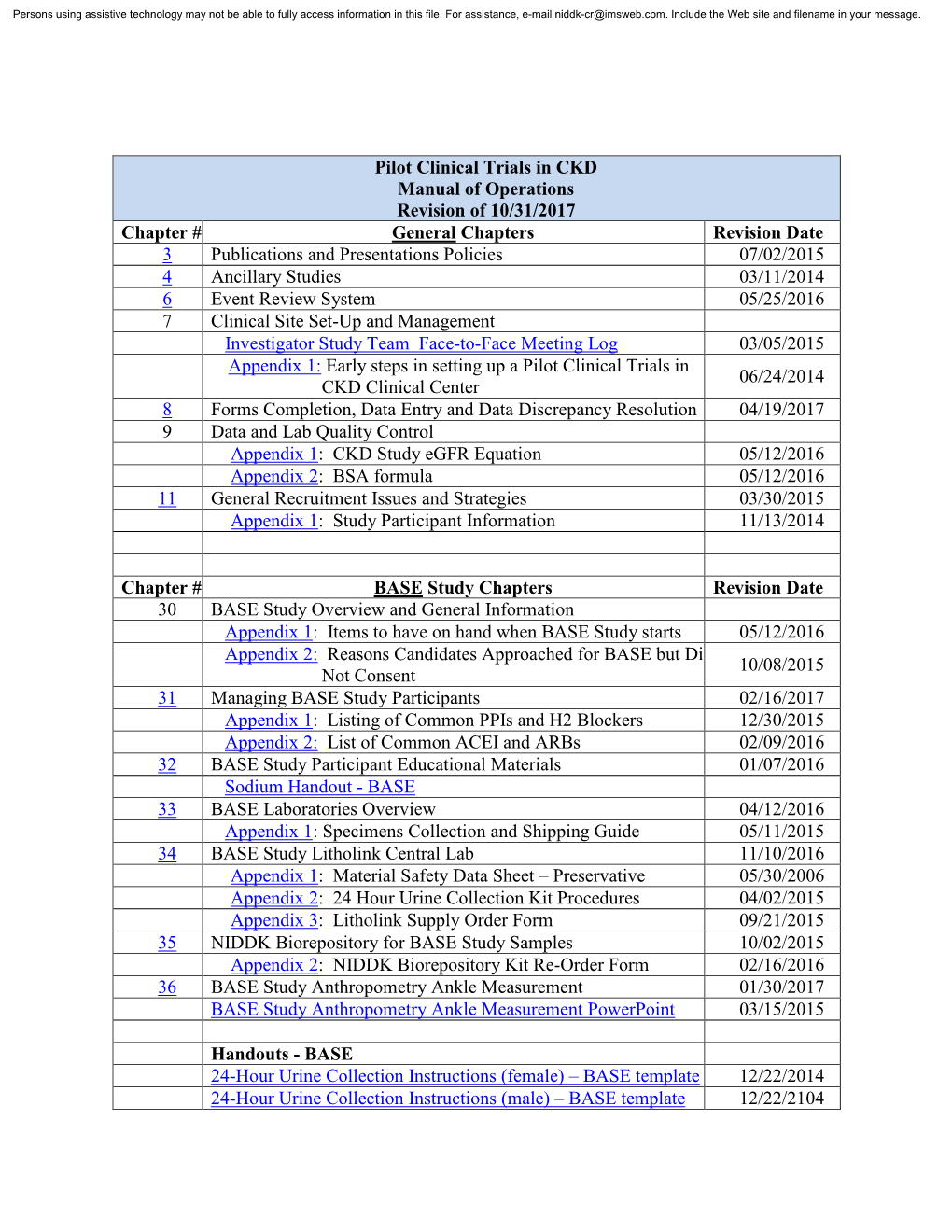
Manual of Procedures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SEABIRD TISSUE ARCHIVAL and MONITORING PROJECT: Protocol for Collecting and Banking Seabird Eggs
OCS Study, MMS 2001-031 NISTIR6735 SEABIRD TISSUE ARCHIVAL AND MONITORING PROJECT: Protocol for Collecting and Banking Seabird Eggs Geoff Weston York Barbara J. Porter Rebecca S. Pugh Da vid G. Roseneau Kristin Simac Paul R. Becker Lyman K. Thorsteinson and Stephen A. Wise e•• •• NlST • ,;) g Nation<:d Institute of Standards and Techn.:>logy Technoio9Y AdminIstration, U.S. Department of Commerce NIST CENTENNIAL. , DCS Study, MMS 2001-031 NISTIR6735 SEABIRD TISSUE ARCHIVAL AND MONITORING PROJECT: Protocol for Collecting and Banking Seabird Eggs Geoff Weston York' Barbara J. Porter Rebecca S. Pugh' David G. Roseneau' Kristin Simac I Paul R. Becker' Lyman K. Thorsteinson" and Stephen A. Wise2 IU.S. Department of the Interior U.S. Geological Survey Alaska Biological Resources Center 2National Institute of Standards and Technology Chemical Science and Technology Laboratory 3U.S. Department of the Interior U.S. Fish and Wildlife Service Alaska Maritime National Wildlife Refuge 4U.S. Department of the Interior U.S. Geological Survey Biological Resources Division - Western Office April 2001 ~USGS scilmce tor" challfJing womJ U.S. Department of Commerce Donald L Evans, Secretary National Institute of Standards and Technology Karen H. Brown, Acting Director CONTENTS page List of Tables .iii List of Figures .iii Acknowledgments iv Disclaimer v INTRODUCTION '" 1 Environmental Specimen Banking 1 Project Goal and Objectives................................................................................................. 2 Banking Seabird Eggs 2 MANAGEMENT SySTEM 6 MA TERIALS 8 Materials Required for Collecting Eggs and Shipping them to the Processing Laboratory... 8 Materials Required for Processing Eggs 8 Materials Required for Packaging Samples and Shipping Them to the Specimen Bank. 9 Seabird Data Form 9 METHODS 15 Egg Collection Field Procedures 15 Egg Processing Laboratory Procedures. -

Installation Tips
Installation Tips Important Please Read Before Going Further! Installation of Kitchen Cabinets is NOT a Do-It-Yourself project for those without extensive experience in finish carpentry. If you are not a professional carpenter please seek help from a trained professional. This guide is meant to be used as a supplement to carpenters who are trained and familiar with cabinetry installa- tion techniques, it is not meant to be a stand alone installation guide. Version 1.0 - 2009 CABINET INSTALLATION TABLE OF CONTENTS Cabinet installation requires special skills and tools. If you are COMMON INSTALLATION TOOLS uncertain of any part of these basic instructions, terms or lack the minimum listed tools, consult with your cabinet supplier For professional results have the tools you need at hand and for recommended professional cabinet installation mechanics. ready. Here’s a tip: save changeover time by having two An error during installation can result in costly repairs and cordless screwguns – one with a drill bit for predrilling screw delays. holes and another with a screw tip. TERMS TO KNOW • Power Drill • Sand Paper • Drill Bits • Block Plane • Terms and Tools Level: A horizontal plane at right angles to the plumb. • Carpenter’s Levels (2’ & 4’) • Clamps • Carpenter’s Square • Caulking Plumb: A true vertical line. If something is “out of plumb” it •Tape Measure (1”x25’) • Chalk Line is not exactly straight up and down. • Step ladder • Mitre Box • Common Construction Details • Nail Set • Marking Tools Square: All lines parallel and at 90° to each other. • Extension Cord(s) • Stud Finder Rail: A horizontal framing member of a cabinet door. -
Grease Sampling Kit for Pillow Block Bearings MGT-01-008
Grease Sampling Kit for Pillow Block Bearings MGT-01-008 Directions for sampling with the Grease Thief from Pillow Block Bearings: Enclosed in the kit: • Eight (8) sleeves containing: - One (1) 10cc plastic syringe - One (1) plastic spatula - One (1) Grease Thief with yellow cap - One (1) Shipping Tube - One (1) Blank Equipment Label • One (1) shipping envelopes 1. Remove yellow cap from Grease Thief and place back into bag to keep clean. 2. Remove plunger from syringe and place back into bag to keep clean 3. Use wide end of spatula to remove any dirt or debris. 4. Use narrow end of spatula to sample grease from desired test area 5. Place grease from spatula into plastic syringe. Approximately 1.5 grams of grease or about 2 cc are needed to completely fill the Grease Thief. 6. Inject the grease from the syringe into the Grease Thief to push the plunger to the far end as the grease fills the body. The Grease Thief is completely full when the grease just begins to exit at the relief holes. While grease is being added, it is necessary to slowly withdraw the syringe tip from within the Grease Thief body to completely fill the open end. BODY OPEN END PISTON BODY HANDLE END BARB 7. Prior to placing the yellow cap onto the Grease Thief for shipment, purge a small por- tion of the grease from the Grease Thief into the yellow cap to relieve any pressure build up from placing the cap on the full Grease Thief. 8. Once a small portion of the grease is in the yellow cap, firmly place the yellow cap on the Grease Thief. -

OP10-1003 Qxq
WOMEN’S INTERAGENCY HIV STUDY ORAL PROTOCOL FORM OP10: SUBGINGIVAL PLAQUE SAMPLES COMLETING THE FORM GENERAL INFORMATION Affix the Participants ID label in the space indicated. Record the visit number, which should be the same as the WIHS core visit. Be sure the form version is the most current version date. Record your initials. Record the date. SUBGINGIVAL PLAQUE SAMPLES If participant if edentulous (OP 6 #1 is coded as 1). Form OP 10 is left blank. 1. Indicate if specimens were collected for positive gingival banding scores on the facial or lingual aspects. 1a. Record the tooth number from which these samples were collected. 2. Indicate if specimens were collected from papilla sites with scores of 3 or 5. 2a. Record the tooth numbers (i.e., the most mesial tooth bounding the interdental space) from which the sample was collected. 2b. Indicate the Papillary Assessment score associated with the sample by circling the appropriate code. 3. These samples should be taken at all visits. Indicate if samples were taken from sites exhibiting a ≥ 2mm change in attachment since the WIHS Oral visit prior to last. 3a. Indicate the tooth numbers from which these samples were taken. Refer to samples in the appendix section of this manual for the complete and proper way to fill out the laboratory request forms that are to accompany each plaque sample collected and shipped to the lab. All three copies of the triplicate should be sent with the specimen. EQUIPMENT • Fine sterile paper points • Cotton rolls • Sterile curette • Sterile cotton forceps • 4 vials (2 plastic vials for PCR analysis and 2 glass vials with anaerobic medium) for affected site. -

PREFERRED PACKAGING: Accelerating Environmental Leadership in the Overnight Shipping Industry
PREFERRED PACKAGING: Accelerating Environmental Leadership in the Overnight Shipping Industry A Report by The Alliance for Environmental Innovation A Project of the Environmental Defense Fund and The Pew Charitable Trusts The Alliance for Environmental Innovation The Alliance for Environmental Innovation (the Alliance) is a joint initiative of the Environmental Defense Fund (EDF) and The Pew Charitable Trusts. The Alliance works cooperatively with private businesses to reduce waste and build environmental considerations into business decisions. By bringing the expertise and perspective of environmental scientists and economists together with the business skills of major corporations, the Alliance creates solutions that make environmental and business sense. Author This report was written by Elizabeth Sturcken. Ralph Earle and Richard Denison provided guidance and editorial review. Acknowledgments Funding for this report was provided by The Pew Charitable Trusts, the Environmental Protection Agency’s WasteWi$e Program and Office of Pollution Prevention, and the Emily Hall Tremaine Foundation. Disclaimer This report was prepared by the Alliance for Environmental Innovation to describe the packaging practices of the overnight shipping industry and identify opportunities for environmental improvement. Copyright of this report is held by the Alliance for Environmental Innovation. Any use of this report for marketing, advertising, promotional or sales purposes, is expressly prohibited. The contents of this report in no way imply endorsement of any company, product or service. Trademarks, trade names and package designs are the property of their respective owners. Ó Copyright The Alliance for Environmental Innovation The Alliance for Environmental Innovation is the product of a unique partnership between two institutions that are committed to finding cost-effective, practical ways to help American businesses improve their environmental performance. -

Method TO-11A
EPA/625/R-96/010b Compendium of Methods for the Determination of Toxic Organic Compounds in Ambient Air Second Edition Compendium Method TO-11A Determination of Formaldehyde in Ambient Air Using Adsorbent Cartridge Followed by High Performance Liquid Chromatography (HPLC) [Active Sampling Methodology] Center for Environmental Research Information Office of Research and Development U.S. Environmental Protection Agency Cincinnati, OH 45268 January 1999 Method TO-11A Acknowledgements This Method was prepared for publication in the Compendium of Methods for the Determination of Toxic Organic Compounds in Ambient Air, Second Edition (EPA/625/R-96/010b), which was prepared under Contract No. 68-C3-0315, WA No. 3-10, by Midwest Research Institute (MRI), as a subcontractor to Eastern Research Group, Inc. (ERG), and under the sponsorship of the U.S. Environmental Protection Agency (EPA). Justice A. Manning, John O. Burckle, and Scott Hedges, Center for Environmental Research Information (CERI), and Frank F. McElroy, National Exposure Research Laboratory (NERL), all in the EPA Office of Research and Development, were responsible for overseeing the preparation of this method. Additional support was provided by other members of the Compendia Workgroup, which include: • John O. Burckle, U.S. EPA, ORD, Cincinnati, OH • James L. Cheney, Corps of Engineers, Omaha, NB • Michael Davis, U.S. EPA, Region 7, KC, KS • Joseph B. Elkins Jr., U.S. EPA, OAQPS, RTP, NC • Robert G. Lewis, U.S. EPA, NERL, RTP, NC • Justice A. Manning, U.S. EPA, ORD, Cincinnati, OH • William A. McClenny, U.S. EPA, NERL, RTP, NC • Frank F. McElroy, U.S. EPA, NERL, RTP, NC • Heidi Schultz, ERG, Lexington, MA • William T. -

Shipping and Transport Media 10
Shipping and Transport Media 10 10.1 Product Transport Media All semiconductor products must be shipped in some type of handling media. The type used is specific to the type of package, die, or wafer that is to be shipped. The following sections outline the many different types of shipping and handling media that Intel uses and outlines how they can be recycled. This is not inclusive of the many different types of media available, but is meant to show the main types used and some of the methods for using them in the factory floor. 10.1.1 Plastic Tubes Plastic shipping and handling tubes are manufactured from polyvinyl chloride (PVC) with an antistatic surfactant treatment. Standard tubes for most package types are translucent and allow visual inspection of units within the tube. Carbon-impregnated, black conductive tubes are available for all parts where required by device or use characteristics. Tube profiles are designed with minimum clearance over the maximum package dimensions to reduce damage caused by movement of the device within the tube. For some package types, tubes have “riding rails” on which the packages rest while in the tube. The rails protect the fragile leads from touching anything in the tube. PVC tacks, nylon tacks, or rubber plugs are used to retain the units. All tube wall thickness are 0.025 inches to 0.040 inches. Table 10-1 through Table 10-8 show tube dimensions and cross- sections and quantity of packages per tube for most Intel package types. Additional information on new packages should be requested through Intel Field Sales. -
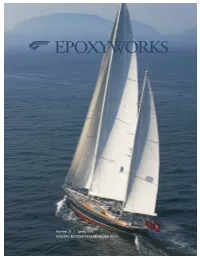
Epoxyworks 23 Is Also Available As A
® EPOXYWORKS ® Number 23 n Spring 2006 BUILDING, RESTORATION & REPAIR with EPOXY Onne van der Wal In this issue EPOXYWORKS® 1 Scheherazade update Editors Kay Harley, Jennifer Jones A late look at the Hodgdon-built, Bruce King-de- Designer Michael Barker signed, 154' ketch. Subscriptions Kristen Lore 2 The limitations of statues What to do when your shepherd gets cold feet and Contributors W. D. Bertelsen, Tim Botimer, Jason Havel, falls apart under a little stress. Brian Knight, Bruce Niederer, Tom Pawlak, Patrick Ropp, 4 Fabricating an air scoop J. R. Watson and Jeff Wright Using the “lost foam” method to build a custom air Epoxyworks is published twice a year by Gougeon Brothers, scoop for a race car. Inc.,BayCity,MIUSA. 6 Building a masthead fitting Product number 000-605 Building a custom sailboat part with a molded cavity also using the “lost foam” method. ©2006 by Gougeon Brothers, Inc. Reproduction in any form, in whole or in part, is expressly forbidden without the 8 If you can’t take the heat... written consent of the publisher. An explanation of the effects of high temperatures on cured epoxy and what HDUL really means. Epoxyworks, Gougeon Brothers, WEST SYSTEM,105, 205, 206, 207, 209, 403, 404, 405, 406, 407, 410, Episize, Scarffer, and 10 Rebuilding an International 110 Microlight as used throughout this publication are trade- Tim Botimer wins a national championship after re- marks of Gougeon Brothers, Inc. building a 110 that sailed in the 1941 Nationals. Subscriptions, US and Canada Epoxyworks subscriptions 12 Readers’ projects are FREE to US and Canadian addresses only. -

Transport Media and Packing
2 10 Transport Media and Packing 1/16/97 5:51 PM CH10WIP.DOC INTEL CONFIDENTIAL (until publication date) 2 CHAPTER 10 TRANSPORT MEDIA AND PACKING 10.1. TRANSPORT MEDIA 10.1.1. Tubes Plastic shipping and handling tubes are manufactured from polyvinyl chloride (PVC) with an antistatic surfactant treatment. Standard tubes for most package types are translucent and allow visual inspection of units within the tube. Carbon-impregnated, black conductive tubes are available for all parts, where required by device or use characteristics. Tube profiles are designed with minimum clearance over the maximum package dimensions to reduce damaging movement of the device within the tube. For some package types, tubes have “riding rails” on which the packages rest while in the tube. The rails protect the fragile leads from touching anything in the tube. Nylon tacks, or rubber plugs are used to retain the units. All tube wall thickness are 0.025 in. to 0.040 in. Table 10-1 through Table 10-8 show tube dimensions, cross-sections and quantity per tube for most Intel package types. Further information on new packages should be requested through Intel Field Sales. 10-1 1/16/97 5:51 PM CH10WIP.DOC INTEL CONFIDENTIAL (until publication date) TRANSPORT MEDIA AND PACKING 2 Table 10-1. PLCC Shipping Tube Dimensions (In Inches) Cross Quantity Lead Section Wall Outside Dimensions Per Type (W x H) Thickness Length (L) Width (W) Height (H) Tube 20 L Square 0.030 19.375 0.480 0.263 46 28L Square 0.030 19.375 0.580 0.263 37 44L Square 0.025 19.375 0.780 0.250 26 52L Square 0.030 19.375 0.880 0.263 23 68L Square 0.025 19.375 1.090 0.250 18 28L Rectangular 0.025 19.375 0.480 0.220 30 32L Rectangular 0.025 19.375 0.580 0.220 30 84L Square 0.040 19.375 1.300 0.288 15 10-2 1/16/97 5:51 PM CH10WIP.DOC INTEL CONFIDENTIAL (until publication date) 2 TRANSPORT MEDIA AND PACKING Table 10-2. -

Paint Product Catalog 2019 5720 0116
Paint Product Catalog 2019 Festool USA LLC 400 N. Enterprise Blvd. Lebanon, IN 46052 Customer Service & Product Questions Tel 888.337.8600 festoolpaint.com Festool USA Paint Product Catalog 2019 5720 0116 Festool is not responsible for typographical errors. Printed in the USA Paint Product Catalog 2019 FESTOOL SERVICE ALL- purchaser. Warranty returns will be processed Instruction Manual ® by Festool according to normal work flow and INCLUSIVE Limited Warranty availability of replacement parts and components. Warning Festool USA warrants that all new Festool Festool will issue a prepaid shipping label for To reduce the risk of personal injury and power tools1 purchased from authorized dealers return of the tool to the Festool Service Center for best optimum tool performance, be in the U.S. and Canada will be free from defects and will also return the repaired tool freight sure to read, understand, and follow all in materials and workmanship for a term of prepaid, if the repair or replacement is covered the safety and operating instructions in the three years from the date of original retail under this Limited Warranty. instruction manual before using the tool. An purchase. instruction manual is furnished with every FESTOOL SHALL NOT BE LIABLE FOR ANY tool. If yours is lost or if you have questions, Conditions of the SERVICE ALL-INCLUSIVE® CONSEQUENTIAL, INCIDENTAL OR SPECIAL please call 888.337.8600 for a replacement. Limited Warranty are as follows: DAMAGES REGARDLESS OF THE THEORY OF LAW ON WHICH THE CLAIM IS BASED. ALL Health Warning This warranty applies for three years from the WARRANTIES IMPLIED BY STATE LAW, Various dusts created by power sanding, date of original retail purchase. -

Specimen Collection and Transport Products Catalog
Specimen Collection and Transport Products Catalog Featuring An Introduction to Global Kitting Management: • Client Supply Services • Clinical Trial Services therapaksg.com 2 Global Kitting Management Client Supply Services Serving hundreds of Personalized Medicine companies, Reference Laboratories, Hospital Outreach Laboratories and Pathology Testing organizations, Therapak is the preferred supplier for kit development, commercial launch and order management and tracking programs. Kit Development Therapak’s team of experienced professionals, armed with a broad base of over 3,000 component products, will work closely with customers to address every aspect of their kit supply needs and ensure timely delivery of supplies to meet project launch timelines. Production Having produced over 100 million kits, Therapak is the Global Leader in regulated kit production across all clinical and commercial disciplines. Our systems are designed to accommodate batch sizes as small as a single clinical trial visit-specific kit to those as large as several thousand repetitive commercial kits. Printing In addition to accommodating your kit supply needs, Therapak provides a complete solution for your printing needs, including: preparation of customized and branded Laboratory Requisition Forms and Booklets, on demand printing of site-specific Requisition Forms and on demand printing of site-specific shipping documents. Quality Assurance Therapak’s quality system operates in accordance to the United States Food and Drug Administration’s current Good Manufacturing Practices for medical devices - 21 CFR § 820; Singapore HSA’s TS-01 - Good Distribution Practices for Medical Devices and Good Assembly Practices; and Article 12 of Council Directive 93/42/EEC concerning medical devices. Ordering Therapak’s Client Supply Express (CSE) Online ordering software intelligently manages the ordering process using Kit-Track ID technology to maintain full visibility of the kit lifecycle. -

Custom Products Pictured in This Catalog
Who We Are Popcorn is a reliable Design & Manufacturing Partner for the Museum Store Marketplace. Popcorn is driven by a small team of Craftsmen and Skilled Designers who specialize in Product Development and Turn-Key Museum Programs. Popcorn is skilled in the Vanishing Art of Manufacturing—our Premium Products are all Made in America. Five Core Museum Products We specialize in 5 core products: Magnets / Matted Prints / Note Cards / Phone Covers / Mugs From beginning to end, Popcorn delivers a perfectly designed and color matched merchandise program. This year we introduced many new custom products pictured in this catalog. Many are great impulse items that are great for the holidays: Glass Ornaments / Journals / Messenger Bags / Pet Bowls / Dog Tags / Luggage Tags / Key Chains. More new products will be introduced during the coming year and can be seen on our website: www.popcornposters.com/custom Program Basics Minimums: Most products are 24 pc minimum Discounts*: 10% off 144 pc orders 15% off 288 pc orders *some products have diff erent discounts Lead Time: Designed, manufactured and shipped within 3 weeks. Reorders generally ship within 3 days! Mission Specifi c Merchandise / Award Winning Design We fulfi ll your museum store mission by developing product that provides your visitors a range of customized, educational products. Our award winning packaging translates into more sales per visitor and provides great branding opportunities for your museum. We assign a team of graphic designers and writers to help tell your story—they bring a wide range of creativity and experience to every project. Popcorn’s Museum Program: Simple & Exceptional 1.