Alcohol Withdrawal Drives Depressive Behaviors by Activating Neurons in the Rostromedial Tegmental Nucleus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Switch to Tonic Discharge by Thyrotropin-Releasing Hormone
Neuron Article Synchronized Network Oscillations in Rat Tuberoinfundibular Dopamine Neurons: Switch to Tonic Discharge by Thyrotropin-Releasing Hormone David J. Lyons,1,* Emilia Horjales-Araujo,1 and Christian Broberger1,* 1Department of Neuroscience, Karolinska Institutet, 171 77 Stockholm, Sweden *Correspondence: [email protected] (D.J.L.), [email protected] (C.B.) DOI 10.1016/j.neuron.2009.12.024 SUMMARY most common form of pituitary tumor (Burrow et al., 1981), and by the hyperprolactinaemia and sometimes galactorrhea that The pituitary hormone, prolactin, triggers lactation in is a side effect of antipsychotic drugs with DA antagonist prop- nursing mothers. Under nonlactating conditions, erties (Clemens et al., 1974; Meltzer and Fang, 1976). Yet, to prolactin secretion is suppressed by powerful inhibi- date, the cellular and network electrophysiological properties tion from hypothalamic tuberoinfundibular dopamine of the TIDA cell population have not been described. These (TIDA) neurons. Although firing pattern has been sug- factors are potentially fundamental features of prolactin regula- gested as integral to neuroendocrine control, the tion since discharge pattern may determine the functional output of neuroendocrine control of the anterior pituitary, as is observed electrical behavior of TIDA cells remains unknown. in the magnocellular system (Wakerley and Lincoln, 1973; Hatton We demonstrate that rat TIDA neurons discharge et al., 1983). Thus, the periodic bursting pattern in hypothalamic rhythmically in a robust 0.05 Hz oscillation. The oscil- gonadotropin-releasing hormone neurons is required for stimu- lation is phase locked between neurons, and while it lation of target gonadotrophs in the pituitary (Knobil, 1980). persists during chemical synaptic transmission When bursting is artificially replaced by continuous agonist stim- blockade, it is abolished by gap junction antagonists. -

Is Shuma the Chinese Analog of Soma/Haoma? a Study of Early Contacts Between Indo-Iranians and Chinese
SINO-PLATONIC PAPERS Number 216 October, 2011 Is Shuma the Chinese Analog of Soma/Haoma? A Study of Early Contacts between Indo-Iranians and Chinese by ZHANG He Victor H. Mair, Editor Sino-Platonic Papers Department of East Asian Languages and Civilizations University of Pennsylvania Philadelphia, PA 19104-6305 USA [email protected] www.sino-platonic.org SINO-PLATONIC PAPERS FOUNDED 1986 Editor-in-Chief VICTOR H. MAIR Associate Editors PAULA ROBERTS MARK SWOFFORD ISSN 2157-9679 (print) 2157-9687 (online) SINO-PLATONIC PAPERS is an occasional series dedicated to making available to specialists and the interested public the results of research that, because of its unconventional or controversial nature, might otherwise go unpublished. The editor-in-chief actively encourages younger, not yet well established, scholars and independent authors to submit manuscripts for consideration. Contributions in any of the major scholarly languages of the world, including romanized modern standard Mandarin (MSM) and Japanese, are acceptable. In special circumstances, papers written in one of the Sinitic topolects (fangyan) may be considered for publication. Although the chief focus of Sino-Platonic Papers is on the intercultural relations of China with other peoples, challenging and creative studies on a wide variety of philological subjects will be entertained. This series is not the place for safe, sober, and stodgy presentations. Sino- Platonic Papers prefers lively work that, while taking reasonable risks to advance the field, capitalizes on brilliant new insights into the development of civilization. Submissions are regularly sent out to be refereed, and extensive editorial suggestions for revision may be offered. Sino-Platonic Papers emphasizes substance over form. -
Last Name First Name/Middle Name Course Award Course 2 Award 2 Graduation
Last Name First Name/Middle Name Course Award Course 2 Award 2 Graduation A/L Krishnan Thiinash Bachelor of Information Technology March 2015 A/L Selvaraju Theeban Raju Bachelor of Commerce January 2015 A/P Balan Durgarani Bachelor of Commerce with Distinction March 2015 A/P Rajaram Koushalya Priya Bachelor of Commerce March 2015 Hiba Mohsin Mohammed Master of Health Leadership and Aal-Yaseen Hussein Management July 2015 Aamer Muhammad Master of Quality Management September 2015 Abbas Hanaa Safy Seyam Master of Business Administration with Distinction March 2015 Abbasi Muhammad Hamza Master of International Business March 2015 Abdallah AlMustafa Hussein Saad Elsayed Bachelor of Commerce March 2015 Abdallah Asma Samir Lutfi Master of Strategic Marketing September 2015 Abdallah Moh'd Jawdat Abdel Rahman Master of International Business July 2015 AbdelAaty Mosa Amany Abdelkader Saad Master of Media and Communications with Distinction March 2015 Abdel-Karim Mervat Graduate Diploma in TESOL July 2015 Abdelmalik Mark Maher Abdelmesseh Bachelor of Commerce March 2015 Master of Strategic Human Resource Abdelrahman Abdo Mohammed Talat Abdelziz Management September 2015 Graduate Certificate in Health and Abdel-Sayed Mario Physical Education July 2015 Sherif Ahmed Fathy AbdRabou Abdelmohsen Master of Strategic Marketing September 2015 Abdul Hakeem Siti Fatimah Binte Bachelor of Science January 2015 Abdul Haq Shaddad Yousef Ibrahim Master of Strategic Marketing March 2015 Abdul Rahman Al Jabier Bachelor of Engineering Honours Class II, Division 1 -

Excitatory Amino Acid Receptor Antagonists and Electroacupuncture Synergetically Inhibit Carrageenan-Induced Behavioral Hyperalgesia and Spinal Fos Expression in Rats
http://www.paper.edu.cn Pain 99 (2002) 525–535 www.elsevier.com/locate/pain Excitatory amino acid receptor antagonists and electroacupuncture synergetically inhibit carrageenan-induced behavioral hyperalgesia and spinal fos expression in rats Yu-Qiu Zhanga, Guang-Chen Jib, Gen-Cheng Wub, Zhi-Qi Zhaoa,* aInstitute of Neurobiology, Fudan University, 220 Han Dan Road, Shanghai, 200433, China bState Key Laboratory of Medical Neurobiology, Medical Center of Fudan University, 138 Yi Xue Yuan Road, Shanghai, 200032, China Received 30 January 2002; accepted 27 June 2002 Abstract The interaction between electroacupuncture and an N-methyl-d-aspartic acid (NMDA) receptor antagonist, (DL-2-amino-5-phosphono- pentanoic acid; AP5), or an ( ^ )-a-Amino-3-hydroxy-5-methylisoxazole-4-propionic acid/kainite (AMPA/KA) receptor antagonist, (6,7- dinitroquinoxaline-2,3 (1H,4H); DNQX) administered intrathecally on carrageenan-induced thermal hyperalgesia and spinal c-Fos expres- sion was investigated. The latency of paw withdrawal (PWL) from a thermal stimulus was used as a measure of hyperalgesia in awake rats. Intrathecal (i.t.) injection of 1 and 10 nmol AP5, but not DNQX, markedly increased the PWL of the carrageenan-injected paw. At a dose of 100 nmol, either AP5 or DNQX significantly increased the PWL of carrageenan-injected paw, with AP5 being more potent. The PWLs of the non-injected and normal saline (NS)-injected paws were not detectably affected by the administration of NMDA or AMPA/KA receptor antagonists at the doses tested. Unilateral electroacupuncture stimulation of the ‘Zu-San-Li’ (St 36) and ‘Kun-Lun’ (UB 60) acupuncture points (60 and 2 Hz alternately, 1–2–3 mA) contralateral to the carrageenan-injected paw significantly elevated the PWLs of carrageenan- and NS-injected paws. -

Prof. J. Joshua Yang University of Southern California, USA
NANO KOREA 2021 July 7~9, KINTEX, Korea Prof. J. Joshua Yang University of Southern California, USA Address: 3737 Watt Way, PHE 608, Los Angeles, CA 90089-0271, USA Telephone: 001- (213) 740-4709 Fax: E-mail: [email protected] Nationality: China Web:http://www.ecs.umass.edu/ece/jjyang/ EDUCATION Doctoral Degree, University of Wisconsin – Madison, 2007 Master's Degree, University of Wisconsin – Madison, 2003 Bachelor's Degree, Southeast University, 1997 PROFESSIONAL ACTIVITIES Advisory Board: Neuromorphic Computing and Engineering (IoP): Senior Advisory Panel ADVANCED INTELLIGENT SYSTEMS (Wiley): Executive Advisory Board ADVANCED MATERIALS TECHNOLOGIES (Wiley): International Advisory Board SMALL STRUCTURE (Wiley): International Advisory Board Editorial Board: SCIENTIFIC REPORTS, FRONTIERS IN NEUROSCIENCE Conference Chairs: The 8th and 10th IEEE Nanotechnology Symposiums on “Emerging Non-volatile Memory Technologies” 2012, and “2D Devices and Materials” 2014, respectively; Conference co-Chair: The IEEE International Conference on Future Computing, 2017, 2018, 2019. AWARD AND HONORS Winner of UMass Spotlight Scholar (2017). Nominee for Samuel F. Conti Faculty Fellowship Awards (2018). Oversea review expert of CAS (2018). NVMTS2019 Best poster award. (2019). UMass Amherst Distinguished Faculty Lecturer (2019). UMass Chancellor's Medal (highest honor of UMass, 2019). Best paper in Advanced Materials Technologies 2019, Wiley. NANO KOREA 2021 July 7~9, KINTEX, Korea Clarivate™ Highly Cited Researchers in the field of Cross-Field (2020). MAIN SCIENTIFIC PUBLICATION Z. Wang, H. Wu, G. Burr, C. S. Hwang, K. L. Wang, Q. Xia* and J. Joshua Yang*, “Resistive switching materials for information processing”, NATURE REVIEW MATERIALS 5, 173-195 (2020). P. Lin, C. Li, Z. Wang, Y. Li, H. -

Chinese Zheng and Identity Politics in Taiwan A
CHINESE ZHENG AND IDENTITY POLITICS IN TAIWAN A DISSERTATION SUBMITTED TO THE GRADUATE DIVISION OF THE UNIVERSITY OF HAWAI‘I AT MĀNOA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN MUSIC DECEMBER 2018 By Yi-Chieh Lai Dissertation Committee: Frederick Lau, Chairperson Byong Won Lee R. Anderson Sutton Chet-Yeng Loong Cathryn H. Clayton Acknowledgement The completion of this dissertation would not have been possible without the support of many individuals. First of all, I would like to express my deep gratitude to my advisor, Dr. Frederick Lau, for his professional guidelines and mentoring that helped build up my academic skills. I am also indebted to my committee, Dr. Byong Won Lee, Dr. Anderson Sutton, Dr. Chet- Yeng Loong, and Dr. Cathryn Clayton. Thank you for your patience and providing valuable advice. I am also grateful to Emeritus Professor Barbara Smith and Dr. Fred Blake for their intellectual comments and support of my doctoral studies. I would like to thank all of my interviewees from my fieldwork, in particular my zheng teachers—Prof. Wang Ruei-yu, Prof. Chang Li-chiung, Prof. Chen I-yu, Prof. Rao Ningxin, and Prof. Zhou Wang—and Prof. Sun Wenyan, Prof. Fan Wei-tsu, Prof. Li Meng, and Prof. Rao Shuhang. Thank you for your trust and sharing your insights with me. My doctoral study and fieldwork could not have been completed without financial support from several institutions. I would like to first thank the Studying Abroad Scholarship of the Ministry of Education, Taiwan and the East-West Center Graduate Degree Fellowship funded by Gary Lin. -

Glutamate but Not Glycine Agonist Affinity for NMDA Receptors Is
The Journal of Neuroscience, April 1, 2002, 22(7):2550–2560 Glutamate But Not Glycine Agonist Affinity for NMDA Receptors Is Influenced by Small Cations Rinat Nahum-Levy,* Eyal Tam,* Sara Shavit, and Morris Benveniste Department of Physiology and Pharmacology, Sackler School of Medicine, Tel Aviv University, Ramat Aviv, 69978 Israel NMDA receptor currents desensitize in an agonist-dependent extracellular cation prevented the reduction of glutamate affin- manner when either the glutamate or glycine agonist is sub- ity. In addition, the use of choline-, sodium-, or cesium-based saturating. This may result from a conformational change in the intracellular solutions did not alter desensitization characteris- NMDA receptor protein that lowers glutamate and glycine bind- tics, indicating that the site responsible for reduction of gluta- ing site affinity induced by co-agonist binding, channel opening, mate affinity is not in the intracellular domain. The fact that the or ion permeation. We have used whole-cell voltage clamp of reduction of glutamate affinity is dependent on certain small cultured hippocampal neurons with agonist paired-pulse pro- extracellular cations whereas the reduction of glycine affinity is tocols to demonstrate that glutamate and glycine dissociate insensitive to such cations indicates that conformational 7.9- and 6.8-fold slower in the absence of their respective changes induced by the binding of glutamate are not com- co-agonists than when their co-agonists are present. Paired- pletely paralleled by the conformational changes induced by pulse and desensitization protocols were used to show that glycine. Although glutamate and glycine are essential co- co-agonist binding and channel opening are sufficient to cause agonists, these data suggest that they have differential roles in a reduction in glycine affinity, but extracellular sodium or mag- the process of NMDA receptor activation. -

Spatial and Temporal Changes of Arable Land Driven by Urbanization and Ecological Restoration in China
Chin. Geogra. Sci. 2018 Vol. 28 No. 4 pp. *–* Springer Science Press https://doi.org/10.1007/s11769-018-0983-1 www.springerlink.com/content/1002-0063 Spatial and Temporal Changes of Arable Land Driven by Urbanization and Ecological Restoration in China WANG Liyan 1,2, ANNA Herzberger3, ZHANG Liyun1,2, XIAO Yi1, WANG Yaqing1,2, XIAO Yang1, LIU Jianguo3, 1 OUYANG Zhiyun (1. State Key Laboratory of Urban and Regional Ecology, Research Center for Eco-Environmental Sciences, Chinese Academy of Sci- ences, Beijing 100085, China; 2. University of Chinese Academy of Sciences, Beijing 100049, China; 3. Center for Systems Integration and Sustainability, Michigan State University, East Lansing, MI48823, USA) Abstract: Since the industrial revolution, human activities have both expanded and intensified across the globe resulting in accelerated land use change. Land use change driven by China’s development has put pressure on the limited arable land resources, which has af- fected grain production. Competing land use interests are a potential threat to food security in China. Therefore, studying arable land use changes is critical for ensuring future food security and maintaining the sustainable development of arable land. Based on data from several major sources, we analyzed the spatio-temporal differences of arable land among different agricultural regions in China from 2000 to 2010 and identified the drivers of arable land expansion and loss. The results revealed that arable land decreased by 5.92 million ha or 3.31%. Arable land increased in the north and decreased in the south of China. Urbanization and ecological restoration programs were the main drivers of arable land loss, while the reclamation of other land cover types (e.g., forest, grassland, and wetland) was the primary source of the increased arable land. -
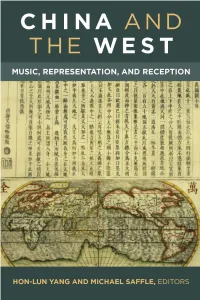
China and the West: Music, Representation, and Reception
Revised Pages China and the West Revised Pages Wanguo Quantu [A Map of the Myriad Countries of the World] was made in the 1620s by Guilio Aleni, whose Chinese name 艾儒略 appears in the last column of the text (first on the left) above the Jesuit symbol IHS. Aleni’s map was based on Matteo Ricci’s earlier map of 1602. Revised Pages China and the West Music, Representation, and Reception Edited by Hon- Lun Yang and Michael Saffle University of Michigan Press Ann Arbor Revised Pages Copyright © 2017 by Hon- Lun Yang and Michael Saffle All rights reserved This book may not be reproduced, in whole or in part, including illustrations, in any form (beyond that copying permitted by Sections 107 and 108 of the U.S. Copyright Law and except by reviewers for the public press), without written permission from the publisher. Published in the United States of America by the University of Michigan Press Manufactured in the United States of America c Printed on acid- free paper 2020 2019 2018 2017 4 3 2 1 A CIP catalog record for this book is available from the British Library. Library of Congress Cataloging- in- Publication Data Names: Yang, Hon- Lun, editor. | Saffle, Michael, 1946– editor. Title: China and the West : music, representation, and reception / edited by Hon- Lun Yang and Michael Saffle. Description: Ann Arbor : University of Michigan Press, 2017. | Includes bibliographical references and index. Identifiers: LCCN 2016045491| ISBN 9780472130313 (hardcover : alk. paper) | ISBN 9780472122714 (e- book) Subjects: LCSH: Music—Chinese influences. | Music—China— Western influences. | Exoticism in music. -

Mandarin Chinese 2
® Mandarin Chinese 2 Reading Booklet & Culture Notes Mandarin Chinese 2 Travelers should always check with their nation’s State Department for current advisories on local conditions before traveling abroad. Booklet Design: Maia Kennedy © and ‰ Recorded Program 2002 Simon & Schuster, Inc. © Reading Booklet 2016 Simon & Schuster, Inc. Pimsleur® is an imprint of Simon & Schuster Audio, a division of Simon & Schuster, Inc. Mfg. in USA. All rights reserved. ii Mandarin Chinese 2 ACKNOWLEDGMENTS VOICES Audio Program English-Speaking Instructor. Ray Brown Mandarin-Speaking Instructor . Qing Rao Female Mandarin Speaker . Mei Ling Diep Male Mandarin Speaker . Yaohua Shi Reading Lessons Female Mandarin Speaker . Xinxing Yang Male Mandarin Speaker . Jay Jiang AUDIO PROGRAM COURSE WRITERS Yaohua Shi Christopher J. Gainty READING LESSON WRITERS Xinxing Yang Elizabeth Horber REVIEWER Zhijie Jia EDITORS Joan Schoellner Beverly D. Heinle PRODUCER & DIRECTOR Sarah H. McInnis RECORDING ENGINEERS Peter S. Turpin Kelly Saux Simon & Schuster Studios, Concord, MA iiiiii Mandarin Chinese 2 Table of Contents Introduction Mandarin .............................................................. 1 Pictographs ........................................................ 2 Traditional and Simplified Script ....................... 3 Pinyin Transliteration ......................................... 3 Readings ............................................................ 4 Tonality ............................................................... 5 Tone Change or Tone Sandhi -

Performing Chinese Contemporary Art Song
Performing Chinese Contemporary Art Song: A Portfolio of Recordings and Exegesis Qing (Lily) Chang Submitted in fulfilment of the requirements for the degree of Doctor of Philosophy Elder Conservatorium of Music Faculty of Arts The University of Adelaide July 2017 Table of contents Abstract Declaration Acknowledgements List of tables and figures Part A: Sound recordings Contents of CD 1 Contents of CD 2 Contents of CD 3 Contents of CD 4 Part B: Exegesis Introduction Chapter 1 Historical context 1.1 History of Chinese art song 1.2 Definitions of Chinese contemporary art song Chapter 2 Performing Chinese contemporary art song 2.1 Singing Chinese contemporary art song 2.2 Vocal techniques for performing Chinese contemporary art song 2.3 Various vocal styles for performing Chinese contemporary art song 2.4 Techniques for staging presentations of Chinese contemporary art song i Chapter 3 Exploring how to interpret ornamentations 3.1 Types of frequently used ornaments and their use in Chinese contemporary art song 3.2 How to use ornamentation to match the four tones of Chinese pronunciation Chapter 4 Four case studies 4.1 The Hunchback of Notre Dame by Shang Deyi 4.2 I Love This Land by Lu Zaiyi 4.3 Lullaby by Shi Guangnan 4.4 Autumn, Pamir, How Beautiful My Hometown Is! by Zheng Qiufeng Conclusion References Appendices Appendix A: Romanized Chinese and English translations of 56 Chinese contemporary art songs Appendix B: Text of commentary for 56 Chinese contemporary art songs Appendix C: Performing Chinese contemporary art song: Scores of repertoire for examination Appendix D: University of Adelaide Ethics Approval Number H-2014-184 ii NOTE: 4 CDs containing 'Recorded Performances' are included with the print copy of the thesis held in the University of Adelaide Library. -

Origin Narratives: Reading and Reverence in Late-Ming China
Origin Narratives: Reading and Reverence in Late-Ming China Noga Ganany Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2018 © 2018 Noga Ganany All rights reserved ABSTRACT Origin Narratives: Reading and Reverence in Late Ming China Noga Ganany In this dissertation, I examine a genre of commercially-published, illustrated hagiographical books. Recounting the life stories of some of China’s most beloved cultural icons, from Confucius to Guanyin, I term these hagiographical books “origin narratives” (chushen zhuan 出身傳). Weaving a plethora of legends and ritual traditions into the new “vernacular” xiaoshuo format, origin narratives offered comprehensive portrayals of gods, sages, and immortals in narrative form, and were marketed to a general, lay readership. Their narratives were often accompanied by additional materials (or “paratexts”), such as worship manuals, advertisements for temples, and messages from the gods themselves, that reveal the intimate connection of these books to contemporaneous cultic reverence of their protagonists. The content and composition of origin narratives reflect the extensive range of possibilities of late-Ming xiaoshuo narrative writing, challenging our understanding of reading. I argue that origin narratives functioned as entertaining and informative encyclopedic sourcebooks that consolidated all knowledge about their protagonists, from their hagiographies to their ritual traditions. Origin narratives also alert us to the hagiographical substrate in late-imperial literature and religious practice, wherein widely-revered figures played multiple roles in the culture. The reverence of these cultural icons was constructed through the relationship between what I call the Three Ps: their personas (and life stories), the practices surrounding their lore, and the places associated with them (or “sacred geographies”).