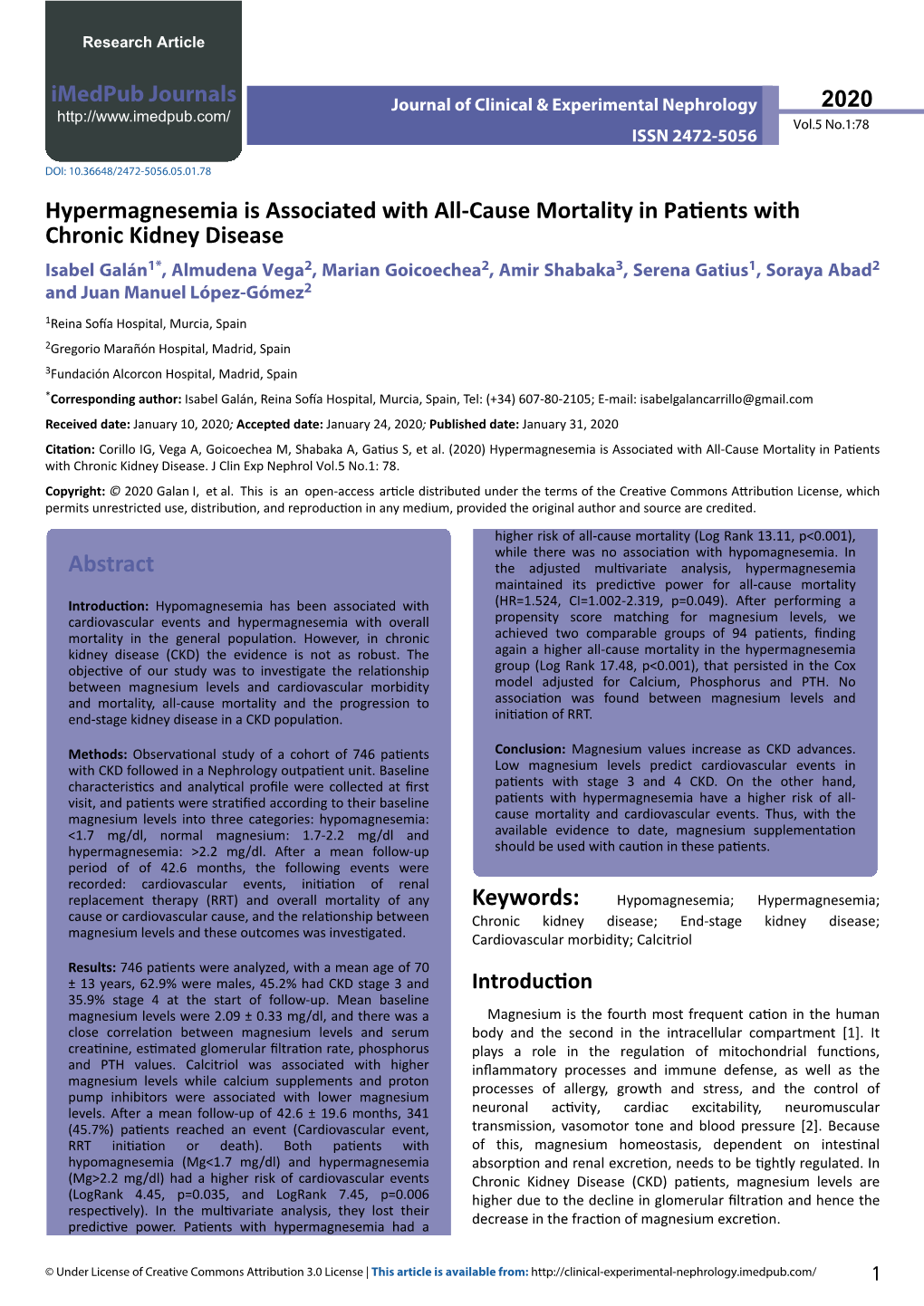
Load more
Recommended publications
-

Dysmagnesemia in Covid-19 Cohort Patients: Prevalence and Associated Factors
Magnesium Research 2020; 33 (4): 114-122 ORIGINAL ARTICLE Dysmagnesemia in Covid-19 cohort patients: prevalence and associated factors Didier Quilliot1, Olivier Bonsack1, Roland Jaussaud2, Andre´ Mazur3 1 Transversal Nutrition Unit and; 2 Internal Medicine and Clinical Immunology. Nancy University Hospital, University of Lorraine, France; 3 Universite´ Clermont Auvergne, INRAE, UNH, Unite´ de Nutrition Humaine, Clermont-Ferrand, France Correspondence <[email protected]> Abstract. Hypomagnesemia and hypermagnesemia could have serious implications and possibly lead to progress from a mild form to a severe outcome of Covid-19. Susceptibility of subjects with low magnesium status to develop and enhance this infection is possible. There is little data on the magnesium status of patients with Covid-19 with different degrees of severity. This study was conducted to evaluate prevalence of dysmagnesemia in a prospective Covid-19 cohort study according to the severity of the clinical manifestations and to identify factors associated. Serum magnesium was measured in 300 of 549 patients admitted to the hospital due to severe Covid-19. According to the WHO guidelines, patients were classified as moderate, severe, or critical. 48% patients had a magnesemia below 0.75 mmol/L (defined as magnesium deficiency) including 13% with a marked hypomagnesemia (<0.65 mmol/L). 9.6% had values equal to or higher than 0.95 mmol/L. Serum magnesium concentrations were significantly lower in female than in male (0.73 Æ 0.12 vs 0.80 Æ 0.13 mmol/L), whereas the sex ratio M/F was higher in severe and critical form (p<0.001). In a bivariate analysis, the risk of magnesium deficiency was significantly and negatively associated with infection severity (p<0.001), sex ratio (M/F, p<0.001), oxygenotherapy (p<0.001), stay in critical care unit (p=0.028), and positively with nephropathy (p=0.026). -

Assessment Report
17 September 2020 EMA/522604/2020 Corr.1 Committee for Medicinal Products for Human Use (CHMP) Assessment report Velphoro Common name: sucroferric oxyhydroxide Procedure No. EMEA/H/C/002705/X/0020/G Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us An agency of the European Union Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 6 1.1. Submission of the dossier ...................................................................................... 6 1.2. Steps taken for the assessment of the product ......................................................... 7 2. Scientific discussion ................................................................................ 8 2.1. Problem statement ............................................................................................... 8 2.1.1. Disease or condition ........................................................................................... 8 2.1.2. Epidemiology and risk factors, screening tools/prevention ...................................... 8 2.1.3. Biologic features ............................................................................................... -

Increased Mortality Associated with Hypermagnesemia in Severe COVID-19 Illness
Original Investigation Increased Mortality Associated with Hypermagnesemia in Severe COVID-19 Illness Jacob S. Stevens 1,2, Andrew A. Moses1, Thomas L. Nickolas1,2, Syed Ali Husain1,2, and Sumit Mohan1,2,3 Key Points Hypermagnesemia is common in patients admitted with coronavirus disease 2019. The development of hypermagnesemia in coronavirus disease 2019 is associated with renal failure and markers of high cell turnover. In adjusted models, patients who develop hypermagnesemia have an increased risk of mortality. Abstract Background Although electrolyte abnormalities are common among patients with COVID-19, very little has been reported on magnesium homeostasis in these patients. Here we report the incidence of hypermagnesemia, and its association with outcomes among patients admitted with COVID-19. Methods We retrospectively identified all patients with a positive test result for SARS-CoV-2who were admitted to a large quaternary care center in New York City in spring 2020. Details of the patients’ demographics and hospital course were obtained retrospectively from medical records. Patients were defined as having hypermagnesemia if their median magnesium over the course of their hospitalization was .2.4 mg/dl. Results A total of 1685 patients hospitalized with COVID-19 had their magnesium levels checked during their hospitalization, and were included in the final study cohort, among whom 355 (21%) had hypermagnesemia. Patients who were hypermagnesemic had a higher incidence of shock requiring pressors (35% vs 27%, P,0.01), respiratory failure requiring mechanical ventilation (28% vs 21%, P50.01), AKI (65% vs 50%, P,0.001), and AKI severe enough to require renal replacement therapy (18% vs 5%, P,0.001). -
Early-Onset Neonatal Hyperkalemia Associated with Maternal
Tanaka et al. BMC Pediatrics (2018) 18:55 https://doi.org/10.1186/s12887-018-1048-4 CASEREPORT Open Access Early-onset neonatal hyperkalemia associated with maternal hypermagnesemia: a case report Kenichi Tanaka1, Hiroko Mori1, Rieko Sakamoto2, Shirou Matsumoto2, Hiroshi Mitsubuchi1, Kimitoshi Nakamura2 and Masanori Iwai1* Abstract Background: Neonatal nonoliguric hyperkalemia (NOHK) is a metabolic abnormality that occurs in extremely premature neonates at approximately 24 h after birth and is mainly due to the immature functioning of the sodium (Na+)/potassium (K+) pump. Magnesium sulfate is frequently used in obstetrical practice to prevent preterm labor and to treat preeclampsia; this medication can also cause hypermagnesemia and hyperkalemia by a mechanism that is different from that of NOHK. Herein, we report the first case of very early-onset neonatal hyperkalemia induced by maternal hypermagnesemia. Case presentation: A neonate born at 32 weeks of gestation developed hyperkalemia (K+ 6.4 mmol/L) 2 h after birth. The neonate’s blood potassium concentration reached 7.0 mmol/L 4 h after birth, despite good urine output. The neonate and his mother had severe hypermagnesemia caused by intravenous infusion of magnesium sulfate given for tocolysis due to pre-term labor. Conclusion: The early-onset hyperkalemia may have been caused by the accumulation of potassium ions transported through the placenta, the shift of potassium ions from the intracellular to the extracellular space in the infant due to the malfunctioning of the Na+/K+ pump and the inhibition of renal distal tube potassium ion secretion, there is a possibility that these mechanisms were induced by maternal and fetal hypermagnesemia after maternal magnesium sulfate administration. -

Supermicar Data Entry Instructions, 2007 363 Pp. Pdf Icon[PDF
SUPERMICAR TABLE OF CONTENTS Chapter I - Introduction to SuperMICAR ........................................... 1 A. History and Background .............................................. 1 Chapter II – The Death Certificate ..................................................... 3 Exercise 1 – Reading Death Certificate ........................... 7 Chapter III Basic Data Entry Instructions ....................................... 12 A. Creating a SuperMICAR File ....................................... 14 B. Entering and Saving Certificate Data........................... 18 C. Adding Certificates using SuperMICAR....................... 19 1. Opening a file........................................................ 19 2. Certificate.............................................................. 19 3. Sex........................................................................ 20 4. Date of Death........................................................ 20 5. Age: Number of Units ........................................... 20 6. Age: Unit............................................................... 20 7. Part I, Cause of Death .......................................... 21 8. Duration ................................................................ 22 9. Part II, Cause of Death ......................................... 22 10. Was Autopsy Performed....................................... 23 11. Were Autopsy Findings Available ......................... 23 12. Tobacco................................................................ 24 13. Pregnancy............................................................ -

Clinical Characteristics of Tumor Lysis Syndrome in Childhood Acute Lymphoblastic Leukemia
www.nature.com/scientificreports OPEN Clinical characteristics of tumor lysis syndrome in childhood acute lymphoblastic leukemia Yao Xue1,2,22, Jing Chen3,22, Siyuan Gao1,2, Xiaowen Zhai5, Ningling Wang6, Ju Gao7, Yu Lv8, Mengmeng Yin9, Yong Zhuang10, Hui Zhang11, Xiaofan Zhu12, Xuedong Wu13, Chi Kong Li14, Shaoyan Hu15, Changda Liang16, Runming Jin17, Hui Jiang18, Minghua Yang19, Lirong Sun20, Kaili Pan21, Jiaoyang Cai3, Jingyan Tang3, Xianmin Guan4* & Yongjun Fang1,2* Tumor lysis syndrome (TLS) is a common and fatal complication of childhood hematologic malignancies, especially acute lymphoblastic leukemia (ALL). The clinical features, therapeutic regimens, and outcomes of TLS have not been comprehensively analyzed in Chinese children with ALL. A total of 5537 children with ALL were recruited from the Chinese Children’s Cancer Group, including 79 diagnosed with TLS. The clinical characteristics, treatment regimens, and survival of TLS patients were analyzed. Age distribution of children with TLS was remarkably diferent from those without TLS. White blood cells (WBC) count ≥ 50 × 109/L was associated with a higher risk of TLS [odds ratio (OR) = 2.6, 95% CI = 1.6–4.5]. The incidence of T-ALL in TLS children was signifcantly higher than that in non-TLS controls (OR = 4.7, 95% CI = 2.6–8.8). Hyperphosphatemia and hypocalcemia were more common in TLS children with hyperleukocytosis (OR = 2.6, 95% CI = 1.0–6.9 and OR = 5.4, 95% CI = 2.0–14.2, respectively). Signifcant diferences in levels of potassium (P = 0.004), calcium (P < 0.001), phosphorus (P < 0.001) and uric acid (P < 0.001) were observed between groups of TLS patients with and without increased creatinine. -

(October), 2005
VOL 46, NO 4, SUPPL 1, OCTOBER 2005 CONTENTS American Journal of AJKD Kidney Diseases K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Children With Chronic Kidney Disease Tables............................................................................................................................... S1 Figures ............................................................................................................................. S1 Acronyms and Abbreviations........................................................................................ S2 Algorithms ....................................................................................................................... S3 Work Group Members..................................................................................................... S4 K/DOQI Advisory Board Members................................................................................. S5 Foreword.......................................................................................................................... S6 Introduction ..................................................................................................................... S8 Guideline 1. Evaluation of Calcium and Phosphorus Metabolism ............................ S12 Guideline 2. Assessment of Bone Disease Associated with CKD................................ S18 Guideline 3. Surgical Management of Osteodystrophy ............................................. S23 Guideline 4. Target Serum Phosphorus Levels......................................................... -

Electrolyte Disorders and Arrhythmogenesis
Cardiology Journal 2011, Vol. 18, No. 3, pp. 233–245 Copyright © 2011 Via Medica REVIEW ARTICLE ISSN 1897–5593 Electrolyte disorders and arrhythmogenesis Nabil El-Sherif1, Gioia Turitto2 1State University of NY, Downstate Medical Center and NY Harbor VA Healthcare System, Brooklyn, NY, USA 2Methodist University Hospital, Brooklyn, NY, USA Abstract Electrolyte disorders can alter cardiac ionic currents kinetics and depending on the changes can promote proarrhythmic or antiarrhythmic effects. The present report reviews the mecha- nisms, electrophysiolgical (EP), electrocardiographic (ECG), and clinical consequences of elec- trolyte disorders. Potassium (K+) is the most abundent intracellular cation and hypokalemia is the most commont electrolyte abnormality encountered in clinical practice. The most signifcant ECG manifestation of hypokalemia is a prominent U wave. Several cardiac and + non cardiac drugs are known to suppress the HERG K channel and hence the IK, and especially in the presence of hypokalemia, can result in prolonged action potential duration and QT interval, QTU alternans, early afterdepolarizations, and torsade de pointes ventricu- lar tachyarrythmia (TdP VT). Hyperkalemia affects up to 8% of hospitalized patients mainly in the setting of compromised renal function. The ECG manifestation of hyperkalemia de- pends on serum K+ level. At 5.5–7.0 mmol/L K+, tall peaked, narrow-based T waves are seen. At > 10.0 mmol/L K+, sinus arrest, marked intraventricular conduction delay, ventricular techycardia, and ventricular fibrillation can develop. Isolated abnormalities of extracellular calcium (Ca++) produce clinically significant EP effects only when they are extreme in either direction. Hypocalcemia, frequently seen in the setting of chronic renal insufficiency, results in prolonged ST segment and QT interval while hypercalcemia, usually seen with hyperparathy- roidism, results in shortening of both intervals. -
Front Matter (PDF)
HIGH RATE OF SUCCESS IN AN NIH- STUDY of hypertensive patients- highest percentage - remained on itial therapy 83% with NORVASC#{174}(amlodipi besylate) after 4 years; nearly all pati were on the 5-mg starting dose’ LOW RATE DISCONTINUATION ONLY 1.5%of patients in placebo studies (n= 1730) discontinued due to adverse effects2 PROVEN No negative inotropic effects clinical doses in hemodyna m ic stud 2* No clinically significant effect on cardiac conduction or heart rate2 *S1IflH,jr fiernodynamic findings, hcvever fiave been agents possessing significant neqafive notropic ebecto and 10-mg tablets Once-Daily NORV (ambdipine EFFICACY AND SAFETY THAT’S EASY TO WITH Br$e(Summary NORVASC(amlodlpine besylate) Tablets For Oral Use CONTRAINDICATIONS: NORVASC is contraindicated in patients with known sensitivity to arniodipirre. In hypertension WARNINGS: Increased Angina and/or MyOcardIal Infarction: Rarely, patients, particulady those with severe obstruc5ve coronary artery disease, have developed documented increased frequency,durationand/or severity of angina or acute myocardial infarction on starhng cafrium channel blocker therapy or attire time of dosage increase. The mechanism of this effect has not been elucidated. PRECAUTIONS: General: Since the vasoditation induced by NORVASC is gradual in onset, acute hypotension has rarely been reported after oraladministrationof NORVASC. Nonethetuss, caution should be exercised when admin- or angina, convenient istering NORVASC as with any other penpherio vasodilator particularly in pahentswithsevere -
2012 CKD Guideline
OFFICIAL JOURNAL OF THE INTERNATIONAL SOCIETY OF NEPHROLOGY KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease VOLUME 3 | ISSUE 1 | JANUARY 2013 http://www.kidney-international.org KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease KDIGO gratefully acknowledges the following consortium of sponsors that make our initiatives possible: Abbott, Amgen, Bayer Schering Pharma, Belo Foundation, Bristol-Myers Squibb, Chugai Pharmaceutical, Coca-Cola Company, Dole Food Company, Fresenius Medical Care, Genzyme, Hoffmann-LaRoche, JC Penney, Kyowa Hakko Kirin, NATCO—The Organization for Transplant Professionals, NKF-Board of Directors, Novartis, Pharmacosmos, PUMC Pharmaceutical, Robert and Jane Cizik Foundation, Shire, Takeda Pharmaceutical, Transwestern Commercial Services, Vifor Pharma, and Wyeth. Sponsorship Statement: KDIGO is supported by a consortium of sponsors and no funding is accepted for the development of specific guidelines. http://www.kidney-international.org contents & 2013 KDIGO VOL 3 | ISSUE 1 | JANUARY (1) 2013 KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease v Tables and Figures vii KDIGO Board Members viii Reference Keys x CKD Nomenclature xi Conversion Factors & HbA1c Conversion xii Abbreviations and Acronyms 1 Notice 2 Foreword 3 Work Group Membership 4 Abstract 5 Summary of Recommendation Statements 15 Introduction: The case for updating and context 19 Chapter 1: Definition, and classification -

Women'shealthreport
Issue 4, 2014 Women’sHealthREPORT A QuaRTERLY PubLicatiON OF WOMEN’S HEALth diETEtic PRacticE GROup MICRONUTRIENTS AND THE OLDER ADULT – Part 1: Micronutrients of Importance to Older Adults By Vijaya Jain, MS, MSc, RD, CDN among older adults. A decreased energy intake associated with advancing age has important implications in terms of nutrient intake among older adults, including protein and micronutrients. Suboptimal intake for several micronutrients is prevalent among older adults. INTRODUCTION Increasing life expectancy has led to a steady rise in the number of older persons globally. In 2012, the number of older Americans aged 65 years and older had reached 43.1 million (1). As many of these older Americans continue to remain healthy and active well into their eighties and even nineties, and have better medi- cal management of chronic diseases and their comorbidities, the size of the older population is projected to double between 2000 and 2030 (2). According to the US Bureau of the Census, the size of the population age 85 and over is projected to be 7 Note from Chair: Collaboration is essential to the success of both million by 2020 (1). The baby-boomer generation will reach age individuals and organizations. It is has been a personal goal of mine 65 between 2010 and 2030, meaning that by 2030, one in five to see the Women’s Health DPG work with other DPGs and related American citizens will be older adults (1), and two out of every health organizations. In recent years, we have enhanced our mission three older Americans will have multiple chronic conditions (3). -
Rhode Island Chapter Abstracts
Rhode Island Chapter Abstracts April 1, 2015 Abdin, Ahmad Last Name: Abdin First Author: Resident First Name: Ahmad Category: Clinical Vignette PG Year: PGY-1 or MS Year: ACP Number: 2888549 Medical School or Residency Program: Warren Alpert Medical School of Brown University Hospital Affiliation: Memorial Hospital of Rhode Island, Providence VA Medical Center Additional Authors: Ahmad Abdin, MD, Mohammed Salhab, MD, Amos Charles, MD, Mazen Al-Qadi, MD Abstract Title: Amiodarone-Induced Cerebellar Dysfunction Abstract Text: Introduction: Amiodarone is a class III antiarrhythmic agent that is widely used to treat ventricular and supraventricular tachycardias. Several side-effects of the drug have been recognized including thyroid dysfunction, photosensitivity, hepatotoxicity, parenchymal lung disease, corneal deposits, and peripheral neuropathy. Cerebellar dysfunction is rarely seen in patients receiving amiodarone. We are reporting a rare case of amiodarone-induced cerebellar dysfunction that resolved completely upon discontinuation of the drug. Case Presentation: A 73-year-old man with a past medical history significant for paroxysmal atrial fibrillation, coronary artery disease, diabetes and hypertension who presented with worsening lower extremity weakness and unsteady gait with recurrent falls for the last 6 months. Two days prior to admission, his symptoms got worse and caused him to seek medical attention. Two years ago he was started and maintained on amiodarone 200 mg daily for rhythm control. On physical examination, vital signs were normal. A wide-based unsteady gait was noted. He had dysmetria bilaterally on finger-to-nose and heel-to-shin testing. The rapid alternating movements of the hands were irregular. The remainder of the general and neurologic examinations were unremarkable.