Priory Residential and Nursing Home
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Monmouthshire Local Development Plan (Ldp) Proposed Rural Housing
MONMOUTHSHIRE LOCAL DEVELOPMENT PLAN (LDP) PROPOSED RURAL HOUSING ALLOCATIONS CONSULTATION DRAFT JUNE 2010 CONTENTS A. Introduction. 1. Background 2. Preferred Strategy Rural Housing Policy 3. Village Development Boundaries 4. Approach to Village Categorisation and Site Identification B. Rural Secondary Settlements 1. Usk 2. Raglan 3. Penperlleni/Goetre C. Main Villages 1. Caerwent 2. Cross Ash 3. Devauden 4. Dingestow 5. Grosmont 6. Little Mill 7. Llanarth 8. Llandewi Rhydderch 9. Llandogo 10. Llanellen 11. Llangybi 12. Llanishen 13. Llanover 14. Llanvair Discoed 15. Llanvair Kilgeddin 16. Llanvapley 17. Mathern 18. Mitchell Troy 19. Penallt 20. Pwllmeyric 21. Shirenewton/Mynyddbach 22. St. Arvans 23. The Bryn 24. Tintern 25. Trellech 26. Werngifford/Pandy D. Minor Villages (UDP Policy H4). 1. Bettws Newydd 2. Broadstone/Catbrook 3. Brynygwenin 4. Coed-y-Paen 5. Crick 6. Cuckoo’s Row 7. Great Oak 8. Gwehelog 9. Llandegveth 10. Llandenny 11. Llangattock Llingoed 12. Llangwm 13. Llansoy 14. Llantillio Crossenny 15. Llantrisant 16. Llanvetherine 17. Maypole/St Maughans Green 18. Penpergwm 19. Pen-y-Clawdd 20. The Narth 21. Tredunnock A. INTRODUCTION. 1. BACKGROUND The Monmouthshire Local Development Plan (LDP) Preferred Strategy was issued for consultation for a six week period from 4 June 2009 to 17 July 2009. The results of this consultation were reported to Council in January 2010 and the Report of Consultation was issued for public comment for a further consultation period from 19 February 2010 to 19 March 2010. The present report on Proposed Rural Housing Allocations is intended to form the basis for a further informal consultation to assist the Council in moving forward from the LDP Preferred Strategy to the Deposit LDP. -

CONSULTATION DOCUMENT Proposed Federation of Kymin View Primary School and Llandogo Primary School
CONSULTATION DOCUMENT Proposed Federation of Kymin View Primary School and Llandogo Primary School Contents 1. Introduction ...................................................................................... 3 2. Background to Kymin View and Llandogo Primary School ................................. 4 3. Schools Aims and Policies ....................................................................... 4 4. Pupil Attainment ................................................................................. 5 5. School Budgets ................................................................................... 6 6. Pupil Projections ................................................................................ 6 7. HR Compliance ................................................................................... 7 8. Premises .......................................................................................... 7 9. Relationship with Community ................................................................. 7 10. Annual Report to Parents ..................................................................... 8 11.Proposed Instrument of Government ......................................................... 8 12 Timeline for proposal ........................................................................... 9 Appendix 1 – Budget Statement Kymin View Primary School ................................ 10 Appendix 2 Budget Statement Llandogo Primary School ..................................... 11 Appendix 3 Proposed Instrument of Government ............................................ -

ROSE COTTAGE Trellech ! Monmouthshire
ROSE COTTAGE Trellech ! Monmouthshire ROSE COTTAGE Cleddon, Trellech ! Monmouthshire, NP25 4PN Rose Cottage is situated in an idyllic setting nestled between Monmouth and Chepstow in the Wye Valley AONB. It is surrounded by pretty countryside excellent for riding and walking, yet accessible to major road networks and good local schools. Entrance Hall ! Kitchen ! Sitting Room ! Dining Room Snug ! Study ! Utility ! Shower Room ! Ground Floor Bedroom 4 further Bedrooms ! Family Bathroom Gardens and paddock extending to 1.5 Acres Stables with Tack Room ! Carport/Store Monmouth 7 miles ! Chepstow 8 miles Bristol 25 miles (All Distances are approximate) For further particulars of this and all our properties, visit: elstons.co.uk Location " Situated in an idyllic quiet hamlet between Monmouth and Chepstow. " Located near the picturesque Wye Valley Walk. " Accessible to the M4/M5 for Bristol, Cardiff and The Midlands. " School bus stop nearby for Monmouth schools. Description of property " Good riding and walking directly surrounding the house. " Rose Cottage is a charming traditional Welsh, Stone built cottage. " Extensively modernised to include bespoke kitchen, Aga and limestone flooring. " Large conservatory/dining room with doors opening onto the garden. " Sitting room with beamed ceiling and woodburner stove. " Five bedrooms. " Family bathroom and shower room. Outside " Pretty cottage style gardens. " Stabling block with tack room. " Carport/store. " Flat paddock bordering a stream. " Parking for several cars. Services " Mains water and electricity. Private drainage. " Oil central heating. Fixtures and Fittings " Only those items mentioned in these sale particulars are included in the sale. All others, such as fitted carpets, curtains, and light fittings are specifically excluded but may be made available by separate negotiation. -

Appendix 4 Tintern
Appendix 4: Tintern (other holdings) Monastic holding or landscape feature Name meaning (Mod E = Modern Monastic holding or Grange or manor Location (including current civil parish/ HER NMR Date endowned and Held at Notes Sources name (with variant spellings/ first dates English, OE = Old English, W = landscape feature containing the community and county/ unitary entry entry donor Dissolution or for these) Welsh) type feature authority, and OS grid reference if earlier disposal known) Acle Oak wood (from ac ) clearing (from Manor Acle Acle, Norfolk (TG402102) Y Y 1302; Roger Bigod Held at Dissolution The abbey's most valuable landed possession. Granted ‘all his Calendar of Charter Rolls, 1307; leah ) (OE) (Roger Bigod) manor of Acle, with all the appurtenances, and the William of Worcester Itinery, 1478; advowson of the church there’ (1307). Confirmed as 209 acres of Valor Ecclesiasticus, 1535; List of the demesne arable lands, meadow and pasture grazing, market, Lands of Dissolved Religious Houses, dovecote, turbury rights, two mills, a park (1478). 1540 Saint Edmund's Church, Acle Church of Saint Edmund; Oak wood Rectory and church Acle Acle, Norfolk (TG401102) Y Y 1302; Roger Bigod Not held at Calendar of Charter Rolls, 1307 (from ac ) clearing (from leah ) (OE) tithes Dissolution Aluredeston (Aberdeston, 1223; Alveston, Aelfred's (personal name) farmstead, Grange Aluredeston Plusterwine, Woolaston, Gloucestershire N Y 1302; Roger Bigod Held at Dissolution Grange granted in exchange for Plataland. Chapel, sheepcote, Calendar of Charter Rolls, 1307; Valor 1535; Alverstone, 1536; Alverston, 1540) estate or village (from tun ) (OE) (ST596994) (farmed out) water mill, fulling mill, byre, bake-house etc. -
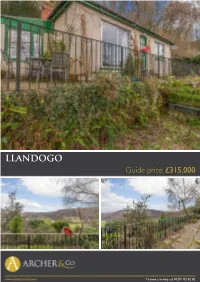
LLANDOGO Guide Price £315,000
LLANDOGO Guide price £315,000 . www.archerandco.com To book a viewing call 01291 62 62 62 www.archerandco.comwww.archerandco.com To book a viewing call 01291 62 62 62 ALPINE LODGE Llandogo, NP25 4TF . 2/3 bedroomed bungalow in need of some updating Magnificent views overlooking Llandogo Village and the Wye Valley Grounds extending to approx 0.3 of an acre . Being sold for the first time in 25 years this 2/3 bedroomed bungalow has been a much loved family home for the Vendors during that time. In need of some updating/modernisation, the property stands in an elevated position commanding truly superb views over the village of Llandogo and the Wye Valley. The property is surrounded by a plethora of walks along the River Wye, the Wye Valley Walk, Offas Dyke Walk and the Cleddon Falls (a site of special scientific interest). The village of Llandogo was once a port, renowned for built the trow' a flat-bottomed river boat which until the 19th Century was used for trading up and down the River Wye. The village is also a designated conservation area. The accommodation comprises conservatory/boot room, cloakroom/utility/boiler room, kitchen, living room, inner hall, two bedrooms and bathroom on the ground floor and to the upper floor is a study and third bedroom/playroom. The gardens and grounds extend to approximately 0.3 of an acre and there is a sloping driveway leading to the parking area. www.archerandco.comwww.archerandco.com To book a viewing call 01291 62 62 62 Guide price £315,000 . -
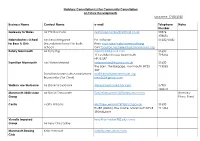
Community Consultation List
Statutory Consultation List for Community Consultation on Future Developments Updated: 17.08.2020 Business Name Contact Name e-mail Telephone Notes Number Gateway to Wales Mr Phil Robinson [email protected] 07876 478652 Haberdashers School Mrs Tessa Norgrove Pa to Bursar: 01600710401 for Boys & Girls (Foundation Bursar) for both Boys: muir.sue@ habsmonmouth.org schools Girls: [email protected] Rotary Monmouth Mr Terry Ing [email protected] 01600 √ 11 Levitsfield Close Monmouth 719426 NP25 5BZ Transition Monmouth Mrs Vivien Mitchell [email protected] 01600 The Barn, The Burgage, Monmouth NP25 715065 3DP Transition Monmouth Administrator [email protected] Bryan Miller (TM Chair) [email protected] Walkers are Welcome Mr Dave Scaysbrook [email protected] 07981 760672 Monmouth 2020 vision Mr David Farnsworth [email protected] (formally Group Place Plan) √ Castle Matty Williams [email protected] 01600 RMRE (Militia), The Castle, Monmouth NP25 711434 3BSAdjutant Visually Impaired [email protected] Group Mr Terry Christopher Monmouth Rowing Kate Harcourt [email protected] Club √ Mitchel Troy Lynne Parker [email protected] Community Council Stoneleigh Llandogo Monmouth NP25 4TA Trellech Community Ms Ann Davison [email protected] 01594 Council 530295 Cllr J Treharne Active Travel Group [email protected] MTC Shire Hall Tristan Blanchard [email protected] Venue (Venue) Andrew Lloyd-Hughes [email protected] -

Review Area 4 Llandogo Village & The
Review Area 4 Llandogo Village & the Surrounding Areas Consultation period: 18th January 2019 to 1st March 2019 1 Contents 1. The Proposal.................................................................................. 3 2. The current position ........................................................................ 4 3. Why are we considering the proposed change? ......................................... 6 4. Background information .................................................................... 7 5. Advantages and Disadvantages of the proposal ......................................... 8 6. Financial Implications ....................................................................... 9 7. What Next? ................................................................................... 9 2 1. The Proposal The Council are considering amending the secondary school catchment area for children and young people currently residing within the village of Llandogo and the immediate surrounding areas. The areas identified currently form part of the catchment area for Llandogo Primary School, and Chepstow School. The map below illustrates the areas that are being considered under this proposal, and will help you to understand whether you could be affected by the proposed changes The Council would like to know your views on whether the secondary school catchment boundary should be amended for the specified areas (area identified above), to form part of the catchment area for Monmouth Comprehensive School, thus aligning the entire catchment area -

Bargains Cottage Llandogo, Monmouthshire
Bargains Cottage Llandogo, Monmouthshire Bargains Cottage Llandogo, Monmouthshire Set high above the Wye Valley with outstanding panoramic views, this pretty and well presented three Approached from sun terrace into: bedroomed cottage has two raised sun terraces, a detached garage and terraced mature woodland OPEN FRONTED PORCH: gardens. Llandogo has a primary school, pub and village shop and is equidistant from Monmouth and Fitted timber benches to both sides. Through vertically Chepstow with easy access to major road networks. boarded solid wooden door with glazed viewing panel into: HALLWAY: Originally dating back 200 years the cottage has a fascinating history. It is constructed in stone under a Doors to the following: slate tiled roof. Sensitively updated with solid wood framed double glazed windows, features include: CLOAK ROOM: Low level WC, wall mounted wash basin, tiled splash back original stone fire places, beams and exposed stone walls and internal doors are vertically boarded with and light over. Cupboard at high level housing consumer Suffolk latches. An oil fired boiler provides heating to radiators throughout. units. Price £385,000 SITTING ROOM: 4.15m x 3.33m (13'7" x 10'11") MASTER BEDROOM: 4.23m x 3.33m average (13'11" Window to front overlooking Wye Valley. Feature stone x 10'11" average) fireplace with recessed wood burner on raised stone hearth Window to front overlooking Wye Valley. Door into: with wooden lintel over. BEDROOM 3/STUDY: 3.35m x 2.78m (11'0" x 9'1") DINING ROOM: 3.79m x 3.2m (12'5" x 10'6") Double aspect with windows to side and front overlooking Pair of windows to front overlooking Wye Valley. -

Cyngor Sir Fynwy / Monmouthshire County Council Rhestr Wythnosol
Cyngor Sir Fynwy / Monmouthshire County Council Rhestr Wythnosol Ceisiadau Cynllunio a Gofrestrwyd / Weekly List of Registered Planning Applications Wythnos / Week 05/09/2019 i/to 11/09/2019 Dyddiad Argraffu / Print Date 12.09.2019 Mae’r Cyngor yn croesawu gohebiaeth yn Gymraeg, Saesneg neu yn y ddwy iaith. Byddwn yn cyfathrebu â chi yn ôl eich dewis. Ni fydd gohebu yn Gymraeg yn arwain at oedi. The Council welcomes correspondence in English or Welsh or both, and will respond to you according to your preference. Corresponding in Welsh will not lead to delay. Ward/ Ward Rhif Cais/ Disgrifia d o'r Cyfeiriad Safle/ Enw a Chyfeiriad yr Enw a Chyfeiriad Math Cais/ Dwyrain/ Application Datblygiad/ Site Address Ymgeisydd/ yr Asiant/ Application Gogledd Number Development Applicant Name & Agent Name & Type Easting/ Description Address Address Northing Llanover DM/2019/01425 Erection of 2 No. Great Tyrmynach Mr Andrew Certificate of 339849 boiler houses and Farm Whittingham Mr Ian Pick ExistLawful 208250 Plwyf/ Parish: Dyddiad App. Dilys/ installation of 2 No. Tre-mynach Road J P P Whittingham Ian Pick Associates Use or Dev Llanarth Date App. Valid: 199kw biomass Bryngwyn and Son Ltd 12.09.2019 Community boilers. Usk Great Tyrmynach Station Farm Offices Council Monmouthshire Farm, Wansford Road NP15 2JP Tre-Mynach Road Driffield Bryngwyn YO25 8NJ NP15 2JP East Yorkshire Llanover DM/2019/01426 Construction of 3 Lower Pentwyn Mr Andrew Certificate of 333723 No. boiler houses Farm Whittingham Mr Ian Pick ExistLawful 206131 Plwyf/ Parish: Dyddiad App. Dilys/ and installation of 3 Nant-y-derry Road J P P Whittingham Ian Pick Associates Use or Dev Llanover Date App. -
Wordsworth Walk
Hill Rive Fo r C rt o s n n e c t i o n s Wordsworth Walk Circular walk around Llandogo 2 HOUR, 3 MILE WALK (with steep sections to viewpoint) Through riverside meadows and along village tracks, climbing in the footsteps of William Wordsworth to the Bread and Cheese viewpoint and Cleddon Shoots waterfall. Discover the heritage of the Wye Valley through our four themes Hil Riv Hid Hill Rive Vi l F View er de Fo r ew o p C n r C po rt o o t o s i I s n in n n n n t t n s s d e e u c c s t t i t i o r o y n n s s Hill Rive Hill F Fo r C o r rt t o s s n n e c t i o n s Hill Forts Hidden Industry River Connections Viewpoints ‘Upon the Little Echoing to the sound of ‘If you have never ‘so uncommonly Doward, a hill of hammers and forges and excellent, that the most with fiery furnaces belching navigated the peculiarly fine exact critic in landscape out fumes and smoke the would scarcely wish to outline….. are the Wye Valley was one of the Wye, you have alter a position in the interesting remains of earliest places in the UK to nothing.’ seen assemblage of woods, industrialise. Pioneering William Gilpin, 1783 a British camp. Three cliffs, ruins and water’ circular terraces wind ironmasters took advantage of the wood and water all Think of the Wye as a watery Wyndham, 1774 up to the summit.’ highway linking the riverside around, putting the Valley’s Tourists first discovered the Fosbroke, 1818 villages with the wider world metal-making industries at beauty of the Wye Valley in and you’ll begin to understand Considering what striking the cutting edge of industrial the 18th century when it its importance in earlier features they are in today’s development. -

Vebraalto.Com
The Old Farmhouse Cottage Llandogo, Monmouth, Monmouthshire, NP25 4TL 3 3 2 F DIRECTIONS From our Chepstow office proceed up the High Street turning right onto Welsh Street. Continue to the roundabout £369,950 taking the third exit onto the Wye Valley link road. Proceed through the village of Tintern and into Llandogo. Turn left directly before Browns Shop and then turn left into the first available car park area where you will find the property. SERVICES Mains water and electric, oil fired central heating and private drainage. TENURE - FREEHOLD You are recommended to have this verified by your legal advisors at your earliest convenience. Description The Old Farmhouse Cottage comprises a deceptively spacious semi-detached cottage situated within the picturesque rural village of Llandogo, a popular area of the Wye Valley. Being within a designated AONB there are an abundance of beautiful views and fantastic walks surrounding the property. Internally the property offers a reception hall with access to ground floor WC, stairs to the first floor and steps down to the living room. The living room is a spacious reception room with further access to the study/snug, kitchen dining room, cellar and rear lobby which in turn leads to the ground floor bedroom and en-suite. To the first floor is the principal bedroom with open plan bathroom/en-suite area and second bedroom again within en-suite facilities. Outside the property benefits from off-road parking area within a shared access car park which lead to the gardens. The garden itself occupies a sunny aspect with cottage style landscaping complete with level lawn, natural pond and well stocked borders. -

Ministry Areas in Monmouth Archdeaconry
Monmouth Ministry Areas No. 1 Abergavenny (St Mary, Christchurch) Llanwenarth (St Peter) Abergavenny (Holy Trinity) Govilon (Christchurch) Llanfoist (St Ffwyst) Llanelen (St Helen) No. 2 Llantilio Pertholey (St Teilo, Bettws Chapel) Llanfihangel Crucorney Group (United Parish of Crucorney) (St David, St Martin, St Michael) Grosmont (St Nicholas) Skenfrith (St Bride) Llanfair (St Mary) Llangattock Lingoed (St Cadoc) Llanaddewi Rydderch (St David) Llanarth & Llansantfraed (St Bridget) Llangattock - j - Usk (St Cadoc) Llantilio Crossenny (St Teilo) Penrhos (St Cadoc) Llanvetherine (St James the Elder) Llanvapley (St Mable) Llanddewi Skirrid (St David) Monmouth Ministry Areas No. 3 Dingestow (St Dingat) Cwmcarvan (St Catwg) Penyclawdd (St Martin) Tregaer (St Mary) Rockfield (St Cenhedlon) St Maughan's & Llangattock - Vibon Avel (St Cadoc, St Meugan) Llanvihangel-ystern-llewern (St Michael) Monmouth (St Mary the Virgin) Overmonnow (St Thomas) Mitchel Troy (St Michael) Wonastow (St Wonnow) Llandogo (St Oudoceus) Tintern (St Michael) Llanishen (St Dennis) Trellech Grange (Parish Church) Llanfihangel-Tor-y-Mynydd (St Michael) Llansoy (St Tysoi) Trellech & Penallt (Old St Marys Church, St Nicholas) No. 4 Caerwent (St Stephen & St Tathan) Llanvair Discoed (St Mary) Penhow (St John the Baptist) St Brides (St Bridget) Llanvaches (St Dubritius) Llandevaud (St Peter) Caldicot (St Mary the Virgin, St Marys Portskewett, St Marys Rogiet) Magor (Langstone Parish Church, St Cadwaladr, St Martin, St Mary Magdalene, St Marys Llanwern, St Marys Magor, St Marys