Complex II Inhibition by 3-NP Causes Mitochondrial Fragmentation and Neuronal Cell Death Via an NMDA- and ROS-Dependent Pathway
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Switch to Tonic Discharge by Thyrotropin-Releasing Hormone
Neuron Article Synchronized Network Oscillations in Rat Tuberoinfundibular Dopamine Neurons: Switch to Tonic Discharge by Thyrotropin-Releasing Hormone David J. Lyons,1,* Emilia Horjales-Araujo,1 and Christian Broberger1,* 1Department of Neuroscience, Karolinska Institutet, 171 77 Stockholm, Sweden *Correspondence: [email protected] (D.J.L.), [email protected] (C.B.) DOI 10.1016/j.neuron.2009.12.024 SUMMARY most common form of pituitary tumor (Burrow et al., 1981), and by the hyperprolactinaemia and sometimes galactorrhea that The pituitary hormone, prolactin, triggers lactation in is a side effect of antipsychotic drugs with DA antagonist prop- nursing mothers. Under nonlactating conditions, erties (Clemens et al., 1974; Meltzer and Fang, 1976). Yet, to prolactin secretion is suppressed by powerful inhibi- date, the cellular and network electrophysiological properties tion from hypothalamic tuberoinfundibular dopamine of the TIDA cell population have not been described. These (TIDA) neurons. Although firing pattern has been sug- factors are potentially fundamental features of prolactin regula- gested as integral to neuroendocrine control, the tion since discharge pattern may determine the functional output of neuroendocrine control of the anterior pituitary, as is observed electrical behavior of TIDA cells remains unknown. in the magnocellular system (Wakerley and Lincoln, 1973; Hatton We demonstrate that rat TIDA neurons discharge et al., 1983). Thus, the periodic bursting pattern in hypothalamic rhythmically in a robust 0.05 Hz oscillation. The oscil- gonadotropin-releasing hormone neurons is required for stimu- lation is phase locked between neurons, and while it lation of target gonadotrophs in the pituitary (Knobil, 1980). persists during chemical synaptic transmission When bursting is artificially replaced by continuous agonist stim- blockade, it is abolished by gap junction antagonists. -

Excitatory Amino Acid Receptor Antagonists and Electroacupuncture Synergetically Inhibit Carrageenan-Induced Behavioral Hyperalgesia and Spinal Fos Expression in Rats
http://www.paper.edu.cn Pain 99 (2002) 525–535 www.elsevier.com/locate/pain Excitatory amino acid receptor antagonists and electroacupuncture synergetically inhibit carrageenan-induced behavioral hyperalgesia and spinal fos expression in rats Yu-Qiu Zhanga, Guang-Chen Jib, Gen-Cheng Wub, Zhi-Qi Zhaoa,* aInstitute of Neurobiology, Fudan University, 220 Han Dan Road, Shanghai, 200433, China bState Key Laboratory of Medical Neurobiology, Medical Center of Fudan University, 138 Yi Xue Yuan Road, Shanghai, 200032, China Received 30 January 2002; accepted 27 June 2002 Abstract The interaction between electroacupuncture and an N-methyl-d-aspartic acid (NMDA) receptor antagonist, (DL-2-amino-5-phosphono- pentanoic acid; AP5), or an ( ^ )-a-Amino-3-hydroxy-5-methylisoxazole-4-propionic acid/kainite (AMPA/KA) receptor antagonist, (6,7- dinitroquinoxaline-2,3 (1H,4H); DNQX) administered intrathecally on carrageenan-induced thermal hyperalgesia and spinal c-Fos expres- sion was investigated. The latency of paw withdrawal (PWL) from a thermal stimulus was used as a measure of hyperalgesia in awake rats. Intrathecal (i.t.) injection of 1 and 10 nmol AP5, but not DNQX, markedly increased the PWL of the carrageenan-injected paw. At a dose of 100 nmol, either AP5 or DNQX significantly increased the PWL of carrageenan-injected paw, with AP5 being more potent. The PWLs of the non-injected and normal saline (NS)-injected paws were not detectably affected by the administration of NMDA or AMPA/KA receptor antagonists at the doses tested. Unilateral electroacupuncture stimulation of the ‘Zu-San-Li’ (St 36) and ‘Kun-Lun’ (UB 60) acupuncture points (60 and 2 Hz alternately, 1–2–3 mA) contralateral to the carrageenan-injected paw significantly elevated the PWLs of carrageenan- and NS-injected paws. -

Glutamate but Not Glycine Agonist Affinity for NMDA Receptors Is
The Journal of Neuroscience, April 1, 2002, 22(7):2550–2560 Glutamate But Not Glycine Agonist Affinity for NMDA Receptors Is Influenced by Small Cations Rinat Nahum-Levy,* Eyal Tam,* Sara Shavit, and Morris Benveniste Department of Physiology and Pharmacology, Sackler School of Medicine, Tel Aviv University, Ramat Aviv, 69978 Israel NMDA receptor currents desensitize in an agonist-dependent extracellular cation prevented the reduction of glutamate affin- manner when either the glutamate or glycine agonist is sub- ity. In addition, the use of choline-, sodium-, or cesium-based saturating. This may result from a conformational change in the intracellular solutions did not alter desensitization characteris- NMDA receptor protein that lowers glutamate and glycine bind- tics, indicating that the site responsible for reduction of gluta- ing site affinity induced by co-agonist binding, channel opening, mate affinity is not in the intracellular domain. The fact that the or ion permeation. We have used whole-cell voltage clamp of reduction of glutamate affinity is dependent on certain small cultured hippocampal neurons with agonist paired-pulse pro- extracellular cations whereas the reduction of glycine affinity is tocols to demonstrate that glutamate and glycine dissociate insensitive to such cations indicates that conformational 7.9- and 6.8-fold slower in the absence of their respective changes induced by the binding of glutamate are not com- co-agonists than when their co-agonists are present. Paired- pletely paralleled by the conformational changes induced by pulse and desensitization protocols were used to show that glycine. Although glutamate and glycine are essential co- co-agonist binding and channel opening are sufficient to cause agonists, these data suggest that they have differential roles in a reduction in glycine affinity, but extracellular sodium or mag- the process of NMDA receptor activation. -

Alcohol Withdrawal Drives Depressive Behaviors by Activating Neurons in the Rostromedial Tegmental Nucleus
Alcohol Withdrawal Drives Depressive Behaviors by Activating Neurons in the Rostromedial Tegmental Nucleus Cite this article as: Rao Fu, Wanhong Zuo, Nimisha Shiwalkar, Qinghua Mei, Qing Fan, Xuejun Chen, Jing Li, Alex Bekker and Jiang-Hong Ye, Alcohol Withdrawal Drives Depressive Behaviors by Activating Neurons in the Rostromedial Tegmental Nucleus, Neuropsychopharmacology doi:10.1038/s41386-019-0378-8 This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version. Terms of use and reuse: academic research for non-commercial purposes, see here for full terms. https://www.nature.com/authors/policies/license.html#AAMtermsV1 © 2019 American College of Neuropsychopharmacology. All rights reserved. Alcohol Withdrawal Drives Depressive Behaviors by Activating Neurons in the Rostromedial Tegmental Nucleus Rao Fu, Wanhong Zuo, Nimisha Shiwalkar, Qinghua Mei, Qing Fan, Xuejun Chen, Jing Li, Alex Bekker, Jiang-Hong Ye* Department of Anesthesiology, Department of Pharmacology, & Physiology and Neuroscience, Rutgers, The State University of New Jersey, New Jersey Medical School, Newark, New Jersey, 07103, USA RF and WZ contribute equally to this work. Corresponding author: Jiang-Hong Ye Department of Anesthesiology, Rutgers, the State University of New Jersey, New Jersey Medical School 185 South Orange Ave, Newark, NJ 07103, USA [email protected] Tel: 973-972-1866 Running title: RMTg in alcohol withdrawal Keywords: dopamine; GABA; nucleus accumbens; chemogenetics; electrophysiology; sucrose preferring test; forced swimming test; functional hemispheric disconnection Abstract: 245 words, Introduction: 330 words, Materials and Methods: 753 words Discussion: 1348 Text total: 4312 (Introduction, Methods, Results, Discussion) # of Figures: 6 # of table 1 # of supplement data: 1 1 © 2019 American College of Neuropsychopharmacology. -

Nomination Background: L-Beta-Methylaminoalanine
Chemical Information Review Document for L-β-Methylaminoalanine [CAS No. 15920-93-1] Supporting Nomination for Toxicological Evaluation by the National Toxicology Program September 2008 National Toxicology Program National Institute of Environmental Health Sciences National Institutes of Health U.S Department of Health and Human Services Research Triangle Park, NC http://ntp.niehs.nih.gov/ Abstract L-β-Methylaminoalanine (L-BMAA) is a neurotoxic non-protein amino acid that is produced by cyanobacteria, a blue-green algae that is common to many lakes, oceans, and soils, and is found in Cycas circinalis seeds. It has previously been associated with the neurological disease amyotrophic lateral sclerosis-Parkinson dementia complex (ALS-PDC) in an indigenous population in Guam. Consumption of tortillas made from cycad-seed flour and of flying foxes (Mariana fruit bats, a "traditional delicacy" in Guam) that feed on cycad fruit has been implicated as the source of L-BMAA exposure. Protein-bound and free L-BMAA have been shown to bioconcentrate in the Guam ecosystem (bacteria, plants, animals, and human tissues) and detectable levels have been measured in brain tissue of people in Guam who suffered from dementia-related disorders. Because it is present in blue-green algae from a variety of water sources around the world and samples of Baltic Sea and oceanic blooms, significant quantities may be released into the world's oceans and water supplies. Studies in primates showed that L-BMAA produced a neurodegenerative syndrome very similar to that of ALS-PDC. Single doses also induced seizures in mice and rats and intracranial injection in mice produced hippocampal damage. -

Demonstration of a Neural Circuit Critical for Imprinting Behavior in Chicks
The Journal of Neuroscience, March 24, 2010 • 30(12):4467–4480 • 4467 Development/Plasticity/Repair Demonstration of a Neural Circuit Critical for Imprinting Behavior in Chicks Tomoharu Nakamori,1,3 Katsushige Sato,2,4 Yasuro Atoji,5 Tomoyuki Kanamatsu,6 Kohichi Tanaka,1 and Hiroko Ohki-Hamazaki1,3,7 1Laboratory of Molecular Neuroscience, School of Biomedical Science and Medical Research Institute and 2Department of Physiology and Cell Biology, Faculty of Medicine, Graduate School, Tokyo Medical and Dental University, Bunkyo-ku, Tokyo 113-8519, Japan, 3Division of Biology, College of Liberal Arts and Sciences, Kitasato University, Sagamihara, Kanagawa 228-8555, Japan, 4Department of Health and Nutrition Sciences, Faculty of Human Health, Komazawa Women’s University, Inagi-shi, Tokyo 206-8511, Japan, 5Laboratory of Veterinary Anatomy, Faculty of Applied Biological Sciences, Gifu University, Gifu 501-1193, Japan, 6Department of Environmental Engineering for Symbiosis, Faculty of Engineering, Soka University, Hachioji, Tokyo 192-8577, Japan, and 7Recognition and Formation, Precursory Research for Embryonic Science and Technology, Japan Science and Technology Agency, Kawaguchi, Saitama 332-0012, Japan Imprinting behavior in birds is elicited by visual and/or auditory cues. It has been demonstrated previously that visual cues are recog- nized and processed in the visual Wulst (VW), and imprinting memory is stored in the intermediate medial mesopallium (IMM) of the telencephalon. Alteration of neural responses in these two regions according to imprinting has been reported, yet direct evidence of the neural circuit linking these two regions is lacking. Thus, it remains unclear how memory is formed and expressed in this circuit. Here, we present anatomical as well as physiological evidence of the neural circuit connecting the VW and IMM and show that imprinting training during the critical period strengthens and refines this circuit. -

Agmatine Improves Spatial Memory
macolog Khales et al., J Pharma Reports 2016, 1:2 ar ic h a P l f R o e l p a o n r r t s u o J Journal of Pharmacological Reports Research Article Article OpenOpen Access Access Agmatine Improves Spatial Memory Consolidation: The Role of Nitric Oxide Golnaz Yadollahi Khales1, Atefeh Khajeh2 and Maryam Moosavi1,3* 1Shiraz Neuroscience Research Center, Shiraz University of Medical Sciences, Shiraz, Iran 2Students Research Committee, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran 3Nanomedicine and Nanobiology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran Abstract Objective: The existence of agmatine in the hippocampus suggests a role in memory formation. Endogenous agmatine increases after training in the hippocampus, howbeit the effect of exogenous agmatine on memory is not consistent yet. This work was aimed to assess the differential effect of systemic agmatine on spatial memory consolidation and retrieval. Additionally L-NAME was used to assess if nitric oxide is involved in the effect of agmatine. Methods: Male Sprague-Dawley rats (250-350 g) were trained in water maze single training session. After 24 h the memory of animals were examined in a probe trial which was consisted of a trial without platform. To assess the effect of agmatine (40 mg/kg) on memory consolidation it was administered immediately after training and to assess its effect on memory retrieval it was injected 30 min before probe trial. In order to evaluate the involvement of nitric oxide, L-NAME (3 mg/kg) was co-administered with agmatine. Results: Post-training injection (to assess consolidation phase) of agmatine improved the performance of animals in probe test, while its pre-probe administration (to assess retrieval phase) had no effect. -

( 12 ) United States Patent
US009737531B2 (12 ) United States Patent ( 10 ) Patent No. : US 9 , 737 ,531 B2 Javitt ( 45) Date of Patent : Aug . 22 , 2017 ( 54 ) COMPOSITION AND METHOD FOR 2008 /0194698 A1 * 8 / 2008 Hermanussen et al. .. .. 514 /662 TREATMENT OF DEPRESSION AND 2011/ 0207776 A18 / 2011 Buntinx 2011 /0306586 Al 12 / 2011 Khan PSYCHOSIS IN HUMANS 2012 /0041026 A12 / 2012 Waizumi (71 ) Applicant : Daniel C Javitt , Bardonia , NY (US ) FOREIGN PATENT DOCUMENTS ( 72 ) Inventor: Daniel C Javitt, Bardonia , NY (US ) CN 101090721 12 / 2007 KR 2007 0017136 A 2 / 2007 ( 73 ) Assignee : GLYTECH , LLC , Ft. Lee, NJ (US ) WO WO 2005 /000216 A2 1 / 2005 WO WO 2005 /065308 A2 7 / 2005 ( * ) Notice : Subject to any disclaimer , the term of this WO WO 2005 /079756 9 / 2005 patent is extended or adjusted under 35 WO 2011044089 4 / 2011 U . S . C . 154 ( b ) by 0 days . wo WO 2012 / 104852 Al 8 / 2012 ( 21 ) Appl. No. : 13 /936 , 198 OTHER PUBLICATIONS Ceglia et al. , “ The 5 -HT2A receptor antagonist M100 , 907 prevents ( 22 ) Filed : Jul. 7 , 2013 extracellular glutamate rising in response to NMDA receptor block ade in the mPFC ,” Journal of Neurochemistry , 2004 , 91 , 189 - 199 . * ((65 65 ) Prior Publication Data Mony et al. , “ Identification of a novel NR2B -selective NMDA US 2014 / 0018348 A1 Jan . 16 , 2014 receptor antagonist using a virtual screening approach , ” Bioorganic & Medicinal Chemistry Letters 20 ( 2010 ) 5552 - 5558 . * Ceglia et al ., “ The 5HT2A receptor antagonist M100 , 907 prevents Related U . S . Application Data extracellular glutamate rising in response to NMDA receptor block ( 60 ) Provisional application No . -

The Effects of Excitatory Amino Acids on Intracellular Calcium in Single Mouse Striatal Neurons in Vitro
The Journal of Neuroscience, December 1987, 7(12): 4145-4158 The Effects of Excitatory Amino Acids on Intracellular Calcium in Single Mouse Striatal Neurons in vitro Shawn N. Murphy, Stanley A. Thayer, and Richard J. Miller Department of Pharmacological and Physiological Sciences, University of Chicago, Chicago, Illinois 60637 Using microspectrofluorimetry and the calcium-sensitive dye also often been observed that administration of glutamate or fura-2, we examined the effect of excitatory amino acids on its structural analogs directly into the brain is highly toxic and [Ca*+], in single striatal neurons in vitro. Kmethyl-o-aspartic results in the destruction of neurons whose cell bodies are close acid (NMDA) produced rapid increases in [Ca*+],. These were to the site of administration (Olney, 1969; Schwartz et al., 1984; blocked by oL-2-amino4phosphonovaleric acid (AP5), by Rothman, 1985). Apart from being a useful lesioning technique, Mg2+, by phencyclidine, and by MK801. The block produced such effects may be extremely important in certain pathological by Mg*+ and MK801 could be relieved by depolarizing cells conditions. For example, it is thought that the neuronal degen- with veratridine. When external Ca*+ was removed, NMDA eration associated with conditions such as cerebral ischemia, no longer increased [Ca*+],. Furthermore, the effects of NMDA epilepsy, Alzheimer’s disease, and Huntington’s chorea may were not blocked by concentrations of La3+ that blocked result from the release of abnormal quantities of glutamate-like depolarization induced rises in [Cal+],. Substitution of Na+, agonists in situ under certain conditions (Schwartz et al., 1984). by Li+ did not block the effects of NMDA. -

The 1980S: D-AP5, LTP and a Decade of NMDA Receptor Discoveries
Neurochemical Research https://doi.org/10.1007/s11064-018-2640-6 ORIGINAL PAPER The 1980s: D-AP5, LTP and a Decade of NMDA Receptor Discoveries D. Lodge1 · J. C. Watkins1 · Z. A. Bortolotto1 · D. E. Jane1 · A. Volianskis2,3 Received: 26 June 2018 / Revised: 12 September 2018 / Accepted: 17 September 2018 © The Author(s) 2018 Abstract In the 1960s and 70s, biochemical and pharmacological evidence was pointing toward glutamate as a synaptic transmitter at a number of distinct receptor classes, known as NMDA and non-NMDA receptors. The field, however, lacked a potent and highly selective antagonist to block these putative postsynaptic receptors. So, the discoveries in the early 1980s of D-AP5 as a selective NMDA receptor antagonist and of its ability to block synaptic events and plasticity were a major breakthrough leading to an explosion of knowledge about this receptor subtype. During the next 10 years, the role of NMDA receptors was established in synaptic transmission, long-term potentiation, learning and memory, epilepsy, pain, among others. Hints at pharmacological heterogeneity among NMDA receptors were followed by the cloning of separate subunits. The purpose of this review is to recognize the important contributions made in the 1980s by Graham L. Collingridge and other key scientists to the advances in our understanding of the functions of NMDA receptors throughout the central nervous system. Keywords Long-term potentiation (LTP) · NMDA · NMDA receptors · APV · D-AP5 · Synaptic plasticity Introduction at the time, stating that ‘NMA receptors…may play a role in synaptic plasticity’, this observation, and the use of this new The 1980s proved to be a decade where N-methyl-D-aspar- pharmacological tool are at the core of the now established tate (NMDA) receptor-mediated neurotransmission became role of NMDA receptors in excitatory neurotransmission, in firmly established. -

D-Serine and D-Cycloserine Reduce Compulsive Alcohol Intake in Rats
Neuropsychopharmacology (2015) 40, 2357–2367 © 2015 American College of Neuropsychopharmacology. All rights reserved 0893-133X/15 www.neuropsychopharmacology.org D-Serine and D-Cycloserine Reduce Compulsive Alcohol Intake in Rats Taban Seif1, Jeffrey A Simms1, Kelly Lei1, Scott Wegner1, Antonello Bonci2,3, Robert O Messing1,4 and *,1 F Woodward Hopf 1Department of Neurology, University of California at San Francisco, San Francisco, CA, USA; 2NIDA Intramural Research Program, Baltimore, MD, USA; 3Solomon H. Snyder Department of Neuroscience, The Johns Hopkins University, School of Medicine, Baltimore, MD, USA; 4 The University of Texas at Austin, College of Pharmacy, Austin, TX, USA There is considerable interest in NMDAR modulators to enhance memory and treat neuropsychiatric disorders such as addiction, depression, and schizophrenia. D-serine and D-cycloserine, the NMDAR activators at the glycine site, are of particular interest because they have been used in humans without serious adverse effects. Interestingly, D-serine also inhibits some NMDARs active at hyperpolarized potentials (HA-NMDARs), and we previously found that HA-NMDARs within the nucleus accumbens core (NAcore) are critical for promoting compulsion-like alcohol drinking, where rats consume alcohol despite pairing with an aversive stimulus such as quinine, a paradigm considered to model compulsive aspects of human alcohol use disorders (AUDs). Here, we examined the impact of D-serine and D-cycloserine on this aversion-resistant alcohol intake (that persists despite adulteration with quinine) and consumption of quinine-free alcohol. Systemic D-serine reduced aversion-resistant alcohol drinking, without altering consumption of quinine-free alcohol or saccharin with or without quinine. Importantly, D-serine within the NAcore but not the dorsolateral striatum also selectively reduced aversion- resistant alcohol drinking. -
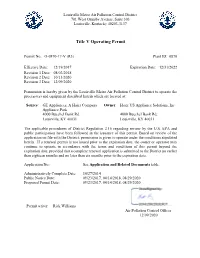
Title V Operating Permit
Louisville Metro Air Pollution Control District 701 West Ormsby Avenue, Suite 303 Louisville, Kentucky 40203-3137 Title V Operating Permit Permit No.: O-0870-17-V (R3) Plant ID: 0870 Effective Date: 12/19/2017 Expiration Date: 12/31/2022 Revision 1 Date: 08/02/2018 Revision 2 Date: 10/13/2020 Revision 3 Date: 12/09/2020 Permission is hereby given by the Louisville Metro Air Pollution Control District to operate the process(es) and equipment described herein which are located at: Source: GE Appliances, A Haier Company – Owner: Haier US Appliance Solutions, Inc Appliance Park 4000 Buechel Bank Rd. 4000 Buechel Bank Rd, Louisville, KY 40031 Louisville, KY 40031 The applicable procedures of District Regulation 2.16 regarding review by the U.S. EPA and public participation have been followed in the issuance of this permit. Based on review of the application on file with the District, permission is given to operate under the conditions stipulated herein. If a renewal permit is not issued prior to the expiration date, the owner or operator may continue to operate in accordance with the terms and conditions of this permit beyond the expiration date, provided that a complete renewal application is submitted to the District no earlier than eighteen months and no later than six months prior to the expiration date. Application No.: See Application and Related Documents table. Administratively Complete Date: 10/27/2014 Public Notice Date: 09/23/2017, 04/14/2018, 08/29/2020 Proposed Permit Date: 09/23/2017, 04/14/2018, 08/29/2020 Permit writer: Rick Williams Air Pollution Control Officer 12/09/2020 Plant ID: 0870 Table of Contents Permit Revisions and Changes.......................................................................................................