UI Thesis Dipeolu IO Effect 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

AFRREV STECH, Vol. 3(2) May, 2014
AFRREV STECH, Vol. 3(2) May, 2014 AFRREV STECH An International Journal of Science and Technology Bahir Dar, Ethiopia Vol. 3 (2), S/No 7, May, 2014: 51-65 ISSN 2225-8612 (Print) ISSN 2227-5444 (Online) http://dx.doi.org/10.4314/stech.v3i2.4 THE USE OF COMPOSITE WATER POVERTY INDEX IN ASSESSING WATER SCARCITY IN THE RURAL AREAS OF OYO STATE, NIGERIA IFABIYI, IFATOKUN PAUL Department of Geography and Environmental Management, Faculty of Social Sciences University of Ilorin; Ilorin, Kwara State, Nigeria E-mail: 234 8033231626 & OGUNBODE, TIMOTHY OYEBAMIJI Faculty of Law Bowen University, Iwo Osun State, Nigeria Abstract Physical availability of water resources is beneficial to man when it is readily accessible. Oyo State is noted for abundant surface water and appreciable groundwater resources in its pockets of regolith aquifers; as it has about eight months of rainy season and a relatively deep weathered regolith. In spite of this, cases of water associated diseases Copyright© IAARR 2014: www.afrrevjo.net 51 Indexed and Listed in AJOL, ARRONET AFRREV STECH, Vol. 3(2) May, 2014 and deaths have been reported in the rural areas of the state. This study attempts to conduct an investigation into accessibility to potable water in the rural areas of Oyo State, Nigeria via the component approach of water poverty index (WPI). Multistage method of sampling was applied to select 5 rural communities from 25 rural LGAs out of the 33 LGAs in the State. Data were collected through the administration of 1,250 copies of questionnaire across 125 rural communities. Component Index method as developed by Sullivan, et al (2003) was modified and used in this study. -
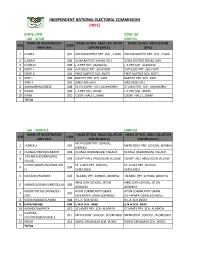
State: Oyo Code: 30 Lga : Afijio Code: 01 Name of Registration Name of Reg
INDEPENDENT NATIONAL ELECTORAL COMMISSION (INEC) STATE: OYO CODE: 30 LGA : AFIJIO CODE: 01 NAME OF REGISTRATION NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE AREA (RA) CENTRE (RACC) (RAC) 1 ILORA I 001 OKEDIJI BAPTIST PRY. SCH., ILORA OKEDIJI BAPTIST PRY. SCH., ILORA 2 ILORA II 002 ILORA BAPTIST GRAM. SCH. ILORA BAPTIST GRAM. SCH. 3 ILORA III 003 L.A PRY SCH. ALAWUSA. L.A PRY SCH. ALAWUSA. 4 FIDITI I 004 CATHOLIC PRY. SCH FIDITI CATHOLIC PRY. SCH FIDITI 5 FIDITI II 005 FIRST BAPTIST SCH. FIDITI FIRST BAPTIST SCH. FIDITI 6 AWE I 006 BAPTIST PRY. SCH. AWE BAPTIST PRY. SCH. AWE 7 AWE II 007 AWE HIGH SCH. AWE HIGH SCH. 8 AKINMORIN/JOBELE 008 ST.JOHN PRY. SCH. AKINMORIN ST.JOHN PRY. SCH. AKINMORIN 9 IWARE 009 L.A PRY SCH. IWARE. L.A PRY SCH. IWARE. 10 IMINI 010 COURT HALL 1, IMINI COURT HALL 1, IMINI TOTAL LGA : AKINYELE CODE: 02 NAME OF REGISTRATION NAME OF REG. AREA COLLATION NAME OF REG. AREA COLLATION S/N CODE AREA (RA) CENTRE (RACC) CENTRE (RACC) METHODIST PRY. SCHOOL, 1 IKEREKU 001 METHODIST PRY. SCHOOL, IKEREKU IKEREKU 2 OLANLA/OBODA/LABODE 002 OLANLA (OGBANGAN) VILLAGE OLANLA (OGBANGAN) VILLAGE EOLANLA (OGBANGAN) 3 003 COURT HALL ARULOGUN VILLAGE COURT HALL ARULOGUN VILLAGE VILLAG OLODE/AMOSUN/ONIDUND ST. LUKES PRY. SCHOOL, ST. LUKES PRY. SCHOOL, 4 004 U ONIDUNDU ONIDUNDU 5 OJO-EMO/MONIYA 005 ISLAMIC PRY. SCHOOL, MONIYA ISLAMIC PRY. SCHOOL, MONIYA ANGLICAN SCHOOL, OTUN ANGLICAN SCHOOL, OTUN 6 AKINYELE/ISABIYI/IREPODUN 006 AGBAKIN AGBAKIN IWOKOTO/TALONTAN/IDI- AYUN COMMUNITY GRAM. -

Assessment of Factors Influencing the Saving Culture Among Rural Households in Ibarapa East Local Government of Oyo State, Nigeria
Yusuf et al., 2020 Journal of Research in Forestry, Wildlife & Environment Vol. 12(1) December, 2020 E-mail: [email protected]; [email protected] http://www.ajol.info/index.php/jrfwe 156 jfewr ©2020 - jfewr Publications This work is licensed under a ISBN: 2141 – 1778 Creative Commons Attribution 4.0 License Yusuf et al., 2020 ASSESSMENT OF FACTORS INFLUENCING THE SAVING CULTURE AMONG RURAL HOUSEHOLDS IN IBARAPA EAST LOCAL GOVERNMENT OF OYO STATE, NIGERIA * Yusuf, 1W.A. Yusuf2 , S. A., Adesope3 A. A. A. and Adebayo, A. A. 2 *1Department of Economics, Nile University of Nigeria, FCT Abuja, Nigeria 2Department of Agricultural Economics, University of Ibadan, Ibadan Nigeria 3Forestry Research Institute of Nigeria, Jericho Ibadan, Oyo State, Nigeria *Corresponding Author Email: [email protected] ABSTRACT The study determined the saving culture of rural households in Ibarapa East Local Government of Oyo State. A multi-stage sampling technique was used to select 200 respondents for the study and questionnaire was used to elicit information from the respondents. Descriptive statistics and Probit regression were used to analyse the data. The result shows that the mean household size was 7, an indication of a relatively large average household size. The result of Probit regression shows a positive relationship between the income of respondents and their participation in commercial banks. However, participation of the respondents in Bank of Agriculture (BOA) is very low due to their poor awareness of the program. The result also reveals that distant to commercial banks, collateral and high interest rate hampered the respondents’ access to loan. The study recommends that activities of unorganized rural bank should be strengthened by the Government. -

(GIS) in Oyo State, Nigeria
Journal of Geography, Environment and Earth Science International 11(1): 1-15, 2017; Article no.JGEESI.34634 ISSN: 2454-7352 Mapping Groundwater Quality Parameters Using Geographic Information System (GIS) in Oyo State, Nigeria T. O. Ogunbode 1* and I. P. Ifabiyi 2 1Faculty of Basic Medical and Health Sciences, Bowen University, Iwo, Nigeria. 2Department of Geography and Environmental Management, University of Ilorin, Nigeria. Authors’ contributions This work was carried out in collaboration between both authors. Both authors read and approved the final manuscript. Article Information DOI: 10.9734/JGEESI/2017/34634 Editor(s): (1) Wen-Cheng Liu, Department of Civil and Disaster Prevention Engineering, National United University, Taiwan and Taiwan Typhoon and Flood Research Institute, National United University, Taipei, Taiwan. Reviewers: (1) H. O. Nwankwoala, University of Port Harcourt, Nigeria. (2) Dorota Porowska, University of Warsaw, Poland. Complete Peer review History: http://www.sciencedomain.org/review-history/20122 Received 2nd June 2017 th Original Research Article Accepted 9 July 2017 Published 19 th July 2017 ABSTRACT The knowledge of spatial pattern of groundwater quality is important to ensure a holistic approach to the management of the resource quality status in space and time. Thus a sample each of underground water was collected from each of the selected 5 rural communities in each of the selected 25 out of the 33 LGAs in Oyo State for the purpose of quality assessments. Eleven (11) + parameters namely water temperature (°C), pH, electr ical conductivity (EC), Sodium (Na ), SO 4, + Potassium (K ), Nitrate (NO 3), Phosphate (PO 3), coli-form count, Oxidation Redox Potential (ORP) and Total Dissolved Solids (TDS) were subjected to standard laboratory analysis. -

7.Results of Geophysical Survey
7.Results of Geophysical Survey 1. General 1-1 Purpose of Geophysical Survey The purpose of the geophysical survey is to find the promising communities with high potential ground water development. 1-2 Contents of geophysical survey -1st Stage (BD1) The geophysical survey was conducted in 100 communities of high priority selected among 220 communities -2nd stage(BD2) 56 communities among 100 communities were analyzed as low potential water development in 1st stage. The geophysical re-survey conducted at these 56 communities and in the new 17 additional communities. Total of geophysical survey including re-survey is 117communities (173 sites). ① Electromagnetic Survey ・Method :Loop-Loop (Srigram) ・Line :more than200 m(5 m interval) ・Equipment :GEONICS EM34 ・Analysis :Horizontal Electric Conductivity Profiling ② Resistivity Survey ・Method :Schlumberger method ・Survey depth:a=100m ・Equipment :ABEM SAS300B ・Analysis :1dimention inversion 2. Result of survey 2-1 Potential of Ground Water Basement of survey area is composed with crystal formation (Granite, Gneiss) in Precambrian Period. Upper stratum is weathered. According to the situation of weathered zone, crack and fault in crystal rock (Granite, Gneiss), the formation of aquifer is not constant due to thickness of weathered zone and scale of crack etc. Formation of aquifer are as follow: ・ It is difficult to find aquifer in fissure zone ・ Main aquifer from the test boreholes are located in the boundary between weathered zone and basement. ・ The thickness of weathered zone needs to be more than 20m for high potential of water development ・ Based on the electric conductivity and existing data, the resistivity of weathered zone needs to be less than 130 ohm-m. -

Question Number: ID
Attitudes to Democracy and Markets In Nigeria, November-December, 1999 Data Codebook From data gathered by: Research and Marketing Services (RMS) survey teams Prepared by: Cheryl Coslow Michigan State University October 2002 The Institute for Democracy in South Africa (IDASA) Ghana Centre for Democratic Development (CDD-Ghana) Michigan State University (MSU) 6 Spin Street, Church Square 14 West Airport Residential Area Department of Political Science Cape Town 8001, South Africa P.O. Box 404, Legon-Accra, Ghana East Lansing, Michigan 48824 27 21 461 2559•fax: 27 21 461 2589 233 21 776 142•fax: 233 21 763 028 517 353 3377•fax: 517 432 1091 Mattes ([email protected]) Gyimah-Boadi ([email protected]) Bratton ([email protected]) Copyright Afrobarometer 1 Michigan State University Attitudes to Democracy and Markets Data Codebook Prepared by: Cheryl Coslow From data gathered by: Research and Marketing Services (RMS) survey teams Copyright Afrobarometer 2 Question Number: -- Question: Respondent number. Variable Label: respno Values: 1-1329, 1340-3613 Value Labels: Source: Notes: Assigned by survey managers. Question Number: -- Question: Primary sampling unit. Variable Label: PSU Values: 1-60 Value Labels: 1=Lagos, 2=Ikorodu, 3=Ibadan, 4=Ikire, 5=Egbeda, 6=Abeokuta, 7=Igbo-Ora, 8=Idere, 9=Ondo, 10=Owena, 11=Idanre, 12=Aba, 13=Ikot-Ekpene, 14=Onicha Ngwa, 15=Enugu, 16=Aguobu-owa, 17=Eke, 18=Nsukka, 19=Ibagwa, 20=Obukpa, 21=Benin, 22=Sapele, 23=Ologbo, 24=Port Harcourt, 25=Rumuodamaya, 26=Rukpokwu, 27=Warri, 28=Ughelli, 29=Agbara, 30=Yenagoa, 31=Ilorin, -

Gamma Radioactivity Levels and Their Corresponding External Exposure of Soil Samples from Tantalite Mining Areas in Oke-Ogun, South-Western Nigeria
Radioprotection 2012 DOI: 10.1051/radiopro/2012003 Vol. 47, n° 2, pages 243 à 252 Article Gamma radioactivity levels and their corresponding external exposure of soil samples from tantalite mining areas in Oke-Ogun, South-Western Nigeria A.K. ADEMOLA1, R.I. OBED2 (Manuscript received 9 September 2011, accepted 16 January 2012) Abstract The radioactivity concentrations of 226Ra, 232Th and 40K were measured using gamma-ray spectroscopy with NaI (Tl) detectors in four tantalite mining sites in the Oke-Ogun area, South-Western Nigeria. The measured values of the activities of 40K, 226Ra and 232Th in the soil samples were found to lie in the ranges 123.7 ± 3.8 – 1372.3 ± 8.6, 16.8 ± 1.6 – 71.1 ± 2.53 and 3.0 ± 0.7 – 31.9 ± 1.0 Bq kg–1, respectively. These samples were also found to have radium equivalent activity in the range 74.2–121.0 Bq kg-1. Values of 0.2–0.3 for the external and 0.3–0.4 for the internal hazard indices were estimated for the samples and the annual effective dose varied from 70.3 ± 13.5 to 100.8 ± 42.8 µSv with a mean of 87.5 ± 18.6 µSv y–1. The annual effective dose is higher than the world average. Keywords: Oke-Ogun / radionuclide / tantalite / natural radioactivity / effective dose 1. Introduction Human beings are exposed to background radiation that stems from both natural and man-made sources. Natural background radiation, which is equivalent to 2.4 mSv per person, makes up approximately 80% of the total radiation to which a person is exposed during one year (IAEA, 1996). -

Schedule 2 Local Government Igr Sources in Oyo State
SCHEDULE 2 LOCAL GOVERNMENT IGR SOURCES IN OYO STATE S/N REVENUE NAMES NAME OF LOCAL GOVERNMENT RATE # REMARKS 1 MARRIAGE CERTIFICATE AFIJIO 8,000.00 PER ANNUM 2 BAKE HOUSE LICENSE AFIJIO 10,000.00 PER ANNUM 3 CART TRUCK LICENSE AFIJIO 3,000.00 PER ANNUM 4 HAWKERS/SQUARTORS PERMIT AFIJIO 100.00 WEEKLY 5 ABBATOIR/SLAUGHTER LICENSE AFIJIO 500.00 PER CATTLE 6 HUNTING PERMIT AFIJIO 2,500.00 PER ANNUM 7 CINEMATOGRAPH LICENSE AFIJIO 5,000.00 PER ANNUM 8 TRADE PERMIT(ARTISANS) AFIJIO 4,000.00 PER ANNUM 9 FOREST TIMBER LICENSE AFIJIO 25,000.00 PER ANNUM 10 TRADE UNION FEES AFIJIO 10,000.00 PER ANNUM MINIMUM DEPENDS ON TYPE OF 11 CONTRACTOR REGISTRATION AFIJIO 20,000.00 CONTRACT 12 ASSOCIATION FEES AFIJIO 10,000.00 PER ANNUM MINIMUM DEPENDS ON NATURE 13 TENDERS FEES AFIJIO 30,000.00 OF CONTRACT 14 DEATH REGISTRATION CERTIFICATE AFIJIO 2,500.00 PER CHILD 15 DEVELOPMENT LEVIES AFIJIO 200.00 PER ANNUM 16 PARKING FEES AFIJIO 200.00 DAILY 17 LOCAL GOVERNMENT IDENTIFICATION AFIJIO 2,500.00 18 PROCEED FROM SALES OF GOODS/FARM PRODUCES AFIJIO VARIES 19 SALES OF SCRAPS AFIJIO VARIES 20 EARNING FROM COMMERCIAL ACTIVITIES AFIJIO VARIES 21 EARNING FROM PARK AND GARDEN AFIJIO 500.00 PER PERSON 22 EARNING FROM GUEST HOUSE AFIJIO 10,000.00 PER ANNUM 23 POLLS TAX AFIJIO 1,000.00 PER ANNUM MINIMUN. DEPENDS ON 24 LIVESTOCK AFIJIO 1,000.00 PRODUCT 25 TENAMENT RATES AFIJIO 2,300.00 MINIMUN. DEPEND ONSIZE 26 BULL PERMIT AFIJIO 5,000.00 PER ANNUM 27 WHEEL BARROW FEES AFIJIO 50.00 DAILY 28 SHOP AND KIOSK FEES AFIJIO 200.00 PER MONTH 29 MARKET SQUATER AFIJIO 50.00 PER -

Effects of Wood Harvesting on the Livelihood of Forest Fringe Communities in Southwest Nigeria
51 Agro-Science Journal of Tropical Agriculture, Food, Environment and Extension Volume 19 Number 4 (October 2020) pp. 51 - 55 ISSN 1119-7455 EFFECTS OF WOOD HARVESTING ON THE LIVELIHOOD OF FOREST FRINGE COMMUNITIES IN SOUTHWEST NIGERIA *Awe F., Olarewaju T.O., Orumwense L.A. and Olatunji B.T. Forest Economics & Extension Department, Forestry Research Institute of Nigeria, P.M.B. 5054, Jericho Hills, Ibadan, Oyo State, Nigeria *Corresponding author’s email: [email protected] ABSTRACT This study was carried out to assess effects of wood harvesting on the livelihood of forest communities in Ibarapa region, southwest, Nigeria. The study was conducted to identify the various livelihood activities engaged in by forest communities in the region; to assess how wood harvesting in the forests has affected the livelihood of the people in the region as well as to determine the factors influencing wood harvesting in the region. Three hundred copies of structured questionnaire were used to elicit information from the respondents. Focused Group Discussion and Key Informant Interview were also used. Data were analyzed using descriptive statistics and logistic regression. Results show that various livelihood activities were engaged in by the respondents, prominent among which were food crop production, cash crop production, charcoal production, among others. Among the factors that were responsible for wood harvesting in the region, only age, occupation, household size and the distance of respondent’s house to the forest were significant at 5%. It was observed that excessive wood harvesting has negatively affected the forests in the study area as most of the forests have been greatly degraded. -

Farmers Perception on Effects of Climate Change on Cocoa Production in Ibarapa/Ibadan Agricultural Zone of Oyo State, Nigeria
International Journal of Innovative Agriculture & Biology Research 7(3):18-25, July-Sept., 2019 © SEAHI PUBLICATIONS, 2019 www.seahipaj.org ISSN: 2354- 2934 Farmers Perception On Effects Of Climate Change On Cocoa Production In Ibarapa/Ibadan Agricultural Zone Of Oyo State, Nigeria 1Ilori, A.R, Fadipe M. O., & Onasanya A. S. Department of Agricultural Extension and Rural Sociology Faculty of Agricultural Management and Rural Development College of Agricultural Sciences, Olabisi Onabanjo University Yewa Campus, Ayetoro, Ogun State, Nigeria [email protected] Tel: 08059371025 ABSTRACT Climate change poses serious threat to agricultural development in many developing countries like Nigeria. This study focused on farmer's perception on effects of climate change on cocoa production in Ibarapa/Ibadan agricultural zone of Oyo State. Multistage random technique was adopted in obtaining the sample size of 126 respondents. Structured interview schedule was used to collect data from the respondents on personal characteristics, constraints facing farmers, source of information on climate change by farmers and perception of cocoa farmers on climate change. The data were subjected to both descriptive and inferential statistics. The results reveal that 67.5% of the respondents were male, 96.8% were married, 39.7% of respondents falls between 41-50Years. It was also revealed that significant relationship exist between age (x=68.239,p<0.05), sex (x=40.245,p<0.05), marital status (x=35.909,p<0.05) and their perception on effects of climate change on cocoa production. The major constraints revealed were capital (x=37.360,p<0.05), labour (x=54.087,p<0.05). -

Effect of Ebola Virus Disease Outbreak on Bush Meat Consumption in Ibarapa Region of Oyo State, Nigeria
International Journal of Agriculture and Earth Science Vol. 2 No.2 ISSN 2489-0081 2016 www.iiardpub.org EFFECT OF EBOLA VIRUS DISEASE OUTBREAK ON BUSH MEAT CONSUMPTION IN IBARAPA REGION OF OYO STATE, NIGERIA Olaniyan, S. T., Adeosun, A. O., and Owoade O. A. Department of Agricultural Education, School of Vocational and Technical Education, Emmanuel Alayande College of Education Oyo, Lanlate Campus Nigeria [email protected] Abstract Bush meat is a special delicacy of the Ibarapas, hence, a survey of the effects of Ebola Virus disease outbreak on consumption of bush meat in Ibarapa region of Oyo state was conducted. Questionnaires were randomly administered on 630 respondents in the three local governments in the region. Data were analyzed using descriptive statistics and likert rating scale. Findings revealed that outbreak of Ebola virus disease has implication on consumption of bush meat in the study area and has affected the livelihood of the marketer. Bush meats consumed in the area were also found to include squirrel, rodents, antelope, snake, alligator, bush fowl etc. Investigation revealed that consumption of animals such as bats and big rats were forbidden in some places in the studied area. Also, choices of bush meat consumed were found to depend on availability, delicacy, price, nutrition and custom. Respondents agreed that bush meat if not properly cooked can transmit not only EBOV but other diseases. Respondent agreed that not all wild animals can transmit EBOV. The study therefore concluded that there should be adequate education on mode of transmission and prevention of EBOV by stakeholders, such as Health officer and extension workers.