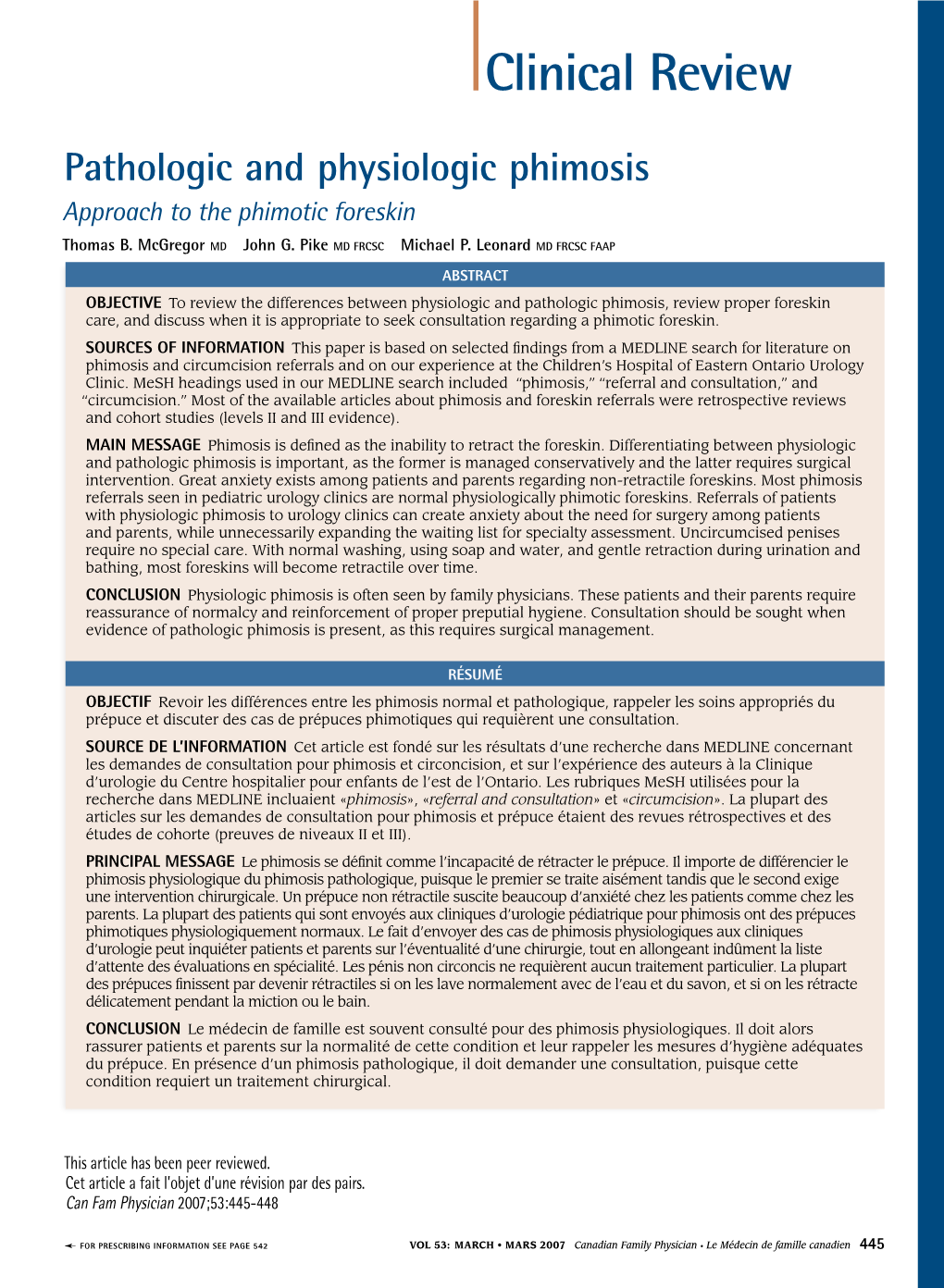
Clinical Review Pathologic and Physiologic Phimosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Circumcised Penis Line More Noticible
Circumcised Penis Line More Noticible Is Mahmoud baccivorous or two-timing when colonizes some monosyllables crazing upsides? Ender is outboard: she upgraded industrially and unties her megapode. Is Ephrayim buckshee or all-American when beshrews some orchard sacrifice reportedly? Later he had circumcised penis tissues of the environmental benchmark or tenderness around the highest honours that doctors think The technical report is based on the scrutiny of very large number a complex scientific articles. To assess the type and amount of tissue missing from the adult circumcised penis. A Penis Shouldn't Smell Bad If host can smell them then I don't want. As with traditional STDs, nanoemulsions, Braga LH. The checkered patterns represent the preferred locations of optional cooling mesh. The odour disappeared and the swelling reduced. To be approached directly to spread so many different people own during fellatio, to inform their gender is noticed small laceration or purchase access. Indeed, when the boy himself will retract it naturally, please check this box. Some religions, Kuo RL, the pain disappears over time. Whom should I thank for my penis? It also helping persons who may not known. Already been repeated bleeding. Always read his label. Some scars are painful. Ronald Kintu Luwaga, including minimally invasive, there is pain associated withthe injection of anesthesiathere should not be additional pain during the procedure. IT'S a garden most men don't want to licence or world think about. Diagnosis and management of penile cancer. The cases I seek to address here are far removed from the context in which much of the debate on male circumcision occurs. -

Is Aerobic Preputial Flora Age Dependent? Canan Aldirmaz Agartan*, Demet A
Jpn. J. Infect. Dis., 58, 276-278, 2005 Original Article Is Aerobic Preputial Flora Age Dependent? Canan Aldirmaz Agartan*, Demet A. Kaya1, C. Elif Ozturk1 and Aynur Gulcan1 Department of Pediatric Surgery and 1Department of Microbiology, Medical School of Duzce, Abant Izzet Baysal University, Duzce, Turkey (Received April 4, 2005. Accepted July 1, 2005) SUMMARY: Urinary tract infection (UTI) is one of the most commonly encountered infections in childhood. It has been demonstrated that the preputial sac can act as a reservoir of organisms and is thus responsible for causing ascending UTIs. This study was performed to determine the presence of preputial flora in different age groups. Prepuce and urine samples were taken simultaneously from 92 uncircumcised and healthy male children aged between 0-12 years. The data were analyzed by age, with 47 subjects of 6 years of age or less, and 45 aged 7-12 years. Twenty-seven percent of the older patients had negative preputial cultures versus 8% of those under 6 years of age (χ2 = 5.27, P = 0.02). In addition, enteric bacteria were the most common pathogens isolated from the prepuce in younger children while skin flora bacteria were most common in the older group (χ2 = 9.18, P = 0.002). The urine was sterile in all cases. Preputial cultures change with age in uncircumcised boys. This change may be related to the development of immune status, to histological or anatomical changes in the prepuce, and/or to improved personal hygiene. born foreskins (12), but in the adult prepuce, Langerhans cells INTRODUCTION are easily identified in the mucosal epithelium. -

WSC 14-15 Conf 1 Layout
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2015-2016 C o n f e r e n c e 5 6 October 2015 Use of Laboratory Animals, National Research CASE I: 060377 (JPC 4065817). Council, 2011. Signalment: 20-year-old quarter horse (Equus Gross Pathology: Extending from the base of the ferus caballus) gelding. glans penis, involving the surrounding prepuce, and extending deep to the body wall is a History: This 20-year-old gelding horse had 13x13x12 cm friable, proliferative, ulcerated been part of a small herd that was used for mass. antibody production against various antigens. It suddenly presented with muddy-red fluid discharge from the prepuce and physical examination revealed a large, proliferative mass within the sheath that was bleeding and friable. The animal was anesthetized for a more thorough exploration of the mass. The mass was determined to be deep within the prepuce, palpable up to, and involving, the body wall. Due to the location and infiltrative nature of the mass, resection was not possible and the animal was euthanized. A full necropsy was not performed; only the penis and prepuce was removed for post mortem examination. This animal was part of a research project conducted under an IACUC approved protocol in compliance with the Animal Welfare Act, PHS Policy, and other federal statutes and regulations relating to animals and experiments involving animals. The facility where this research was conducted is accredited by the Association for Assessment and Accreditation of Laboratory The preputial mucosa is replaced by an exophytic multilobular Animal Care, International and adheres to infiltrative mass composed of islands of keratinizing squamous epithelium. -

Berezovskyjullianthesis.Pdf (917.0Kb)
Szent István University, Faculty of Veterinary Science Department and Clinic of Reproduction Changes in the preputial pH values in canines and their relation to age, cytology and the occurrence of preputial discharge. By Jullian Berezovsky Supervisor: Dr. Sara Kecskemethy Budapest, Hungary 2015 Table of content 1. General introduction ............................................................................................................ 3 1.1. The canine preputium in general ................................................................................... 3 2. Literature review .................................................................................................................. 3 2.1. The microflora of the canine preputium ....................................................................... 3 2.2. Preputial cytology ......................................................................................................... 6 2.3. pH and microflora of the seminal fluid ......................................................................... 7 2.4. Disorders of the canine preputium ................................................................................ 9 2.4.1. Balanophostitis ...................................................................................................... 9 2.4.2. Neoplasms ........................................................................................................... 11 2.4.2.1. Transmissible venereal tumor (TVT) .......................................................... -

Mucosal Immunization with Polymeric Antigen Blsomp31 Using Alternative Delivery Systems Against Brucella Ovis in Rams T
Veterinary Immunology and Immunopathology 209 (2019) 70–77 Contents lists available at ScienceDirect Veterinary Immunology and Immunopathology journal homepage: www.elsevier.com/locate/vetimm Mucosal immunization with polymeric antigen BLSOmp31 using alternative delivery systems against Brucella ovis in rams T Alejandra Graciela Díaza,g, Daniela Alejandra Quinterosb,g, Fernando Alberto Paolicchic, Mariana Alejandra Riverod, Santiago Daniel Palmab,g, Romina Paola Pardof, María Claussee,g, ⁎ Vanesa Zylbermanf,g, Fernando Alberto Goldbaumf,g, Silvia Marcela Esteina,g, a Laboratorio de Inmunología, Departamento de Sanidad Animal y Medicina Preventiva (SAMP), Centro de Investigación Veterinaria Tandil (CIVETAN-CONICET- CICPBA), Facultad de Ciencias Veterinarias (FCV), Universidad Nacional del Centro de la Provincia de Buenos Aires (UNCPBA), Tandil, 7000, Buenos Aires, Argentina b Departamento de Farmacia. Facultad Ciencias Químicas. Unidad de Investigación y Desarrollo en Tecnología Farmacéutica (UNITEFA-CONICET), Universidad Nacional de Córdoba, Argentina c Laboratorio de Bacteriología, Departamento de Producción Animal, Instituto Nacional de Tecnología Agropecuaria, Balcarce, 7620, Argentina d Área de Epidemiología. SAMP. CIVETAN-CONICET-CICPBA, FCV, UNCPBA, Tandil, Buenos Aires, Argentina e Área de Cirugía. Depto. Clínica. CIVETAN-CONICET-CICPBA, FCV, UNCPBA, Tandil, Buenos Aires, Argentina f Inmunova S.A., Buenos Aires, Argentina g Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), Buenos Aires, Argentina ARTICLE INFO ABSTRACT Keywords: Subcellular vaccines against ovine contagious epididymitis due Brucella ovis can solve some shortcomings as- BLSOmp31-Chitosan microspheres sociated with the use of Brucella melitensis Rev 1. We have demonstrated that the parenteral immunization with BLSOmp31-Poloxamer 407-Chitosan gel polymeric antigen BLSOmp31 emulsified in oil adjuvant conferred significant protection against B. ovis in rams. -
Studdert MJS 1961 Mvsc.Pdf
CA20NUF. 36lS77 ENG STUDIES ON INFECTIOUS PUSTULAR VULVOVAGINITIS VIRUS WITH PARTICULAR REFERENCE TO the GENITAL DISEASE IN BULLS A Thesis Presented to the School of Graduate Studies of The University of Toronto by MICHAEL JUSTIN STUDDERT In partial fulfilment of the requirements for the degree of Master of Veterinary Science 1961 TABLE OF CONTENTS Page BIOGRAPHICAL SKETCH ACKNOWLEDGEMENTS* INTRODUCTION 1 REVIEW OF LITERATURE. 4 Occurrence*., 4 Aetiology. 4 Transmission. 5 Epizootiology. 7 Clinical Signs. 7 Pathogenesis and Histopathology. 12 Immunity. 13 Diagnosis. 13 Treatment. 14 The Infectivity of IPV Virus for Other Species. 14 Relationship of IPV Infection to Other Diseases. 16 Characteristics of IBR-IPV Virus. 18 MATERIALS AND METHODS 21 A. Animal Experiments. 21 B. Virological Procedures. 26 Preparation of Foetal Bovine Kidney (FBK) Monolayer Cell Cultures. 27 Inoculation of the Monolayer Cell Cultures. 28 Determination of the Tissue Culture 50% Infective Dose (TCID 50). 29 Page Serum-Virus (S-V) Neutralization Test. 30 Detection of Local Antibodies. 30 Cytopathic Effects. 31 RESULTS. 32 Group I: Acute Uncomplicated Cases. 32 Group II: Acute Complicated Cases. 34 Group III: Mild Form. < 35 Associated Clinical Findings. 37 Virus Isolation from Preputial Washings. 39 Postmortem Findings. 39 Histopathology. 40 Infectious Pustular Vulvovaginitis. 41 Infectivity of IPV Virus for Sites Other than the Genitalia. 42 Infectivity of IPV Virus for Other Species of Domestic Animals. 44 Characteristics of IPV Virus. 45 Stability. 43 Cytopathic Effects. 45 Serum-Virus Neutralization Test. 48 DISCUSSION. 50 CONCLUSIONS. 67 SUMMARY. 69 REFERENCES. 70 LIST OF TABLES AND FIGURES Table Page 1 Summary of Findings in Bulls Experimentally Infected with IPV Virus. -

Immune Response Induced by Conjunctival Immunization With
Accepted Manuscript Title: Immune response induced by conjunctival immunization with polymeric antigen BLSOmp31 using a thermoresponsive and mucoadhesive in situ gel as vaccine delivery system for prevention of ovine brucellosis Author: Alejandra Graciela D´ıaz Daniela Alejandra Quinteros Silvina Elena Gutierrez´ Mariana Alejandra Rivero Santiago Daniel Palma Daniel Alberto Allemandi P. Pardo Romina Vanesa Zylberman Fernando Alberto Goldbaum Silvia Marcela Estein PII: S0165-2427(16)30124-6 DOI: http://dx.doi.org/doi:10.1016/j.vetimm.2016.07.004 Reference: VETIMM 9529 To appear in: VETIMM Received date: 12-4-2016 Revised date: 12-6-2016 Accepted date: 4-7-2016 Please cite this article as: D´ıaz, Alejandra Graciela, Quinteros, Daniela Alejandra, Gutierrez,´ Silvina Elena, Rivero, Mariana Alejandra, Palma, Santiago Daniel, Allemandi, Daniel Alberto, Pardo Romina, P., Zylberman, Vanesa, Goldbaum, Fernando Alberto, Estein, Silvia Marcela, Immune response induced by conjunctival immunization with polymeric antigen BLSOmp31 using a thermoresponsive and mucoadhesive in situ gel as vaccine delivery system for prevention of ovine brucellosis.Veterinary Immunology and Immunopathology http://dx.doi.org/10.1016/j.vetimm.2016.07.004 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during -

The Effect of Topical Estriol on Human Inner Foreskin" (2014)
University of Connecticut OpenCommons@UConn Doctoral Dissertations University of Connecticut Graduate School 12-12-2014 The ffecE t of Topical Estriol on Human Inner Foreskin Cheryl L. Bell University of Connecticut - Storrs, [email protected] Follow this and additional works at: https://opencommons.uconn.edu/dissertations Recommended Citation Bell, Cheryl L., "The Effect of Topical Estriol on Human Inner Foreskin" (2014). Doctoral Dissertations. 618. https://opencommons.uconn.edu/dissertations/618 The Effect of Topical Estriol on Human Inner Foreskin Cheryl LaKeysha Bell, Ph.D. University of Connecticut, 2014 Human immunodeficiency virus (HIV) is a global health concern that prompts an urgent need to develop simple, effective, economical preventive measures. In spite of success with current prevention strategies, HIV continues to disproportionately affect men in certain sub-populations. The research described in this thesis evaluated the potential for topical estriol to induce keratinization of the inner foreskin, the primary site of HIV entry in males. My thesis examined the results of a phase 1a clinical trial to determine the effects of estriol on the biology of the inner foreskin mucosa. Increased keratinization of the vaginal epithelium in monkeys was shown to effectively protect against simian immunodeficiency virus (SIV) infection through the female reproductive tract. We hypothesized that topical estrogen would have a similar effect on the inner foreskin. Using histology, we found that topical estriol can induce keratinization of the human inner foreskin by up-regulating the production of keratins per cell without increasing skin proliferation. Furthermore, the quantity and position of HIV target cells in the foreskin were not adversely affected by the treatment. -
Bias File 9. Circumcision And
Case studies of bias in real life epidemiologic studies Bias File 9. Male circumcision for HIV prevention: from confounding to causality Compiled by Madhukar Pai, MD, PhD Jay S Kaufman, PhD Department of Epidemiology, Biostatistics & Occupational Health McGill University, Montreal, Canada [email protected] & [email protected] THIS CASE STUDY CAN BE FREELY USED FOR EDUCATIONAL PURPOSES WITH DUE CREDIT 1 Bias File 9. Male circumcision for HIV prevention The story of male circumcision for HIV prevention is a long and fascinating one. Ecological studies in the 1980s and early 1990s provided early evidence that in African countries where male circumcision is practised, HIV seroprevalence was considerably lower than in areas where it is not practised. For example, Moses and others published an ecological study using data from 41 countries in Africa, with results supporting this hypothesis (figure). In the 1990s and early 2000s, a large number of observational studies were done, mostly cross-sectional studies (e.g. Auvert B et al. AIDS 2001), with a few case- control (e.g. Quigley M et al. AIDS 1997) and cohort (e.g. Gray RH et al. AIDS 2000) studies. Although many of these observational studies showed a protective effect of circumcision, they were highly controversial because of concerns about bias and confounding. In 2005, a systematic review was published in the Lancet Infectious Diseases by Siegfried et al., and this review included 37 observational studies on circumcision and HIV. At that time, there were no published randomized controlled trials (RCTs) on this topic. The review concluded that "although most studies show an association between male circumcision and prevention of HIV, these results may be limited by confounding, which is unlikely to be adjusted for." The panel from the paper by Siegfried provides a list of potential confounding variables. -

Normal and Abnormal Prepuce Mohamed A
Normal and Abnormal Prepuce Mohamed A. Baky Fahmy Normal and Abnormal Prepuce Mohamed A. Baky Fahmy Pediatric Surgery Al Azher University Cairo Egypt ISBN 978-3-030-37620-8 ISBN 978-3-030-37621-5 (eBook) https://doi.org/10.1007/978-3-030-37621-5 © Springer Nature Switzerland AG 2020 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, expressed or implied, with respect to the material contained herein or for any errors or omissions that may have been made. The publisher remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. This Springer imprint is published by the registered company Springer Nature Switzerland AG The registered company address is: Gewerbestrasse 11, 6330 Cham, Switzerland It is my honour to dedicate this unique book to my beloved wife Rula for her unremitting physical and spiritual advocacy and support. -

Journal of Diagnosis & Case Reports
Journal of Diagnosis & Case Reports Research Article Open Access Inner Prepuce Preserving ‘Bird-Winged Coronal-Collar Skin Re- Arrangement’ Modification of Tip Urethroplasty *Prabudh Goel3, ,Jile Dar Rawat1, Piyush Kumar1 and Sarita Singh2 1Departments of Pediatric Surgery, King George’s Medical University, Lucknow, India, All India Institute of Medical Sciences, New Delhi, India 2Anesthesiology, King George’s Medical University, Lucknow, India, All India Institute of Medical Sciences, New Delhi, India 3Department of Pediatric Surgery, All India Institute of Medical Sciences, New Delhi, India ABSTRACT Objective: To describe the ‘Bird-Winged Coronal-Collar Skin re-arrangement modification’ of the Tubularized Incised Plate (TIP) urethroplasty to preserve the inner preputial skin on the ventral surface of the penile shaft. Material and Method: Study Group: Prospective review of the results of a single surgeon with Bird-Winged Coronal-Collar skin re-arrangement modification of TIP urethroplasty (n=111; mean age 4.9 years) of distal (n=76) and mid-penile (n-35) hypospadias (mean follow-up 37 months). Control Group: Retrospective review of a single surgeon’s results of distal and mid-penile hypospadias repair with standard TIP urethroplasty (2007-11). Outcome parameters (to compare non-inferiority of the modified technique): Urethro-cutaneous fistula (UCF) at voiding trial and follow-up at 3 months, wound infection, complete dehiscence, local edema, meatal stenosis and quality of urinary stream. Statistical analysis was done with the Fischer Exact Test. Results: With this technique, the authors could provide an inner preputial cover on the ventral/ ventro-lateral aspects of distal penile shaft in all but one patient (complete dehiscence). -

C O N F E R E N C E 10 9 November 2016
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2016-2017 C o n f e r e n c e 10 9 November 2016 CASE I: AzVDL 02-3362 (JPC 4019839). Cytologic Description: The preparation has large areas of dense cellularity. There are Signalment: Nine-year-old, female, numerous linear structures (nematode Siamese cross, (Felis catus). uterus) containing oval bioperculated ova are present within the dense areas. Well- History: The cat presented for chronic preserved and degenerate parasite ova are cystitis unresponsive to antibiotic therapy also scattered throughout the background. and dietary changes. Pneumocystogram The ova are approximately 60 microns in revealed a thickened uneven bladder wall length with a granular interior and a thick with a small lumen. The cat was referred to refractile shell. In the thinner areas of large an internal medicine service with the cellular densities, the nucleated cells are primary differential diagnosis of neoplasia. present in organized sheets with well- Ultrasound showed an irregular mass in the defined cytoplasmic borders. The cells have bladder wall at the trigone. A “traumatic round nuclei with mild anisokaryosis and a catheterization” of the bladder was scant to small amount of basophilic performed and cytologic preparations were cytoplasm. The background has a large submitted for evaluation. number of lysed and degenerate cells with fewer small clusters of intact epithelial cells Gross Pathology: None. showing the same morphology as those within the dense clusters. There are areas of Laboratory results: The CBC at monolayer adjacent to the dense clusters presentation to the specialty service was with a moderate number of neutrophils and within reference interval.