Autonomic Function in Holmes Adie Syndrome
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Medical Diary Official Publication for the Federation of Medical Societies of Hong Kong
VOL.12 NO.9 SEPTEMBER 2007 ॷġ෫ġᚂġଉ THE HONG KONG MEDICAL DIARY OFFICIAL PUBLICATION FOR THE FEDERATION OF MEDICAL SOCIETIES OF HONG KONG www.fmshk.org Editorial Editorial Dr. Timothy YY Lai Medical Bulletin Management of Tearing in Adults Dr. Alan CK Ng Dr. Dylan DN Chan Ocular Allergy in Children Dr. Koon-man Lam Neuro-ophthalmology for General Practitioners: A Revision Dr.CarmenKMChan Normal Tension Glaucoma - a Sick Eye in a Sick Body Dr. Dexter YL Leung Retinal Complications of High Myopia Dr. Timothy YY Lai Amblyopia: An overview Dr. Wilson WK Yip Prof. Dorothy SP Fan Surgical Correction for Near Sightedness Dr. Arthur CK Cheng Traditional Chinese Medicine and Ophthalmology Dr. Jane CC Yeung Special Feature Rosiglitazone and Risk of Myocardial Infarction: Clear Danger or Dr. Norman Chan Media Hype? Clinical Quiz Clinical Quiz Dr. Helen KS Tung Society News Medical Diary of September Calendar of Events ISSN 1812 - 1691 ᚂᖒԙষΙড়ᒑȅᩧҕஶቆᜰЖ VOL.12 NO.9 SEPTEMBER 2007 Contents The Federation of Medical Societies of Hong Kong 4/F Duke of Windsor Social Service Building, Contents 15 Hennessy Road, Wanchai, Hong Kong Tel: 2527 8898 Fax: 2865 0345 Editorial President Dr. FONG To-sang, Dawson 方道生醫生 1st Vice- President Editorial 2 Dr. CHAN Chi-kuen 陳志權醫生 2nd Vice- President Dr. Timothy YY Lai Dr. LO Sze-ching, Susanna 盧時楨醫生 Hon. Secretary Dr. LO See-kit, Raymond 勞思傑醫生 Medical Bulletin Deputy Hon. Secretary Dr. CHAN Sai-kwing 陳世炯醫生 Management of Tearing in Adults 4 Hon. Treasurer Mr. LAM Lop-chi, Nelson 林立志先生 Dr.AlanCKNg Deputy Hon. Treasurer Dr. Dylan DN Chan Mr. -

Pupillary Disorders LAURA J
13 Pupillary Disorders LAURA J. BALCER Pupillary disorders usually fall into one of three major cat- cortex generally do not affect pupillary size or reactivity. egories: (1) abnormally shaped pupils, (2) abnormal pupillary Efferent parasympathetic fibers, arising from the Edinger– reaction to light, or (3) unequally sized pupils (anisocoria). Westphal nucleus, exit the midbrain within the third nerve Occasionally pupillary abnormalities are isolated findings, (efferent arc). Within the subarachnoid portion of the third but in many cases they are manifestations of more serious nerve, pupillary fibers tend to run on the external surface, intracranial pathology. making them more vulnerable to compression or infiltration The pupillary examination is discussed in detail in and less susceptible to vascular insult. Within the anterior Chapter 2. Pupillary neuroanatomy and physiology are cavernous sinus, the third nerve divides into two portions. reviewed here, and then the various pupillary disorders, The pupillary fibers follow the inferior division into the orbit, grouped roughly into one of the three listed categories, are where they then synapse at the ciliary ganglion, which lies discussed. in the posterior part of the orbit between the optic nerve and lateral rectus muscle (Fig. 13.3). The ciliary ganglion issues postganglionic cholinergic short ciliary nerves, which Neuroanatomy and Physiology initially travel to the globe with the nerve to the inferior oblique muscle, then between the sclera and choroid, to The major functions of the pupil are to vary the quantity of innervate the ciliary body and iris sphincter muscle. Fibers light reaching the retina, to minimize the spherical aberra- to the ciliary body outnumber those to the iris sphincter tions of the peripheral cornea and lens, and to increase the muscle by 30 : 1. -

Accommodation in the Holmes-Adie Syndrome by G
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.21.4.290 on 1 November 1958. Downloaded from J. Neurol. Neurosurg. Psychiat., 1958, 21, 290. ACCOMMODATION IN THE HOLMES-ADIE SYNDROME BY G. F. M. RUSSELL From the Neurological Research Unit, the National Hospital, Queen Square, London In 1936, Bramwell suggested that the title response to near and far vision respectively. But it "Holmes-Adie syndrome" be given to the clinical has also been noted that the reaction to convergence complex of a slowly reacting pupil and absent tendon may be remarkably wide in its range, considering reflexes in recognition of the descriptions by Holmes that it often follows a stage of complete paralysis (1931) and Adie (1932). Both authors had empha- (Strasburger, 1902). Not only is the reaction to sized the chief clinical features-dilatation of the convergence well preserved when compared to the pupil, apparent loss of the reaction to light, slow reaction to light, but it may in fact be excessive constriction and relaxation in response to near and (Alajouanine and Morax, 1938; Heersema and distant vision, and partial loss of the tendon reflexes. Moersch, 1939). In assessing the degree of tonicity Although the syndrome had been recognized wholly there are, therefore, two criteria: slowness ofguest. Protected by copyright. or in part many years previously (Strasburger, 1902; pupillary movement and preservation of the range Saenger, 1902; Nonne, 1902; Markus, 1906; Weill of movement. and Reys, 1926), credit must go to Adie for stressing Adler and Scheie (1940) showed that the tonic the benign nature of the disorder and distinguishing pupil constricts after the conjunctival instillation it clearly from neurosyphilis. -

Adie Syndrome: a Case Report
J Am Board Fam Pract: first published as 10.3122/jabfm.10.6.439 on 1 November 1997. Downloaded from Adie Syndrome: A Case Report T. Micheal Sherrill, MD, and DavidJ Lutz In 1932 Adie 1 described a syndrome in which were roughly equal, and the right corneal reflex unilateral accommodation and pupillary contrac was decreased. A rapid plasma reagin was ob tion were abnormal. It typically was observed in tained and found to be negative. The patient was young women with no history or evidence of subsequently referred to an ophthalmologist for syphilis and involved a unilateral dilated pupil confirmation of the diagnosis and to rule out that was unresponsive to light. He noted that other abnormalities. Confirmation was per deep tendon reflexes were absent or markedly di formed using'a dilute solution of pilocarpine. minished in these patients. He concluded that it was "a benign disorder sui generis." We report a Discussion recent case of Adie syndrome. Patients with Adie syndrome have anisocoria characterized by a dilated pupil that is minimally Case Report reactive or unresponsive to light. Deep tendon A 37-year-old woman came to the office with reflexes (knees and ankles) are either diminished right pupil dilatation. It was noticed by a nurse or absent.2 This disorder is most often seen in for the first time earlier that morning and had not young women, who have an average age of onset been present previously according to the patient's in their 30s. It usually occurs in one eye, but oc report. The patient's only visual complaint was curs bilaterally in up to 4 percent of patients.3 mild photophobia in sunlight. -

List of Symptoms Reported to Be Associated with Lyme Disease
List of Symptoms Reported to be Associated with Lyme Disease Abdominal pseudo-eventration Abdominal wall weakness Acrodermatitis chronica atrophicans (ACA) Acute Acral Ischemia Acute conduction disorders Acute coronary syndrome Acute exogenous psychosis Acute febrile illness Acute hemiparesis Acute ischaemic pontine stroke Acute meningitis Acute myelo-meningo-radiculitis Acute myelitis Acute pediatric monoarticular arthritis Acute peripheral facial palsy Acute perimyocarditis Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) Acute pyogenic arthritis Acute reversible diffuse conduction system disease Acute septic arthritis Acute severe encephalitis Acute transitory auriculoventricular block Acute transverse myelitis Acute urinary retention Acquired Immune Deficiency Syndrome (AIDS) Algodystrophy Allergic conditions Allergic conjunctivitis Alopecia Alzheimer’s Disease Amyotrophic lateral sclerosis (ALS - Lou Gehrig's Disease) Amyotrophy Anamnesis Anetoderma Anorexia nervosa Anterior optic neuropathy Antepartum fever Anxiety Arrhythmia Arthralgia Arthritis Asymmetrical hearing loss Ataxic sensory neuropathy Atraumatic spontaneous hemarthrosis Atrioventricular block Attention Deficit Disorder (ADD) Attention Deficit Hyperactivity Disorder (ADHD) Back pain without radiculitis Bannwarth’s Syndrome Behcet's disease Bell’s Palsy Benign cutaneous lymphocytoma Benign lymphocytic infiltration (Jessner-Kanof) Bilateral acute confluent disseminated choroiditis Bilateral carpal tunnel syndrome Bilateral facial nerve palsy Bilateral -

Miotic Adie's Pupils
Journal of Cll/lical Neuro-ophtllJllmology 9(1): 43-45, 1989. RilVen Press, Ltd., New York Miotic Adie's Pupils Michael L. Rosenberg, M.D. Two young adults, aged 24 and 31, had a long history of Adie's syndrome or, pupillotonia, is typically small, poorly reactive pupilS. There was no history of characterized by either unilaterally or bilaterally large pupils, and a review of old photographs confirmed enlarged pupils that are unresponsive to light (1). 10 and 5 years, respectively, of miosis. Both were found to have bilateral tonic pupils that were supersensitive to The diagnosis is made clinically by watching for a diluted pilocarpine. Although it is possible that they had tonic constriction to near stimulation followed by a an unusually early onset of bilateral Adie's syndrome tonic redilatation. with dilated pupils that was not noticed, it is suggested Two young adults are described who were noted that some patients might have primary miotic Adie's during routine examinations to have bilaterally mi pupils without ever passing through a mydriatic phase. Key Words: Adie's syndrome-Argyll Robertson pu otic pupils that were thought to be fixed to light. pils-Miosis. They were both referred for the evaluation of Ar gyll Robertson pupils. Evaluation revealed bilat eral tonic reactions to near stimulation in both pa tients, typical of Adie's tonic pupilS. The diagnosis of parasympathetic denervation was confirmed in both patients as their pupils constricted with di luted pilocarpine. The cases reinforce the principle that any pupil regardless of size should be evalu ated for the possibility of pupillotonia. -

Fascicular Oculomotor Nerve Palsy Due to a Strategic Midbrain Infarction: the ‘Eyes’ Have It Ashin Varghese1, Boby Varkey Maramattom2
J R Coll Physicians Edinb 2021; 51: 272–4 | doi: 10.4997/JRCPE.2021.314 IMAGE OF THE QUARTER Fascicular oculomotor nerve palsy due to a strategic midbrain infarction: the ‘eyes’ have it Ashin Varghese1, Boby Varkey Maramattom2 ClinicalKeywords: fascicular oculomotor nerve palsy, midbrain infarction, third nerve palsy Correspondence to: Ashin Varghese Financial and Competing Interests: No confl ict of interests declared. Department of Neurology, Aster Medcity, Kochi Informed Consent: Written informed consent for the paper to be published (including Kerala images, case history and data) was obtained from the patient for publication of this paper, India including accompanying images. Email: drashin.varghese@ asterhospital.com A 38-year-old female with acute lymphoblastic leukaemia Her white blood cell count was 65,000/cmm3, haemoglobin on treatment was admitted with new onset diplopia of was 6 gm% and platelet counts were 20,000/cmm3. Other two days duration. She had recently fi nished a course of routine blood investigations were normal. The combination of anti-tuberculous treatment for pulmonary tuberculosis. On unilateral ptosis, monocular downgaze palsy and ipsilateral examination, she afebrile, had a partial ptosis of the right unreactive pupil suggested involvement of different structures eye, a right fi xed and dilated pupil, and impaired downgaze innervated by the right oculomotor nerve. Only the LPS muscle, most evident in the primary position and medially suggestive the pupillomotor fi bres and the right IR (the primary depressor of IR palsy (Figures 1 and 2). Other movements of the right of the eye) were affected. The other muscles innervated by eye were preserved. -
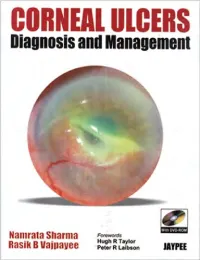
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Association Between Helicobacter Pylori Infection and Posner–Schlossman Syndrome
Eye (2010) 24, 64–69 & 2010 Macmillan Publishers Limited All rights reserved 0950-222X/10 $32.00 www.nature.com/eye 1 1 1 1 2 CLINICAL STUDY Association between CY Choi , MS Kim , JM Kim , SH Park , KH Park and C Hong3 Helicobacter pylori infection and Posner–Schlossman syndrome Abstract uncommon unilateral syndrome with recurrent attacks of anterior non-granulomatous uveitis Objective: To investigate possible association and elevated intraocular pressure (IOP). With between Helicobacter pylori infection and acute attack, IOP is typically 40–60 mmHg. After Posner–Schlossman syndrome. an acute attack, IOP and facility of aqueous Methods: In a prospective study, 40 subjects outflow return to normal.1 It has been with Posner–Schlossman syndrome were considered as a benign, self-limited disease examined. As a control group, 73 subjects because short-term use of topical corticosteroids without Posner–Schlossman syndrome were and antiglaucoma medications usually control selected for comparison with the study group. the attacks. But the aetiology of PSS remains 1 All participants underwent serologic analysis Department of still unknown, so there have been numerous Ophthalmology, for the presence of H. pylori infection by postulations for the pathogenesis of PSS Sungkyunkwan University an enzyme-linked immunosorbent assay. including abnormal vascular reactivity, School of Medicine, Positive rate of serum anti-H. pylori IgG Kangbuk Samsung Hospital, autonomic dysregulation, and infections. was compared between Posner–Schlossman Seoul, Korea Herpes simplex virus or cytomegalovirus has syndrome patients and control participants. been suggested as aetiologies for PSS due to 2 Results: The rate of positive titre Department of their presence in the aqueous humour during Ophthalmology, Seoul (415 U/ml) of H. -

NLM Technical Bulletin, No.1-20
LIBRARY NETWORK/MEDLARS technical bulletin 1969 MAY through DECEMBER NUMBERS 1-8 (Numbers 1-6 issued as MEDLARS/Network Technical Bulletin) Issued by The Office of the Associate Director for Library Operations National Library of Medicine U.S. DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE Public Health Service National Institutes of Health INDEX TO LIBRARY NETWORK/MEDLARS TECHNICAL BULLETIN* * May-December 1969, Numbers 1-8 SUBJECT Issue Number Page ABRIDGED INDEX MEDICUS 7 11 BIBLIOGRAPHIC SERVICES DIVISION Annual Report 3 14 BIBLIOGRAPHIES see Publications CCF (Compressed Citation File) Change in Citation Numbering of July 1969 CCF 2 7 Change in Coverage of Search Files 1 6 One Million Citations 4 9 Statistics on January-June 1969 CCF 2 8 FOREIGN COUNTRIES European Searchers Workshop 3 5 Foreign ILL Requests to RMLs 7 8 Restriction of Services to Foreign Countries (Search) 6 7 FORMS MEDLARS Search Appraisal Form Changes 2 5 New Indexing Data Form 2 14 HEALTH SCIENCES BIBLIOGRAPHIC CLEARINGHOUSE 8 5 HEDGES see also Search Eye 5 8 Narcotics - A Partial Hedge 6 14 Radiology 8 14 Tropical Countries 5 6 HOSPITAL LIBRARIES Workshops and Courses for Hospital Library Personnel 7 14 INDEX MEDICUS 7 11 INDEXING Discontinuation of Designation of Journals as "Depth" or "Non-Depth" 3 4 Index Section Check List 2 10 3 13 4 9 Index Section Current Developments 2 9 Index Section Developments for 1970 4 7 New Indexing Data Form 2 14 Pharmacy and Pharmacology: MEDLARS Indexing Instructions 3 15 1970 Indexing 6 12 *Nos. 1-* issued as MEDLARS/Network Technical -

Differential Diagnoses
Differential diagnoses RETINA • CNVM Degenerative ARMD myopic degeneration angioid streaks choroidal hemangioma juxtafoveal retinal telangiectasia osteogenesis imperfecta optic nerve head pit retinochoroidal coloboma tilted optic disc Heredodegenerative Vitelliform macular dystrophy Fundus flavimaculatus Optic nerve head drusen choroideremia RP with exudate Inflammatory Ocular histoplasmosis syndrome Multifocal choroiditis (white dot syndromes) Serpiginous choroiditis Toxoplasmosis Toxocariasis Rubella Vogt-Koyanagi-Harada syndrome Behcet syndrome Sympathetic ophthalmia Central serous retinopathy sarcoid syphilis chronic uveitis AMPEE Neoplastic Choroidal nevus Choroidal hemangioma Metastatic choroidal tumors Hamartoma of the RPE choroidal osteoma malignant melanoma optic nerve glioma with chronically swollen nerve Traumatic Choroidal rupture Intense photocoagulation IOFB retinal cryoinjury surgical trauma subretinal fluid drainage site Idiopathic • CME post-op Irvine-Gass syndrome corneal surgery retinal surgery laser iridotomy cryo for retinal tear PRP aphakia pseudophakia inherited / dystrophies RP autosomal dominant CME juvenile retinoschisis Goldmann-Favre disease medications Xalatan topical epinephrine nicotinic acid tumors differentials 1 choroidal melanoma / nevi choroidal hemangioma retinal capillary hemangioma tractional ERM vitreomacular traction syndrome inflammatory Eale's CMV pars planitis Behcet Birdshot sarcoidosis idiopathic vitritis scleritis toxo vascular DR CRVO BRVO OIS retinal juxtafoveal telangiectasia CNVM Coat's -
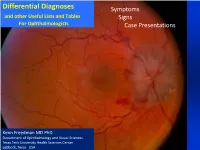
Differential Diagnoses Symptoms and Other Useful Lists and Tables Signs for Ophthalmologists Case Presentations
Differential Diagnoses Symptoms and other Useful Lists and Tables Signs For Ophthalmologists Case Presentations Kenn Freedman MD PhD Department of Ophthalmology and Visual Sciences Texas Tech University Health Sciences Center Lubbock, Texas USA Acknowledgments and Disclaimer The differential diagnoses and lists contained herein are not meant to be exhaustive, but are to give in most cases the most common causes of many ocular / visual symptoms, signs and situations. Included also in these lists are also some less common, but serious conditions that must be “ruled-out”. These lists have been based on years of experience, and I am grateful for God’s help in developing them. I also owe gratitude to several sources* including Roy’s classic text on Ocular Differential Diagnosis. * Please see references at end of document This presentation, of course, will continue to be a work in progress and any concerns or suggestions as to errors or omissions or picture copyrights will be considered. Please feel free to contact me at [email protected] Kenn Freedman Lubbock, Texas - October 2018 Disclaimer: The diagnostic algorithm for the diagnosis and management of Ocular or Neurological Conditions contained in this presentation is not intended to replace the independent medical or professional judgment of the physician or other health care providers in the context of individual clinical circumstances to determine a patient’s care. Use of this Presentation The lists are divided into three main areas 1. Symptoms 2. Signs from the Eight Point Eye Exam 3. Common Situations and Case Presentations The index for all of the lists is given on the following 3 pages.