The Impact of Osteopathic Treatment on Increased Intraocular Pressure in Primary Chronic Open-Angle Glaucoma
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Special Sense
Anatomy Models Special Sense Foramina & Fissures of the Orbit Foramen Structures Passing 1- Optic nerve ( surrounded by its meninges ) Optic Foramen 2- Opthalmic artery 1- Occulomotor n. 2- Trochlear n. Sup. Orbital Fissure 3- Abducent n. 4- Ophthalmic Veins. 1- Infra Orbital nerve Inf. Orbital Fissure 2- Infra Orbital artery 3- Orbital branch of sphenopalatine ganglion. 4- Emissary vein , between inf. orbital V. & pterygoid plexus. Frontal air sinus Ethmoid air sinus Branches of Olfactory Nerve Sphenoid air sinus (Inside body of sphenoid) Perpendicular plate of ethmoid Vomer Superior Oblique Muscle From the post. part of the roof of The lat. Aspect of the eye ball between orbit antromedial to the optic sup. Rectus & lat. rectus foramen. Trochlear n. ( 4 ) S.O.4 Inf. division Medial Rectus Sup. division Superior Rectus Inf . division Inferior Rectus Abducent ( 6) LR 6 Lateral Rectus - The 4 recti muscle arise from tendinous ring at the apex of the o rbit surrounding the optic formen & the med. ends of the sup. & inf. orbital fissure - Origin of each one depends on the name.(e.g. Sup. Rectus from the sup. Part of the ring ) Insertion into the sup. , inf. , med. & lat. Surfaces of the sclera, short dista nce behind the corneo-scleral junction. All extraoccular muscles are supplied by occulomotor nerve(3) except: 1- Lat. Rectus supplied by abducent (6) Optic Nerve 2- Sup. Oblique supplied by trochlear (4) Sup . Lacrimal gland Its Position is upper-lateral Lat . Med . Right Eye Inf . Sup. Oblique m. Optic Nerve Inf. Oblique Oval Round Ear Drum Promantry window window Mastoid air cells Mastoid Antrum Aditus I.C.R Tensor Tympani muscle Eustachian tube Tensor Palati muscle External auditory meatus The medial wall ( nasal septum ) is formed by: 1- Septal cartilage ……………….… Anteriorly 2- Perpendicular plate of ethmoid . -

The Development of Mammalian Dural Venous Sinuses with Especial Reference to the Post-Glenoid Vein
J. Anat. (1967), 102, 1, pp. 33-56 33 With 12 figures Printed in Great Britian The development of mammalian dural venous sinuses with especial reference to the post-glenoid vein H. BUTLER Department ofAnatomy, University of Saskatchewan, Saskatoon, Canada The intracranial venous outflow of mammals drains into both the internal and external jugular veins and the relative role of these two veins varies between different adult mammals as well as at different phases of embryonic and foetal life. In general, the primary head vein (consisting of venae capitis medialis and lateralis and their tributaries) gives rise to the dural venous sinuses which drain into the anterior cardinal vein (the future internal jugular vein). The external jugular veins appear as the face and jaws develop but, at all times, the two venous systems freely com- municate with each other. Morphologically, as shown by Sutton (1888), both the dural venous sinuses and the external jugular venous system are extracranial in so far as they are situated outside the dura mater. The chondrocranium and the dermocranium, however, develop in between the dural venous sinuses and the external jugular vein system (Butler, 1957). Thus, in the adult mammal, the bony skull wall separates the two venous systems, and therefore the dural venous sinuses are topographically intracranial whereas the external jugular venous system is extracranial. Furthermore the development of the skull localizes the connexions between the dural venous sinuses and the external jugular venous system to the various fontanelles and neuro-vascular foramina to form the emissary veins. The post-glenoid vein is one of the more important and controversial emissary veins since its presence or absence has been used in attempts to establish mammalian phylogenetic relationships (van Gelderen, 1925; Boyd, 1930). -

Dural Venous Sinuses Dr Nawal AL-Shannan Dural Venous Sinuses ( DVS )
Dural venous sinuses Dr Nawal AL-Shannan Dural venous sinuses ( DVS ) - Spaces between the endosteal and meningeal layers of the dura Features: 1. Lined by endothelium 2. No musculare tissue in the walls of the sinuses 3. Valueless 4.Connected to diploic veins and scalp veins by emmissary veins .Function: receive blood from the brain via cerebral veins and CSF through arachnoid villi Classification: 15 venous sinuses Paried venous sinuses Unpaired venous sinuses ( lateral in position) • * superior sagittal sinus • * cavernous sinuses • * inferior sagittal sinus • * superior petrosal sinuses • * occipital sinus • * inferior petrosal sinuses • * anterior intercavernous • * transverse sinuses • sinus * sigmoid sinuses • * posterior intercavernous • * spheno-parietal sinuses • sinus • * middle meningeal veins • * basilar plexuses of vein SUPERIOR SAGITTAL SINUS • Begins in front at the frontal crest • ends behind at the internal occipital protuberance diliated to form confluence of sinuses and venous lacunae • • The superior sagittal sinus receives the following : • 1- Superior cerebral veins • 2- dipolic veins • 3- Emissary veins • 4- arachnoid granulation • 5- meningeal veins Clinical significance • Infection from scalp, nasal cavity & diploic tissue • septic thrombosis • CSF absorption intra cranial thrombosis (ICT) • Inferior sagittal sinus - small channel occupy • lower free magin of falx cerebri ( post 2/3) - runs backward and • joins great cerebral vein at free margin of tentorium cerebelli to form straight sinus. • - receives cerebral -

An Anatomico-Radiological Study of the Grooves for Occipital Sinus in the Posterior Cranial Fossa
Bratisl Lek Listy 2008; 109 (11) 520524 COMPARATIVE ANATOMY An anatomico-radiological study of the grooves for occipital sinus in the posterior cranial fossa Srijit Das1, Azian Abd Latiff1, Farihah Haji Suhaimi1, Faizah Bt Othman1, Mohd F Yahaya1, Fairus Ahmad1, Hamzaini Abdul Hamid2 Department of Anatomy, Universiti Kebangsaan Malaysia, Jalan Raja Muda Abdul Aziz, Kuala Lumpur, Malaysia. [email protected] Abstract: Background: The occipital sinus (OS) lies in the attached margin of the falx cerebelli in the internal occipital crest of the occipital bone. The OS extends from the foramen magnum to the confluence of sinuses. Standard textbooks and research reports do not describe in detail any variation in the groove for the occipital sinus. Methods: In the present study, we examined a total of 50 human dried skulls for the groove of OS and its possible variations. We also performed an osteological study supplemented with digital X ray and CT scan. Results: Out of 50 skull specimens, a single case with two grooves for OS was observed (2 %). The two grooves for OS traversed as two limbs from the foramen magnum to join the other at the internal occipital protuberance. An accessory faint groove was also found at the lateral aspect of the left limb. Interestingly, in the same specimen, the superior sagittal sinus instead of continuing as right transverse sinus, continued as left transverse sinus. The X ray and CT scan of the anomalous bone specimen were compared to those of the normal bone specimen. Discussion: To the best of our knowledge, this is the first anatomico-radiological study of multiple OS groove with associated anomalies. -

A Study of Unusual Presentations at the Internal Occipital Protuberance
Original Research Article A study of unusual presentations at the internal occipital protuberance Sudeepa Das¹, Gyanraj Singh2, Satya Narayan Shamal3, Bikash Chandra Satapathy4* 1,2Assistant Professor, 3Professor, Department of Anatomy, KIMS, Bhubaneswar, Odisha. 4Assistant Professor, Department of Anatomy, AIIMS Mangalagiri, Andhra Pradesh, INDIA. Email: [email protected] Abstract The dural venous sinuses contains the venous blood originating from most parts of the cranial cavity. In this study forty head and neck specimens with intact dural folds were studied over 3 years period. In 2 cases variation was noted at the internal occipital protuberance during the routine dissection in Anatomy department. After separating the dura mater from the occipital bone, two distinct internal occipital crests were apparent which then diverge near the foramen magnum. We encountered duplicated internal Occipital crest along with duplicated falx cerebelli and occipital sinus. Of both specimens the falces and the distance between them were recorded. Each of the falx cerebelli had an apex and base with a marked occipital venous sinus attached to its border. These sinuses were draining into their respective transverse sinuses. In both the cases there was wide posterior cerebellar notch and foramen of Magendie associated with large cisterna magna. There was neither any marginal sinus detected nor any defect was marked in the vermis. Knowledge of this variation of posterior cranial fossa would be helpful in suboccipital approaches. Key Words: Variation, -

Bilateral Transverse Sinus Hypoplasia: a Rare Case Report
J Exp Clin Neurosci, 2018, 5(1): 1-2 Case Report Bilateral Transverse Sinus Hypoplasia: A Rare Case Report Elyar Sadeghi-Hokmabadia, Masoud Poureisab, Neda Ghaemiana,*, Zahra Parsianc aNeurosciences Research Center, Tabriz University of Medical Science, Tabriz, Iran bDepartment of Radiology, Radiotherapy and Nuclear Medicine, Tabriz University of Medical Sciences, Tabriz, Iran cDepartment of Emergency Medicine, Tabriz University of Medical Sciences, Tabriz, Iran Abstract The dural sinuses are pathways for drainage of blood from brain to the internal jugular veins. Occipital sinus is a rare normal anatomical variation of dural sinuses which acts as an alternative drainage pathway Correspondence when the transverse sinuses are hypoplastic. It drains blood from skull and brain to the internal jugular Neda Ghaemian, vein. The variations can culminate in wrong diagnosis and imaging interpretation. We reported a Neurosciences Research Center, Tabriz 33 years old pregnant woman presented with headache and normal neurological examination. Magnetic University of Medical Science, Tabriz, Iran. resonance imaging and magnetic resonance venography studies revealed occipital sinus as the main Tel/Fax: +98-41-333340730 drainage pathway of the brain. Both the transverse sinuses were hypoplastic. Without considering this Email: [email protected] rare variation such conditions can culminate in wrong diagnosis, which can be prevented by reporting such rare conditions. Received: 2017-06-10 Accepted: 2017-12-12 Keywords: Transverse sinus, Hypoplasia, Headache DOI:10.13183/jecns.v%vi%i.75 ©2018 Swedish Science Pioneers, All rights reserved. Introduction symptoms. Pain did not respond to oral analgesics. She had The dural sinuses are pathways for drainage of blood from brain a history of chronic generalized deep seated and throbbing to the internal jugular veins [1]. -

The Suboccipital Cavernous Sinus
The suboccipital cavernous sinus Kenan I. Arnautovic, M.D., Ossama Al-Mefty, M.D., T. Glenn Pait, M.D., Ali F. Krisht, M.D., and Muhammad M. Husain, M.D. Departments of Neurosurgery and Pathology, University of Arkansas for Medical Sciences, and Laboratory Service, Veterans Administration Medical Center, Little Rock, Arkansas The authors studied the microsurgical anatomy of the suboccipital region, concentrating on the third segment (V3) of the vertebral artery (VA), which extends from the transverse foramen of the axis to the dural penetration of the VA, paying particular attention to its loops, branches, supporting fibrous rings, adjacent nerves, and surrounding venous structures. Ten cadaver heads (20 sides) were fixed in formalin, their blood vessels were perfused with colored silicone rubber, and they were dissected under magnification. The authors subdivided the V3 into two parts, the horizontal (V3h) and the vertical (V3v), and studied the anatomical structures topographically, from the superficial to the deep tissues. In two additional specimens, serial histological sections were acquired through the V3 and its encircling elements to elucidate their cross-sectional anatomy. Measurements of surgically and clinically important features were obtained with the aid of an operating microscope. This study reveals an astonishing anatomical resemblance between the suboccipital complex and the cavernous sinus, as follows: venous cushioning; anatomical properties of the V3 and those of the petrouscavernous internal carotid artery (ICA), namely their loops, branches, supporting fibrous rings, and periarterial autonomic neural plexus; adjacent nerves; and skull base locations. Likewise, a review of the literature showed a related embryological development and functional and pathological features, as well as similar transitional patterns in the arterial walls of the V3 and the petrous-cavernous ICA. -

7. Internal Jugular Vein the Internal Jugular Vein Is a Large Vein That Receives Blood from the Brain, Face, and Neck
د.احمد فاضل Lecture 16 Anatomy The Root of the Neck The root of the neck can be defined as the area of the neck immediately above the inlet into the thorax. Muscles of the Root of the Neck Scalenus Anterior Muscle Scalenus Medius Muscle The Thoracic Duct The thoracic duct begins in the abdomen at the upper end of the cisterna chyli. It enters the thorax through the aortic opening in the diaphragm and ascends upward, inclining gradually to the left. On reaching the superior mediastinum, it is found passing upward along the left margin of the esophagus. At the root of the neck, it continues to ascend along the left margin of the esophagus until it reaches the level of the transverse process of the seventh cervical vertebra. Here, it bends laterally behind the carotid sheath. On reaching the medial border of the scalenus anterior, it turns 1 downward and drains into the beginning of the left brachiocephalic vein. It may, however, end in the terminal part of the subclavian or internal jugular veins. Main Nerves of the Neck Cervical Plexus Brachial Plexus The brachial plexus is formed in the posterior triangle of the neck by the union of the anterior rami of the 5th, 6th, 7th, and 8th cervical and the first thoracic spinal nerves. This plexus is divided into roots, trunks, divisions, and cords. The roots of C5 and 6 unite to form the upper trunk, the root of C7 continues as the middle trunk, and the roots of C8 and T1 unite to form the lower trunk. -

Laszlo Mechtler, MD
1/16/2012 Summary Normal anatomy Normal varients Incidental findings Laszlo Mechtler MD Venous disease Co-director of Neuroimaging 1. Deep venous thrombosis 2. Cortical venous thrombosis Dent Neurologic Institute 3. Jugular vein thrombosis 4. CCSVI Buffalo NY 5. Benign Intracranial Hypertension 6. Venous obstruction due to neoplasm 7. Vein of Galan Malformation (21).Gre Green – Superior sagittal sinus Yellow- Basal dural sinuses Blue- Transverse sinuses 1 1/16/2012 superior sagittal sinus frontopolar [1], anterior frontal [2], superior sagittal sinus and posterior frontal [3] veins inferior sagittal sinus straight sinus confluence of the sinuses transverse sinuses sigmoid sinuses internal jugular veins Trolard vein [superior anastomotic vein] [4]; and anterior parietal veins [5]) and the larger named veins on the lateral surface of the cerebrum (the superficial sylvian vein [superficial middle cerebral vein] [6], which typically drains into the sphenoparietal sinus or the cavernous sinus, and the Labbé vein [7 Lateral MIP image from contrast-enhanced MR venography shows the major components of the deep venous system: the thalamostriate vein (1), septal vein (2), internal cerebral vein (3), basal vein (Rosenthal vein) (4), and vein of Galen (5). 1), septal vein (2), internal cerebral vein (3), basal vein (Rosenthal vein) (4), and vein of Galen (5). 2 1/16/2012 vein of Trolard – large anastomotic cerebral vein that courses cephalad from the sylvian fissure to the superior sagittal sinus – more dominant on the nondominant side vein of Labbe – courses posterolaterally from the sylvian fissure to the transverse sinus – more prominent on the dominant side Axial MR image with color overlay shows the drainage territory of the deep cerebral veins (internal cerebral vein, vein of Galen) (pink), in which parenchymal abnormalities due to deep venous occlusion typically arePink- found. -
Classification of Cavernous Sinus Fistulas
MEDICAL RADIOLOGY Diagnostic Imaging Editors: A. L. Baert, Leuven M. Knauth, Göttingen K. Sartor, Heidelberg Goetz Benndorf Dural Cavernous Sinus Fistulas Diagnostic and Endovascular Therapy Foreword by K. Sartor With 178 Figures in 755 Separate Illustrations, 540 in Color and 19 Tables 1 3 Goetz Benndorf, MD, PhD Associate Professor, Department of Radiology Baylor College of Medicine Director of Interventional Neuroradiology Ben Taub General Hospital One Baylor Plaza, MS 360 Houston, TX 77030 USA Medical Radiology · Diagnostic Imaging and Radiation Oncology Series Editors: A. L. Baert · L. W. Brady · H.-P. Heilmann · M. Knauth · M. Molls · C. Nieder · K. Sartor Continuation of Handbuch der medizinischen Radiologie Encyclopedia of Medical Radiology ISBN 978-3-540-00818-7 e-ISBN 978-3-540-68889-1 DOI 10.0007 / 978-3-540-68889-1 Medical Radiology · Diagnostic Imaging and Radiation Oncology ISSN 0942-5373 Library of Congress Control Number: 2004116221 © 2010, Springer-Verlag Berlin Heidelberg This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitations, broadcasting, reproduction on microfi lm or in any other way, and storage in data banks. Duplication of this publication or parts thereof is permit- ted only under the provisions of the German Copyright Law of September 9, 1965, in its current version, and permis- sion for use must always be obtained from Springer-Verlag. Violations are liable for prosecution under the German Copyright Law. The use of general descriptive names, trademarks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -
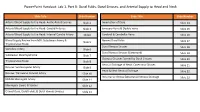
Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation.