Communications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Food Dignity® COVID-19 Era: Challenge the Stigma, Change The
Food Dignity® COVID-19 Era: Challenge the Stigma, Change the Culture May 3, 2021 Bringing to life the dairy community’s shared vision of a healthy, happy, sustainable world, with science as our foundation environmental stewardship goals for air, land The New York Times Magazine September 6, 2020. Photos: Brenda Ann Kenneally Today’s Speakers Clancy Harrison, MS, RDN, FAND Theresa McCormick Lisa McCann, RDN Founder Director of Programs & Healthcare Wellness Manager Food Dignity Project Partnerships Midwest Dairy [email protected] Second Harvest Heartland [email protected] @ClancyCHarrison [email protected] @LisaMcCannRD @Schneitr The Dairy Community’s Commitment to Fighting Hunger Addressing food and nutrition security with dynamic partnerships Local Efforts with Food Banks & Schools Across the United States COVID-19 has impacted every facet of the food system Closure of schools across the Restaurant service was Loss of jobs has challenged U.S. reduced channel that ~30 limited, so Americans are millions of additional Americans million food-insecure children eating a lot more at home with food insecurity – putting rely on for nutritious meals pressure on food banks to serve every day many more clients/families Work with Minnesota Food Banks to Nourish Communities $500,000 Food Bank donation across Midwest Dairy • 5 Minnesota food banks • 777,433 pounds of dairy products to food banks in MN Undeniably Dairy Funding • 27 Refrigeration coolers to MN Food Pantries • Reach of 56,000 People 10 Emergency Relief for Minnesota -

Larsenauction Brouillette 11-3-18.Pmd
AUCTION In order to help settle this Estate, we will offer the following Antiques & Collectibles for sale at public auction to be held in the Cordova Community Building in Cordova, NE on: Saturday, November 3, 2018 Starting at 10:00 a.m. - Lunch stand on grounds Antiques & Collectibles (4) Dump Rakes Steel Implement Wheels (all sizes) Sickle Mowers Rocking Chair Wooden Spinning Wheel Dresser’s Wooden Chairs Shelves Wooden Magazine Rack Wooden Desk 1950’s Formica Table Several Framed Mirrors Metal Lunchboxes & Thermoses Old Saddle (military?) Harness Rosettes Hames Badge Collection Pocket Knives Bottle Opener Collection; Belt Buckles; Many Adv. Pens & Pencils; Adv. Yardsticks; Adv. Calendars; Vacuum Bottle Stopper Display; (3) Guitars (Gene Autry & Others); Toy Guns; Some Old Dolls(Crissy, Porcelain, Soft Body & Handmade); Many Unopened Fast Food Toys; Other Misc. Toys; Letter Opener Display; Adv. Matchbooks; Cigar Boxes; 6’ Long Timex Display; Milk Bottles; Many Old Bottles (all kinds); Steel Beer Cans; Set of Wildlife Beer Steins; Set of 4 Avon Steins (conquest of space, Columbus new world, racing world, postal world); Decanters; Quilts; Pillowcases; Other Doilies & Fancywork; Boxes of Cookbooks; Many Books (new & old); Several Vehicle Repair Manuals; Old Alden & Mont. Wards Catalogs; Magazines in binders; Records; Record Players; Old Radios; Pictures & Prints; Hunting Pictures; Some Decoys; Kerosene Lamps; Aladdin Lamp Base; Old Irons; Food Grinders; Stove Handles; Wood Handled Kitchen Utensils; Shoe Lasts; Cast Horses; Miniature Ducks; Bookends; Meat Shop Scale; Adv Wood Canes; Misc. Tins; Old Curling Irons; Bed Pans; Wire Milk Crate; Metal & Plastic Cookie Cutters; Cookie Jars; Canning Jars; Salt & Peppers; Wall Pockets; Telephone Insulators; Pepsi Bottles w/ carrier; Husker Pop Bottles; Collection of Hens on Nest; Fenton Hobnail Glassware; Cartoon Character Glasses; Pyrex Dishes; Other Baking Dishes; Decorative Glassware; Other Misc. -

Crate Farming 101
CRATE FARMING 101 Before you start growing your own food in milk crates, set yourself up for success with SUN, SOIL and WATER, and the knowledge needed to get the most out of your available space. (1) Minimum 4 hours of sunlight, ideally 6+ hours. (2) Clean tested soil. (3) A crop plan taking into consideration available light, the season, quick/slow crops, available growing space. (4) A water source and irrigation on a timer, OR the availability to water manually e/o day. (5) Knowledge about maintaining the soil (fertilizing/amending), maintaining the garden (thinning, weeding, trellising, pollinating), and pest and disease management. (6) Season extension. (7) How to use your harvest (preparing, cooking, canning, pickling). SITE SELCTION—FINDING LIGHT Light is perhaps the most important element when selecting a garden site. 4- 6 hours of unfiltered sun will support low-light crops, 6 or more hours are required to successfully grow full sun crops (like tomatoes). Using a solar tracker is the most accurate way to measure sunlight hours. Take into account the height of trees when they're leafed out. More sunlight = more growth potential. Green City Growers | 617.776.1400 | [email protected] | 600 Windsor Place, Somerville, MA 02143 | www.greencitygrowers.com WHAT YOU NEED TO GROW SHOPPING LIST Milk crate (1’x1’) Landscaping fabric (3’x3’) Scissors Staple gun Organic soil Seeds/Starts Learn more about how to PLANT SPACING: 1’X1’ grow fresh vegetables anywhere the sun shines with our comprehensive urban farming guide book The Urban Bounty: How to Grow Fresh Food Anywhere. -
One Milk Crate of Debris at a Time
September 2, 2013 Volume 17 Number 17 One milk crate of debris at a timepg. 20 inside Hindsight foresight insight 4 Healing the Mennonite class divide 14 PM40063104 R09613 What is the ‘settler problem’? 23 2 Canadian Mennonite September 2, 2013 Editorial champions “justice” as one of its core beliefs. Can we, with God’s help, bring some kind of redemption to this shadowy Healing sexual abuse narrative? In both cases, we in the larger com- Dick Benner munity can feel rather helpless. In the Editor/Publisher Yoder case, it is a distant event, happen- ing in an era when, in a more patriarchal wo stories on sexual abuse have the experience, what could go better in religious system, men took liberties that re-emerged recently on the restoration of victims and perpetrators today are not tolerated. In the Bolivia TMennonite scene that call for so- in cases of sexual harassment and abuse? Old Colony story, these are far-distant ber reflection and some self-examination, Where can growth continue?” she asks. cousins, both in faith and practice, and but not self-obsession. They should be The safety of women in another in geography. We are shamed and sad- seen, in the present, as “teachable mo- setting—the Manitoba Old Colony of dened, but barely capable of reaching into ments” and occasions for healing, Bolivia—has also hit the inter- such an insular communal group that rather than harsh judgments on national media in a recent first and foremost resents and resists any the sins of our fathers. in-depth story by Time reporter outside counsel or help. -
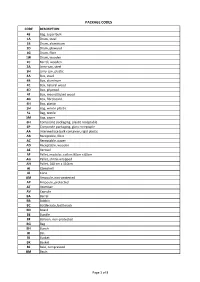
Package Codes
PACKAGE CODES CODE DESCRIPTION 43 Bag, super bulk 1A Drum, steel 1B Drum, aluminium 1D Drum, plywood 1G Drum, fibre 1W Drum, wooden 2C Barrel, wooden 3A Jerry-can, steel 3H Jerry-can, plastic 4A Box, steel 4B Box, aluminum 4C Box, natural wood 4D Box, plywood 4F Box, reconstituted wood 4G Box, fibreboard 4H Box, plastic 5H Bag, woven plastic 5L Bag, textile 5M Bag, paper 6H ComposIte packaging, plastic receptable 6P Composite packaging, glass receptaple AA Intermediate bulk container, rigid plastic AB Receptable, fibre AC Receptable, paper AD Receptable, wooden AE Aerosol AF Pallet, modular, collars 80cm x 60cm AG Pallet, shrink-wrapped AH Pallet, 100 cm x 110cm AI Clamshell AJ Cone AM Ampoule, non-protected AP Ampoule, protected AT Atomiser AV Capsule BA Barrel BB Bobbin BC Bottlecrate, bottlerack BD Board BE Bundle BF Balloon, non-protected BG Bag BH Bunch BI Bin BJ Bucket BK Basket BL Bale, compressed BM Basin Page 1 of 8 PACKAGE CODES CODE DESCRIPTION BN Bale, non-compressed BO Bottle, non-protected, cylindrical BP Balloon, protected BQ Bottle, protected cylindrical BR Bar BS Bottle, non-protected, bulbous BT Bolt BU Butt BV Bottle, protected bulbous BW Box, for liquids BX Box BY Board, in bundle/bunch/truss, BZ Bars, in bundle/bunch/truss CA Can, rectangular CB Beer crate CC Churn CD Can, with handle and spout CE Creel CF Coffer CG Cage CH Chest CI Canister CJ Coffin CK Cask CL Coil CM Collis CN Container not otherwise specified as transport equipment CO Carboy, non-protected CP Carboy, protected CQ Cartdidge CR Crate CS Case CT -

Tender Document for Supply of Milk Plastic Hdpe Crates (12 Ltr Square Types)
JHARKHAND STATE COOPERATIVE MILK PRODUCERS’ FEDERATION LIMITED REQUEST FOR QUOTATION JHARKHAND STATE COOPERATIVE MILK PRODUCERS’ FEDERATION LTD Near Farmers Training Centre Campus, Sec-II, H.E.C., Dhurwa, Ranchi – 834004, Jharkhand Phone no: 7544003404/7360035219/0651-2443055/62 Email: [email protected] Website: www.jmf.coop TENDER DOCUMENT FOR SUPPLY OF MILK PLASTIC HDPE CRATES (12 LTR SQUARE TYPES) Tender No.: JMF-PP-Milk Crate-Square /2020-21/003 Tender Release date: 25.02.2020 Last Date for submission of Tender: On or before: 20 Mar 2020 by 05.30 P.M. Opening of Technical Tender: Opening of Financial Tender: Date: 21 Mar 2020 At 16.00 P.M. Shall be notified Later after opening of At Medha Dairy Plant. Technical Bid. Hotwar, (Khelgaon), Ranchi, Jharkhand – 835217 Name of Bidder: ______________________________________ Address: ________________________________________________ ________________________________________________________ ________________________________________________________ Telephone no: __________________________________________ Email Id________________________________________________ All rights reserved. This material is confidential and proprietary of The Jharkhand State Co-operative Milk Producers’ Federation Ltd(JMF) and no part of this material should be reproduced, published in any form by any means, electronic or mechanical including photocopy or any information storage or retrieval system nor should the material be disclosed to third parties without the written authorization of JMF Page 1 / 10 TENDER INVITATION Invitation for Tender/ Quotation for Supply of: MILK PLASTIC HDPE CRATES (12 Ltr Square Type) with Branding The Jharkhand State Cooperative Milk Producers’ Federation Ltd. (JSCMPFL), registered under Jharkhand Co-operative Societies Act, 1935 is engaged in milk procurement, processing and marketing activities of item milk and milk products in the state of Jharkhand and is popularly known for its brand ‘Medha’. -

Chapter 2B Dating Milk Bottles, Part II © Bill Lockhart 2011 Paper Milk Cartons on Several Occasions, Paper Cartons Challenged
Chapter 2b Dating Milk Bottles, Part II © Bill Lockhart 2011 Paper Milk Cartons On several occasions, paper cartons challenged the supremacy of glass as containers for milk. Only the last was really successful. For a thorough discussion of the issues surrounding paper containers and a more complete list of patents, see the Dairy Antique Site (2011). Early Paper Cartons – 1896-1915 Hervey D. Thatcher, noted for some of the earliest glass milk bottles, also applied for a patent for a waxed paper milk pail on June 24, 1895, and received Patent No. 553,794 on January 28, 1896 (Figure 2-39). Thatcher discussed many of the issues connected with glass milk bottles (including breakage as well as problems with sanitation and washing). He claimed that his “Parafinned Pail” would solve the problems with glass. Thatcher followed up with two other patents for refinements, Patent No. 619,019 for a “Paper Pail” on February 7, 1899, and Patent No. 688,365 for another “Paper Pail” on December 10, 1901. He never advanced beyond the “pail” design. Figure 2-39 – Thatcher “Parafinned Pail” Winslow (1907:140) noted that “the latest departure in the way of a milk bottle is the single service milk container of wood-paper made and invented by G.W. Maxwell of 2101 Folsom St., San Francisco. now in actual use by dairymen in Los Angeles.” The “bottles” were shaped like “an ordinary drinking glass” and came in quart, pint, half-pint, and quarter-pint sizes. The paper cover was wedged into place and held by four tabs. Although Winslow gave Maxwell full credit for the invention, the actual patent document named George W. -

Sliding Top Milk Case Dispenser Laminate Panel (L) Or Stainless Steel (S)
Sliding Top Milk Case Dispenser Laminate Panel (L) or Stainless Steel (S) Project: Item: Quantity: Date: Sliding Top Milk Case Dispenser Top Sliding Laminate Panel (L) or Stainless Steel (S) Laminate Panel Models Length CPM 1306-L/S 39 3/4” CPM 1310-L/S 57” CPM 1314-L/S 75 3/4” Standard Features 14 gauge stainless steel tops Insulated stainless steel sliding doors Self-leveling crate dispensers Dispensers adjustable without tools Welded stainless steel interior 5” swivel casters Cam Operated Line-up Locks CPM-1310-L shown with option: (GG) lid locks. Holds crates, no re-loading necessary Easy mobility Durable and easy to clean Crates maintained at easy-to-reach height ANSI/NSF7 U.L. Sanitation Classifi ed to NSF Standards Specifi cations Self-leveling System - Each milk crate to be held Body (S) - Uni-body structure, fabricated from Top and Lids - Top to be 14 ga. stainless steel at proper height by two stainless steel self- 18 gauge stainless steel, welded ground and A.I.A. File No. 00-0-00 SIS No. 00-0-00 with square turndown on all sides and corners leveling mechanisms, fi eld adjustable without polished. Interior reinforced with 12 gauge fully welded, ground and polished. To have tools, and a removable stainless steel carrier. galvanized uprights to support shelving and a 20 #4 satin fi nish and all edges to have #7 hi-lite (Area above compressor will not be self-leveling.) gauge steel bottom. fi nish. Interior top to turn down into opening and Refrigeration System - A temperature of 38 Body (L) - Standard grade laminate to cover all complete with integral ledges to support sliding degrees F shall be maintained by a cold wall sides of an 18 gauge steel uni-body structure. -

Microbiological Sampling
Microbiological Sampling A webinar presented by: Dr Andy Bowles Attendee Notes 10/10/2018 Microbiological sampling Dr Andy Bowles This webinar will consider Why sample foods? Legal framework Approach to sampling Sampling technique Microbiological sampling Why sample foods? Legal framework Approach to sampling Sampling technique 1 10/10/2018 Purpose of Sampling Surveillance FSA survey Regional sampling Verification As part of routine inspection/audit Compliance Regulation 853/2004 Investigative Complaint Outbreak Microbiological sampling Why sample foods? Legal framework Approach to sampling Sampling technique Legal Framework Regulation (EC) 882/2004 “Official control” Regulation (EC) 178/2002 Regulation (EC) 2073/2005 Food Safety and Hygiene (England) Regs 2013 Food Safety (Sampling and Qualifications) (England) Regulations 2013 Food Law Code of Practice Food Law Practice Guidance 2 10/10/2018 Interventions Official Controls Other interventions inspections education audits advice sampling visits coaching monitoring visits information and intelligence gathering surveillance visits verification visits What is a sample? Sample : “Portion of an item which may or may not be representative of the whole item” Representative sample “A portion of an item that has been taken in such a manner that inferences may be made regarding the microbiological flora or chemical composition of the whole item” 3 10/10/2018 Formal v Informal Samples What is a “Formal” sample? 10 Microbiological sampling Why sample foods? Legal framework Approach to sampling Sampling technique Sampling Pitfalls Three main issues to consider to avoid problems: Planning Sampling technique Continuity of evidence 4 10/10/2018 Planning Consider: Targeting What food is to be sampled Quantity of sample required Nature of target organism Purpose of sampling Follow up action Targeting Consider targeting premises/importers: where concerns have been raised about the ability of management to consistently produce safe food. -

Utah's Hogle Zoo Orangutan Enrichment Catalog MANIPULATIVE
Utah’s Hogle Zoo Orangutan Enrichment Catalog MANIPULATIVE ITEMS/TOYS Crates tied with firehose Description: Animal can manipulate the device or find food items placed in/under crates. Supplies: o Plastic milk crates o Hose or strips of bed sheets to tie crates together PVC “Tinker Toys” Description: Various sizes/shapes of PVC pieces (pipes, T’s, elbows, etc.). Animals can assemble or disassemble into various shapes, use as tools, water toys, etc. Supplies: o PVC pipes o PVC corner pieces Paper Maché Devices Description: Paper maché various plastic devices- boomers, etc. Can hide small food items within the layers of maché, scent/flavor/spice paste mix or just provide plain. Task oriented, destructible enrichment. Supplies: o Newspaper strips o Water o Flour o Treats (small seeds, raisins, peanuts, etc.) o Scents, flavors, spices as needed FOODS/FEEDING Browse Hanger Description: Tightly woven firehose hanger for browse. Weave browse ends into spaces in fire hose, providing for a novel, task oriented browse provision. Supplies: o 2-3 strips of fire hose Kracor Keg in Crate Description: Fill keg with treats and place keg inside a milk crate. Attach milk crate to cage so that all sides are enclosed. The enrichment item provides two barriers and increased challenge to stimulate the animal, encourage foraging techniques and extend feeding times. Supplies: o Plastic milk crate o Keg (Kracor) or make your own . Closed cylindrical container with holes o Chains to attach crate Greens Feeder Description: 2 steel grill grates clipped together with greens inside. The device should be very tightly packed so the animals really have to work to acquire food. -

Reassessing Waste Value for a Sustainable Future
Rochester Institute of Technology RIT Scholar Works Theses 5-10-2015 Waste as Parts: Reassessing waste value for a sustainable future Patricio Corvalan Follow this and additional works at: https://scholarworks.rit.edu/theses Recommended Citation Corvalan, Patricio, "Waste as Parts: Reassessing waste value for a sustainable future" (2015). Thesis. Rochester Institute of Technology. Accessed from This Thesis is brought to you for free and open access by RIT Scholar Works. It has been accepted for inclusion in Theses by an authorized administrator of RIT Scholar Works. For more information, please contact [email protected]. RIT Waste as Parts Reassessing waste value for a sustainable future by Patricio Corvalan A Thesis in Partial Fulfillment of the requirements for the Degree of Master of Fine Arts in Industrial Design School of Design College of Imaging Arts and Science Rochester Institute of Technology Rochester, NY May 10, 2015 1 Chief advisor Stan Rickel, Graduate Coordinator and Associate Professor School of Design, Industrial Design [email protected] Signature of Chief advisor Date Associate Advisor Dan Harel, Project Advisor, Adjunct Professor of Design School of Design, Industrial Design [email protected] Signature of Project Advisor Date Associate Advisor Dana W0lcott, Lead Innovation Coach Simone Center for Innovation and Entrepreneurship [email protected] Signature of Project Advisor Date 2 In a context in which solid waste is a major issue within current society problems, “Adopt a Product” is a line of home objects that uses the structural qualities of disposed plastic containers in their design. Exploring an underestimated material resource brought the idea of using overly reinforced food packaging to make affordable products. -

EPP280 with Web Strap Half-Size Camwarmer Milk Crate Box
EPP280 with Web Strap Milk Crate Box • Features a convenient, • Holds a 13" x 13" milk crate adjustable web carrying strap with 70 half pint milk cartons. and molded in handles. • Features an adjustable web strap and molded in handles. CODE EPP280WSTSW CAPACITY 1 each GN 1/2 8" deep food pan* CODE EPPMBWSTSW VOLUME 23.6 qt. (22,3 L) CAPACITY Holds 1 each 13" x 13" x 11" EXTERIOR DIM. L 15.4" x W 13" x H 12.4" (33 x 33 x 28 cm) milk crate (39,1 x 33 x 31,4 cm) VOLUME 10.7 gal. (40,5 L) INTERIOR DIM. L 13" x W 10.6" x H 10" (33 x 27 x 25,4 cm) EXTERIOR DIM. L 16.1" x W 16.1" x H 15.9" (41 x 41 x 40,4 cm) UNIT WEIGHT 1.8 lbs. (0,8 kg) INTERIOR DIM. L 13.8" x W 13.8" x H 13.5" (35 x 35 x 34,3 cm) Color: Black (110). *Or equivalent. UNIT WEIGHT 2.65 lbs. (1,2 kg) Color: Black (110). EPP180 XLT • The EPP180 with extra Half-Size Camwarmer width, length and height for • Designed to extend food’s easier access when loading hot holding time. and unloading pans. • Submerge in hot water for 35 minutes then add to CODE EPP180XLTSW bottom of carrier. VOLUME 68.2 qt. (64,5 L) EXTERIOR DIM. L 24" x W 17" x H 15.4" (61 x 43,1 x 39,1 cm) CODE HP2632 FITS EPP260SW, EPP280SW, INTERIOR DIM.