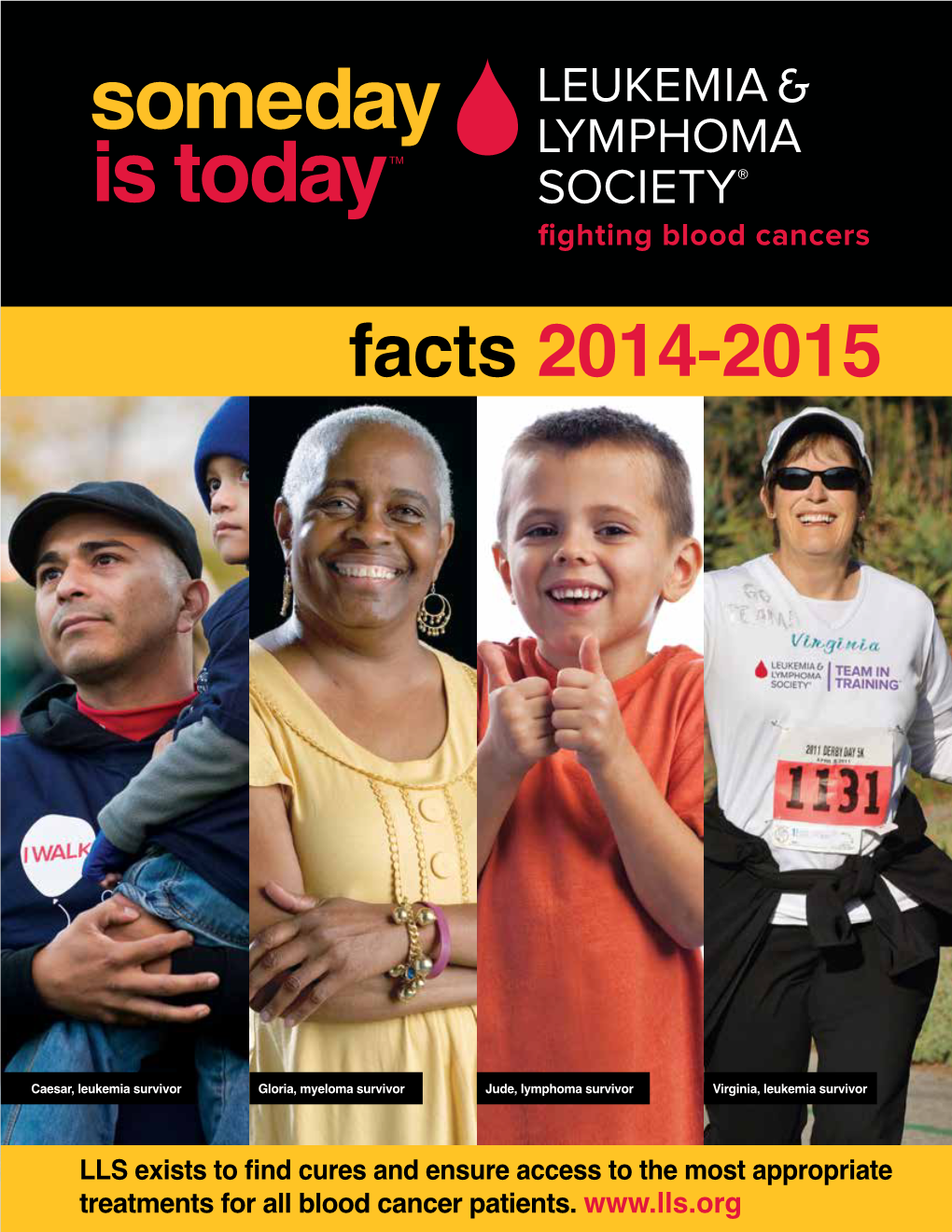
Facts 2014-2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LEUKERAN 3 (Chlorambucil) 4 Tablets 5
1 PRESCRIBING INFORMATION ® 2 LEUKERAN 3 (chlorambucil) 4 Tablets 5 6 WARNING 7 LEUKERAN (chlorambucil) can severely suppress bone marrow function. Chlorambucil is a 8 carcinogen in humans. Chlorambucil is probably mutagenic and teratogenic in humans. 9 Chlorambucil produces human infertility (see WARNINGS and PRECAUTIONS). 10 DESCRIPTION 11 LEUKERAN (chlorambucil) was first synthesized by Everett et al. It is a bifunctional 12 alkylating agent of the nitrogen mustard type that has been found active against selected human 13 neoplastic diseases. Chlorambucil is known chemically as 4-[bis(2- 14 chlorethyl)amino]benzenebutanoic acid and has the following structural formula: 15 16 17 18 Chlorambucil hydrolyzes in water and has a pKa of 5.8. 19 LEUKERAN (chlorambucil) is available in tablet form for oral administration. Each 20 film-coated tablet contains 2 mg chlorambucil and the inactive ingredients colloidal silicon 21 dioxide, hypromellose, lactose (anhydrous), macrogol/PEG 400, microcrystalline cellulose, red 22 iron oxide, stearic acid, titanium dioxide, and yellow iron oxide. 23 CLINICAL PHARMACOLOGY 24 Chlorambucil is rapidly and completely absorbed from the gastrointestinal tract. After single 25 oral doses of 0.6 to 1.2 mg/kg, peak plasma chlorambucil levels (Cmax) are reached within 1 hour 26 and the terminal elimination half-life (t½) of the parent drug is estimated at 1.5 hours. 27 Chlorambucil undergoes rapid metabolism to phenylacetic acid mustard, the major metabolite, 28 and the combined chlorambucil and phenylacetic acid mustard urinary excretion is extremely 29 low — less than 1% in 24 hours. In a study of 12 patients given single oral doses of 0.2 mg/kg of 30 LEUKERAN, the mean dose (12 mg) adjusted (± SD) plasma chlorambucil Cmax was 31 492 ± 160 ng/mL, the AUC was 883 ± 329 ng●h/mL, t½ was 1.3 ± 0.5 hours, and the tmax was 32 0.83 ± 0.53 hours. -

Chemotherapy in Advanced Ovarian Cancer: an Overview of Randomised Clinical Trials BMJ: First Published As 10.1136/Bmj.303.6807.884 on 12 October 1991
Chemotherapy in advanced ovarian cancer: an overview of randomised clinical trials BMJ: first published as 10.1136/bmj.303.6807.884 on 12 October 1991. Downloaded from Advanced Ovarian Cancer Trialists Group Abstract cytotoxic drugs, usually doxorubicin and cyclophos- Objectives-To consider the role of platinum and phamide with or without hexamethylmelamine.45 the relative merits of single agent and combination When, however, doubt was cast on the effectiveness chemotherapy in the treatment of advanced ovarian of doxorubicin by both randomised phase III trials6-8 cancer. and phase II studies in patients not responding to Design-Formal quantitative overview using cisplatin9 several major centres adopted cisplatin plus updated individual patient data from all available cyclophosphamide as standard. Furthermore, when randomised trials (published and unpublished). other trials failed to find significant survival differences Subjects-8139 patients (6408 deaths) included in between single agent cisplatin and cisplatin in combi- 45 different trials. nation with other drugs'0 some centres reverted to Results-No firm conclusions could be reached. using single agent platinum as routine first line treat- Nevertheless, the results suggest that in terms of ment. Recently a large number oftrials have compared survival immediate platinum based treatment was cisplatin with its less nephrotoxic and neurotoxic better than non-platinum regimens (overall relative analogue carboplatin, and although follow up times risk 0-93; 95% confidence interval 0-83 to 1-05); were often short, many institutions have now adopted platinum in combination was better than single agent carboplatin as standard. platinum when used in the same dose (overall Currently it is unclear what constitutes optimal relative risk 0-85; 0*72 to 1-00); and cisplatin and chemotherapy for advanced disease and treatment carboplatin were equally effective (overall relative strategies vary both nationally and internationally. -

Hematopoietic and Lymphoid Neoplasm Coding Manual
Hematopoietic and Lymphoid Neoplasm Coding Manual Effective with Cases Diagnosed 1/1/2010 and Forward Published August 2021 Editors: Jennifer Ruhl, MSHCA, RHIT, CCS, CTR, NCI SEER Margaret (Peggy) Adamo, BS, AAS, RHIT, CTR, NCI SEER Lois Dickie, CTR, NCI SEER Serban Negoita, MD, PhD, CTR, NCI SEER Suggested citation: Ruhl J, Adamo M, Dickie L., Negoita, S. (August 2021). Hematopoietic and Lymphoid Neoplasm Coding Manual. National Cancer Institute, Bethesda, MD, 2021. Hematopoietic and Lymphoid Neoplasm Coding Manual 1 In Appreciation NCI SEER gratefully acknowledges the dedicated work of Drs, Charles Platz and Graca Dores since the inception of the Hematopoietic project. They continue to provide support. We deeply appreciate their willingness to serve as advisors for the rules within this manual. The quality of this Hematopoietic project is directly related to their commitment. NCI SEER would also like to acknowledge the following individuals who provided input on the manual and/or the database. Their contributions are greatly appreciated. • Carolyn Callaghan, CTR (SEER Seattle Registry) • Tiffany Janes, CTR (SEER Seattle Registry) We would also like to give a special thanks to the following individuals at Information Management Services, Inc. (IMS) who provide us with document support and web development. • Suzanne Adams, BS, CTR • Ginger Carter, BA • Sean Brennan, BS • Paul Stephenson, BS • Jacob Tomlinson, BS Hematopoietic and Lymphoid Neoplasm Coding Manual 2 Dedication The Hematopoietic and Lymphoid Neoplasm Coding Manual (Heme manual) and the companion Hematopoietic and Lymphoid Neoplasm Database (Heme DB) are dedicated to the hard-working cancer registrars across the world who meticulously identify, abstract, and code cancer data. -

Waldenstro¨M's Macroglobulinemia Is a Biological Syndrome Which May
Correspondence 1637 cation,10 particularly in acute promyelocytic leukemia (APL), we References searched for genomic similarities. The few specific studies in existence on sequence analysis of the PML-RAR␣ gene show that the breakpoint within the involved gene (usually the PML locus) is variably situated, 1 Saglio G, Guerrasio A, Tassinari A, Ponzetto C, Zaccaria A, Testoni and that the corresponding fusion transcript should be aberrant. The P, Celso B, Rege Cambrin G, Serra A, Pegoraro L. Variability of the ␣ resulting PML-RAR proteins contained residues not homologous with molecular defects corresponding to the presence of a Philadelphia ␣ either PML or RAR . These reported atypical breaks were very similar chromosome in human hematologic malignancies. Blood 1988; to the one recorded in our case. A second original characteristic of 72: 1203–1208. the BCR break reported by us is that an intronic sequence derived 2 Chissoe SL, Bodenteich A, Wang YF, Wang YP, Burian D, Clifton from abl intron Ib was juxtaposed to bcr exon. This is another unpre- SW, Crabtree J, Freeman A, Iyer K, Jian L. Sequence and analysis cedented feature for a CML patient, although on rare occasions it has 10 of the human ABL gene, the BCR gene, and regions involved in been reported in AML patients. So, it may be speculated that in a the Philadelphia chromosomal translocation. Genomics 1995; 27: small proportion of the DNA breaks that occurs in leukemia, a cur- 67–82. rently unknown molecular mechanism could break the coding DNA. 3 Saglio G, Guerrasio A, Rosso C, Zaccaria A, Tassinari A, Serra A, The resulting RNA remains in-frame coding an aberrant or, as in our Rege-Cambrin G, Mazza U, Gavosto F. -
B. Package Leaflet
B. PACKAGE LEAFLET 1 Package Leaflet: Information for the User Chlorambucil 2 mg tablets chlorambucil Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions ask your doctor or nurse. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Chlorambucil is and what it is used for 2. What you need to know before you take Chlorambucil 3. How to take Chlorambucil 4. Possible side effects 5. How to store Chlorambucil 6. Contents of the pack and other information 1. What Chlorambucil is and what it is used for Chlorambucil contains a medicine called chlorambucil. This belongs to a group of medicines called cytotoxics (also called chemotherapy). Chlorambucil is used to treat some types of cancer and certain blood problems. It works by reducing the number of abnormal cells your body makes. Chlorambucil is used for: - Hodgkin's disease and Non-Hodgkin’s Lymphoma. Together, these form a group of diseases called lymphomas. They are cancers formed from cells of the lymphatic system. - Chronic lymphocytic leukaemia. A type of white blood cell cancer where the bone marrow produces a large number of abnormal white cells. -

Lymphoproliferative Disorders
Lymphoproliferative disorders Dr. Mansour Aljabry Definition Lymphoproliferative disorders Several clinical conditions in which lymphocytes are produced in excessive quantities ( Lymphocytosis) Lymphoma Malignant lymphoid mass involving the lymphoid tissues (± other tissues e.g : skin ,GIT ,CNS …) Lymphoid leukemia Malignant proliferation of lymphoid cells in Bone marrow and peripheral blood (± other tissues e.g : lymph nods ,spleen , skin ,GIT ,CNS …) Lymphoproliferative disorders Autoimmune Infection Malignant Lymphocytosis 1- Viral infection : •Infectious mononucleosis ,cytomegalovirus ,rubella, hepatitis, adenoviruses, varicella…. 2- Some bacterial infection: (Pertussis ,brucellosis …) 3-Immune : SLE , Allergic drug reactions 4- Other conditions:, splenectomy, dermatitis ,hyperthyroidism metastatic carcinoma….) 5- Chronic lymphocytic leukemia (CLL) 6-Other lymphomas: Mantle cell lymphoma ,Hodgkin lymphoma… Infectious mononucleosis An acute, infectious disease, caused by Epstein-Barr virus and characterized by • fever • swollen lymph nodes (painful) • Sore throat, • atypical lymphocyte • Affect young people ( usually) Malignant Lymphoproliferative Disorders ALL CLL Lymphomas MM naïve B-lymphocytes Plasma Lymphoid cells progenitor T-lymphocytes AML Myeloproliferative disorders Hematopoietic Myeloid Neutrophils stem cell progenitor Eosinophils Basophils Monocytes Platelets Red cells Malignant Lymphoproliferative disorders Immature Mature ALL Lymphoma Lymphoid leukemia CLL Hairy cell leukemia Non Hodgkin lymphoma Hodgkin lymphoma T- prolymphocytic -

| Lymphoproliferative Disorders
| Lymphoproliferative Hematology 438 teamwork disorders Color index: Red: Important Gray: notes Blue: extra Editing file Not malignant | definitions Lymphoproliferative disorders characters: -mature lymphocytes (no blasts), -lymphocytosis, Lymphoma -chronic. Lymphoid leukemia Several clinical conditions in Malignant proliferation of Malignant lymphoid mass which lymphocytes are lymphoid cells in Bone involving the lymphoid tissues produced in excessive marrow and peripheral blood (± other tissues ie; Extranodal quantities (Lymphocytosis) when the malignancy of lymphocytes reaches the lymphoma, by definition, involves sites other N.B: Lymphoproliferative disorders occur when the normal bone marrow or the peripheral blood we call it than lymph nodes, spleen, thymus and the mechanisms of control of proliferation of lymphocytes break lymphoid leukemia. pharyngeal lymphatic ring. e.g : skin down, resulting in autonomous, uncontrolled proliferation of lymphoid cells and typically leading to lymphocytosis and/or (± other tissues e.g : lymph ,GIT ,CNS) lymphadenopathy, and sometimes to involvement of extranodal sites, e.g. bone marrow. nodes ,spleen , skin ,GIT ,CNS) Autoimmune Infection Malignant Mostly virus Causes of lymphoproliferative disorder: These include (1) malignant—clonal in nature, resulting from the uncontrolled proliferation of a single transformed cell, e.g. lymphoma; (2) nonmalignant—polyclonal lymphoproliferative disorders may result from conditions including (a) infections—lymphocytosis is commonly caused by viral infections, e.g. Epsitein–Barr virus (EBV); lymphadenopathy is a common feature of a very wide variety of infections, (b) reactive—conditions such as systemic lupus erythematosus (SLE) and sarcoidosis frequently cause lymphadenopathy. | Lymphocytosis Blood film is very important, also Age is very important to expect the cause of lymphocytosis. Small lymphocytes: in non-infectious causes ●bacterial infection Some bacteria as ●Chronic lymphocytic ●Viral infection Pertussis ,brucellosis. -
Efficacy of Ethinylestradiol Re-Challenge for Metastatic Castration-Resistant Prostate Cancer
ANTICANCER RESEARCH 36: 2999-3004 (2016) Efficacy of Ethinylestradiol Re-challenge for Metastatic Castration-resistant Prostate Cancer TAKEHISA ONISHI1, TAKUJI SHIBAHARA1, SATORU MASUI1, YUSUKE SUGINO1, SHINICHIRO HIGASHI1 and TAKESHI SASAKI2 1Department of Urology, Ise Red Cross hospital, Ise, Japan; 2Department of Urology, Mie University Graduate School of Medicine, Tsu, Japan Abstract. Background: There has recently been renewed corticosteroids, estrogens, sipuleucel T and, more recently, interest in the use of estrogens as a treatment strategy for CYP17 inhibitor (abirateron acetate) and androgen castration-resistant prostate cancer (CRPC). The purpose of receptor antagonist (enzaltamide) (2-7). Treatment with this study was to evaluate the feasibility and efficacy of estrogens was used as a palliative therapy for advanced ethinylestradiol re-challenge (re-EE) in the management of prostate cancer, however, the discovery of luteinizing CRPC. Patients and Methods: Patients with metastatic CRPC hormone-releasing hormone (LH-RH) agonists led them to who received re-EE after disease progression on prior EE become less common and they stopped being used in most and other therapy were retrospectively reviewed for prostate- countries in the 1980s (8). One of the reasons for reduction specific antigen (PSA) response, PSA progression-free in their use is the risk of cardiovascular and survival (P-PFS) and adverse events. Results: Thirty-six re- thromboembolic events during therapy. However, several EE treatments were performed for 20 patients. PSA response reports demonstrated the positive oncological results of to the initial EE treatment was observed in 14 (70%) patients. therapy with estrogens, such as diethylstilbestrol (DES) PSA response to re-EE was 33.3% in 36 re-EE treatments. -

Hematologic Oncology Update — Issue 1, 2014
POST-TEST Hematologic Oncology Update — issue 1, 2014 The c o rrec T answer is indicaTed wiTh yellow highlighTin g. 1. Which of the following is true regarding the 6. A Phase II study of single-agent brentux- CRS related to CAR T-cell therapy? imab vedotin for the treatment of relapsed a. It manifests as fever, nausea, myalgia or refractory CD30-positive non-hodgkin and hypotension lymphomas demonstrated promising antitumor b. It is associated with high levels of IL-6 activity in patients with DLBCL with a broad c. It is irreversible range of CD30 expression levels. d. Both a and b a. True b. False 2. Updated results of a pilot trial by Porter and colleagues of chimeric antigen receptor T-cell 7. Results from a Phase II trial comparing therapy for patients with relapsed/refractory consolidation therapy with a single dose of CLL reported an overall response rate of 90y-ibritumomab tiuxetan to rituximab mainte- _____________. nance for patients with newly diagnosed Fl a. 12% who have experienced a response to r-CHOP b. 57% demonstrated statistically significant differ- ences in _____________ favoring rituximab c. 82% maintenance. 3. Tocilizumab, an IL-6 receptor antagonist, is a. Progression-free survival effective at reversing the cytokine release b. Overall survival syndrome associated with chimeric antigen c. Both a and b receptor-modified T-cell therapy. a. True 8. The final stage II results of the Phase b. False III CLL11 trial for patients with CLL and coexisting medical conditions demon- 4. The results of a Phase III study of induction strated that obinutuzumab/chlorambucil was therapy with lenalidomide and dexametha- superior to rituximab/chlorambucil in terms of sone followed by maintenance lenalidomide _____________. -

Essential Thrombocythemia Facts No
Essential Thrombocythemia Facts No. 12 in a series providing the latest information for patients, caregivers and healthcare professionals www.LLS.org • Information Specialist: 800.955.4572 Introduction Highlights Essential thrombocythemia (ET) is one of several l Essential thrombocythemia (ET) is one of a related “myeloproliferative neoplasms” (MPNs), a group of closely group of blood cancers known as “myeloproliferative related blood cancers that share several features, notably the neoplasms” (MPNs) in which cells in the bone “clonal” overproduction of one or more blood cell lines. marrow that produce the blood cells develop and All clonal disorders begin with one or more changes function abnormally. (mutations) to the DNA in a single cell; the altered cells in l ET begins with one or more acquired changes the marrow and the blood are the offspring of that one (mutations) to the DNA of a single blood-forming mutant cell. Other MPNs include polycythemia vera and cell. This results in the overproduction of blood cells, myelofibrosis. especially platelets, in the bone marrow. The effects of ET result from uncontrolled blood cell l About half of individuals with ET have a mutation production, notably of platelets. Because the disease arises of the JAK2 (Janus kinase 2) gene. The role that this from a change to an early blood-forming cell that has the mutation plays in the development of the disease, capacity to form red cells, white cells and platelets, any and the potential implications for new treatments, combination of these three cell lines may be affected – and are being investigated. usually each cell line is affected to some degree. -

VINBLASTINE-VINCRISTINE (Chlvpp-EVA
Chemotherapy Protocol LYMPHOMA CHLORAMBUCIL-DOXORUBICIN-ETOPOSIDE-PREDNISOLONE-PROCARBAZINE- VINBLASTINE-VINCRISTINE (ChlVPP-EVA) Regimen • Lymphoma – ChlVPP-EVA-Chlorambucil-Doxorubicin-Etoposide-Prednisolone- Procarbazine-Vinblastine-Vincristine Indication • Hodgkin’s Lymphoma Toxicity Drug Adverse Effect Chlorambucil Gastro-intestinal disturbance Doxorubicin Cardiomyopathy, alopecia, urinary discolouration (red) Etoposide Hypotension on rapid infusion, hyperbilirubinaemia Weight gain, gastro-intestinal disturbances, hyperglycaemia, Prednisolone CNS disturbances, cushingoid changes, glucose intolerance Procarbazine Insomnia, ataxia, hallucinations, headache Vinblastine Peripheral neuropathy, constipation, jaw pain, ileus Vincristine Peripheral neuropathy, constipation, jaw pain, ileus The adverse effects listed are not exhaustive. Please refer to the relevant Summary of Product Characteristics for full details. Patients diagnosed with Hodgkin’s Lymphoma carry a lifelong risk of transfusion-associated graft versus host disease (TA-GVHD). Where blood products are required these patients must receive only irradiated blood products for life. Local blood transfusion departments must be notified as soon as a diagnosis is made and the patient must be issued with an alert card to carry with them at all times. Monitoring Drugs • FBC, LFTs and U&Es prior to day one and eight of treatment Version 1 (May 2018) Page 1 of 10 Lymphoma- ChlVPP-EVA-Chlorambucil-Doxorubicin-Etoposide-Prednisolone-Procarbazine-Vinblastine-Vincristine Dose Modifications The dose modifications listed are for haematological, liver and renal function and limited drug specific toxicities. Dose adjustments may be necessary for other toxicities as well. In principle all dose reductions due to adverse drug reactions should not be re-escalated in subsequent cycles without consultant approval. It is also a general rule for chemotherapy that if a third dose reduction is necessary treatment should be stopped. -

Predictive Significance of the Cut-Off Value of CD20 Expression in Patients with B-Cell Lymphoma
1101-1107.qxd 25/8/2010 12:26 ÌÌ ™ÂÏ›‰·1101 ONCOLOGY REPORTS 24: 1101-1107, 2010 Predictive significance of the cut-off value of CD20 expression in patients with B-cell lymphoma MATEJA HORVAT1, VERONIKA KLOBOVES PREVODNIK2, JAKA LAVRENCAK2 and BARBARA JEZERSEK NOVAKOVIC3 1Bayer d.o.o., Bravnicarjeva 13; Departments of 2Cytopathology, 3Medical Oncology, Institute of Oncology Ljubljana, Zaloska 2, 1000 Ljubljana, Slovenia Received May 25, 2010; Accepted July 15, 2010 DOI: 10.3892/or_00000961 Abstract. The introduction of the anti-CD20 monoclonal 0.5667; 95%CI, 0.124 to 3.18, p=0.57]. Even though we have antibody, rituximab, into the treatment of patients with B-cell proved that patients with a CD20 expression level above the lymphomas has improved the overall response rate, as well as cut-off value treated with rituximab had a significantly longer the response duration and the overall survival of these patients. OS [hazard ratio (HR), 0.4573; 95%CI, 0.1364 to 0.9461, However, only a few studies have addressed the question of p=0.0383] than patients with a CD20 expression level below whether higher CD20 expression parallels with better treatment the cut-off value. Among our study population, 17.5% had a outcomes. The aim of this study was to assess the relationship CD20 expression level below the cut-off value. The highest between the level of CD20 expression and overall survival percentage (80%) of the patients with a CD20 expression (OS), disease-free survival (DFS) along with the overall level below the cut-off value belonged to the group of chronic response rate (ORR) in B-cell lymphoma patients.