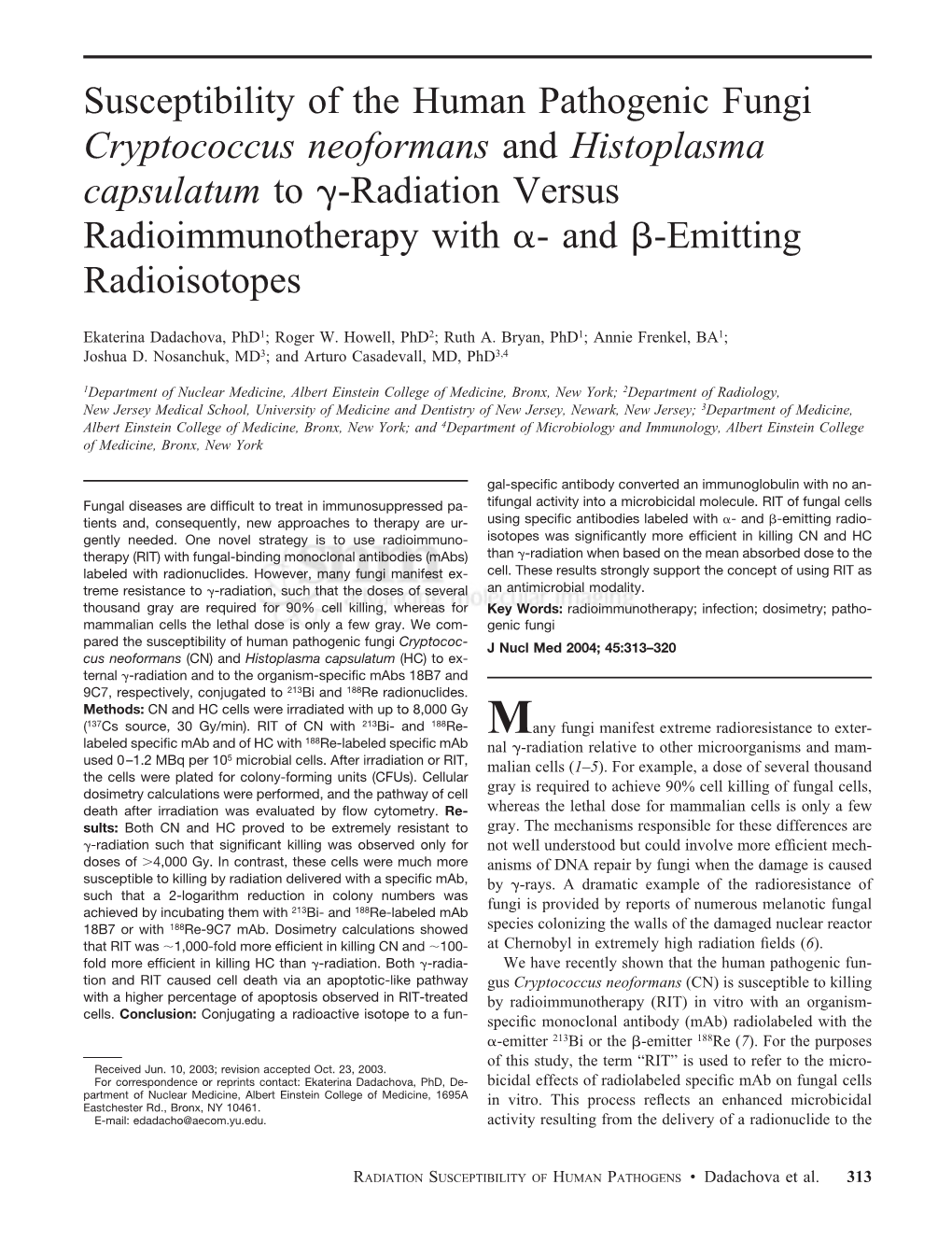
Cryptococcus Neoformans and Histoplasma Capsulatum to ␥-Radiation Versus Radioimmunotherapy with ␣- and -Emitting Radioisotopes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bats (Myotis Lucifugus)
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln The Handbook: Prevention and Control of Wildlife Damage Management, Internet Center Wildlife Damage for January 1994 Bats (Myotis lucifugus) Arthur M. Greenhall Research Associate, Department of Mammalogy, American Museum of Natural History, New York, New York 10024 Stephen C. Frantz Vertebrate Vector Specialist, Wadsworth Center for Laboratories and Research, New York State Department of Health, Albany, New York 12201-0509 Follow this and additional works at: https://digitalcommons.unl.edu/icwdmhandbook Part of the Environmental Sciences Commons Greenhall, Arthur M. and Frantz, Stephen C., "Bats (Myotis lucifugus)" (1994). The Handbook: Prevention and Control of Wildlife Damage. 46. https://digitalcommons.unl.edu/icwdmhandbook/46 This Article is brought to you for free and open access by the Wildlife Damage Management, Internet Center for at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in The Handbook: Prevention and Control of Wildlife Damage by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Arthur M. Greenhall Research Associate Department of Mammalogy BATS American Museum of Natural History New York, New York 10024 Stephen C. Frantz Vertebrate Vector Specialist Wadsworth Center for Laboratories and Research New York State Department of Health Albany, New York 12201-0509 Fig. 1. Little brown bat, Myotis lucifugus Damage Prevention and Air drafts/ventilation. Removal of Occasional Bat Intruders Control Methods Ultrasonic devices: not effective. When no bite or contact has occurred, Sticky deterrents: limited efficacy. Exclusion help the bat escape (otherwise Toxicants submit it for rabies testing). Polypropylene netting checkvalves simplify getting bats out. None are registered. -

Monoclonal Antibodies As Tools to Combat Fungal Infections
Journal of Fungi Review Monoclonal Antibodies as Tools to Combat Fungal Infections Sebastian Ulrich and Frank Ebel * Institute for Infectious Diseases and Zoonoses, Faculty of Veterinary Medicine, Ludwig-Maximilians-University, D-80539 Munich, Germany; [email protected] * Correspondence: [email protected] Received: 26 November 2019; Accepted: 31 January 2020; Published: 4 February 2020 Abstract: Antibodies represent an important element in the adaptive immune response and a major tool to eliminate microbial pathogens. For many bacterial and viral infections, efficient vaccines exist, but not for fungal pathogens. For a long time, antibodies have been assumed to be of minor importance for a successful clearance of fungal infections; however this perception has been challenged by a large number of studies over the last three decades. In this review, we focus on the potential therapeutic and prophylactic use of monoclonal antibodies. Since systemic mycoses normally occur in severely immunocompromised patients, a passive immunization using monoclonal antibodies is a promising approach to directly attack the fungal pathogen and/or to activate and strengthen the residual antifungal immune response in these patients. Keywords: monoclonal antibodies; invasive fungal infections; therapy; prophylaxis; opsonization 1. Introduction Fungal pathogens represent a major threat for immunocompromised individuals [1]. Mortality rates associated with deep mycoses are generally high, reflecting shortcomings in diagnostics as well as limited and often insufficient treatment options. Apart from the development of novel antifungal agents, it is a promising approach to activate antimicrobial mechanisms employed by the immune system to eliminate microbial intruders. Antibodies represent a major tool to mark and combat microbes. Moreover, monoclonal antibodies (mAbs) are highly specific reagents that opened new avenues for the treatment of cancer and other diseases. -

HHE Report No. HETA-92-0348-2361, First United
ThisThis Heal Healthth Ha Hazzardard E Evvaluaaluationtion ( H(HHHEE) )report report and and any any r ereccoommmmendendaatitonsions m madeade herein herein are are f orfor t hethe s sppeeccifiicfic f afacciliilityty e evvaluaaluatedted and and may may not not b bee un univeriverssaalllyly appappliliccabable.le. A Anyny re reccoommmmendaendatitoionnss m madeade are are n noot tt oto be be c consonsideredidered as as f ifnalinal s statatetemmeenntsts of of N NIOIOSSHH po polilcicyy or or of of any any agen agenccyy or or i ndindivivididuualal i nvoinvolvlved.ed. AdditionalAdditional HHE HHE repor reportsts are are ava availilabablele at at h htttptp:/://ww/wwww.c.cddcc.gov.gov/n/nioiosshh/hhe/hhe/repor/reportsts ThisThis HealHealtthh HaHazzardard EEvvaluaaluattionion ((HHHHEE)) reportreport andand anyany rreeccoommmmendendaattiionsons mmadeade hereinherein areare fforor tthehe ssppeecciifficic ffaacciliilittyy eevvaluaaluatteded andand maymay notnot bbee ununiiververssaallllyy appappapplililicccababablle.e.le. A AAnynyny re rerecccooommmmmmendaendaendattitiooionnnsss m mmadeadeade are areare n nnooott t t totoo be bebe c cconsonsonsiideredderedidered as asas f fifinalnalinal s ssttataatteteemmmeeennnttstss of ofof N NNIIOIOOSSSHHH po popolliilccicyyy or oror of ofof any anyany agen agenagencccyyy or oror i indndindiivviviiddiduuualalal i invonvoinvollvvlved.ed.ed. AdditionalAdditional HHEHHE reporreporttss areare avaavaililabablele atat hhtttpp::///wwwwww..ccddcc..govgov//nnioiosshh//hhehhe//reporreporttss This Health Hazard Evaluation (HHE) report and any recommendations made herein are for the specific facility evaluated and may not be universally applicable. Any recommendations made are not to be considered as final statements of NIOSH policy or of any agency or individual involved. Additional HHE reports are available at http://www.cdc.gov/niosh/hhe/reports HETA 92-0348-2361 NIOSH INVESTIGATOR: OCTOBER 1993 STEVEN W. -

Histoplasma Capsulatum Antibody
Lab Dept: Serology Test Name: HISTOPLASMA CAPSULATUM ANTIBODY General Information Lab Order Codes: HAB – Complement Fixation Synonyms: Histoplasma Antibody, Serum; Histoplasma Ab; Histoplasma Complement Fixation; Immunodiffusion for Fungi CPT Codes: 86698 X3 - Antibody; histoplasma Test Includes: Histoplasma Antibody by Complement Fixation Logistics Test Indications: Useful as an aid in the diagnosis of respiratory disease when Histoplasma infection is suspected. Histoplasma capsulatum is a soil saprophyte that grows well in soil enriched with bird droppings. The usual disease is self-limited, affects the lungs and is asymptomatic. Chronic cavitary pulmonary disease, disseminated disease, and meningitis may occur and can be fatal, especially in young children and in immunosuppressed patients. Lab Testing Sections: Serology - Sendouts Referred to: Mayo Medical Laboratories (Mayo Test: SHSTO) Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 – 2 days, test is set up Sunday - Friday Special Instructions: N/A Specimen Specimen Type: Blood Container: SST (Gold, marble or red) Draw Volume: 6 mL (Minimum: 1.5 mL) blood Processed Volume: 2 mL (Minimum: 0.5 mL) serum Collection: Routine blood collection Special Processing: Lab Staff: Centrifuge specimen and remove serum aliquot into a screw- capped round bottom plastic tube. Store and send serum refrigerated. Forward promptly. Patient Preparation: None Sample Rejection: Specimen collected in incorrect container; specimen other than serum; gross hemolysis; mislabeled or unlabeled specimens Interpretive Reference Range: Complement Fixation/Immunodiffusion test: Mycelial by complement fixation: negative (positives reported as titer) Yeast by complement fixation: negative (positives reported as titer) Antibody by immunodiffusion: negative (positives reported as band present) Complement fixation (CF) titers ≥1:32 indicate active disease. -

Review Article Could Histoplasma Capsulatum Be Related to Healthcare-Associated Infections?
Hindawi Publishing Corporation BioMed Research International Volume 2015, Article ID 982429, 11 pages http://dx.doi.org/10.1155/2015/982429 Review Article Could Histoplasma capsulatum Be Related to Healthcare-Associated Infections? Laura Elena Carreto-Binaghi,1 Lisandra Serra Damasceno,2 Nayla de Souza Pitangui,3 Ana Marisa Fusco-Almeida,3 Maria José Soares Mendes-Giannini,3 Rosely Maria Zancopé-Oliveira,2 and Maria Lucia Taylor1 1 Departamento de Microbiolog´ıa-Parasitolog´ıa,FacultaddeMedicina,UniversidadNacionalAutonoma´ de Mexico´ (UNAM), CircuitoInterior,CiudadUniversitaria,AvenidaUniversidad3000,04510Mexico,´ DF, Mexico 2Instituto Nacional de Infectologia Evandro Chagas, Fundac¸ao˜ Oswaldo Cruz (FIOCRUZ), Avenida Brasil 4365, Manguinhos, 21040-360 Rio de Janeiro, RJ, Brazil 3Departamento de Analises´ Cl´ınicas, Faculdade de Cienciasˆ Farmaceuticas,ˆ Universidade Estadual Paulista (UNESP), Rodovia Araraquara-JauKm1,14801-902Araraquara,SP,Brazil´ Correspondence should be addressed to Maria Lucia Taylor; [email protected] Received 30 October 2014; Revised 12 May 2015; Accepted 12 May 2015 Academic Editor: Kurt G. Naber Copyright © 2015 Laura Elena Carreto-Binaghi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Healthcare-associated infections (HAI) are described in diverse settings. The main etiologic agents of HAI are bacteria (85%) and fungi (13%). Some factors increase the risk for HAI, particularly the use of medical devices; patients with severe cuts, wounds, and burns; stays in the intensive care unit, surgery, and hospital reconstruction works. Several fungal HAI are caused by Candida spp., usually from an endogenous source; however, cross-transmission via the hands of healthcare workers or contaminated devices can occur. -
Cryptococcus Neoformans and Histoplasma Capsulatum in Dove's
MICROBIOLOGÍA ORIGINAL ARTICLE cana de i noamer i and sta Lat Cryptococcus neoformans Histoplasma capsula- i Rev Vol. 48, No. 1 tum in dove’s (Columbia livia) excreta in Bolívar State, January - March. 2006 pp. 6 - 9 Venezuela Julman R. Cermeño,* Isabel Hernández,* Ismery Cabello,** Yida Orellán,* Julmery J. Cer- meño,** Rosa Albornoz,* Elba Padrón,* Gerardo Godoy* ABSTRACT. Dove’s excreta samples from state Bolívar several RESUMEN. Se estudiaron muestras de excretas de palomas obteni- places in Venezuela, were evaluated to determine the presence of das de varios lugares del estado Bolívar, Venezuela, con la finali- primary pathogen fungi in dove’s excreta. Filamentous fungi such dad de determinar la presencia de hongos patógenos primarios. as: Aspergillus spp (31.1%), Mucor spp (20.2%), Penicillium spp Hongos filamentosos tales como: Aspergillus spp (31.1%), Mucor (9.5%) and Fusarium spp (6.7%) were the most frequently isolated spp (20,2%), Penicillium spp (9.5%) y Fusarium spp (6.7%) fue- strains. Species such as Candida albicans (4.1%), Cryptococcus al- ron los aislados más frecuentes. Especies como Candida albicans bidus and Rhodotorula spp (2.7%), C. neoformans var neoformans (4.1%), Cryptococcus albidus y Rhodotorula spp (2.7%), C. neo- (1.4%), Trichosporum asahii (1.4%), Curvularia, Microsporum and formans var neoformans (1.4%), Trichosporum asahii (1.4%), Cur- Phoma as well as Histoplasma capsulatum (1.3%) were less fre- vularia, Microsporum y Phoma, así como de Histoplasma capsula- cuently isolated. This study shows the presence of C. neoformans tum (1.3%) se aislaron con menor frecuencia. Este estudio demostró and H. -

Epidemiology of Histoplasmosis Outbreaks, United States, 1938–2013
Article DOI: http://dx.doi.org/10.3201/eid2203.151117 Epidemiology of Histoplasmosis Outbreaks, United States, 1938–2013 Technical Appendix References for Reported Histoplasmosis Outbreaks by Setting, United States, 1938–2013* Building Bartlett PC, Vonbehren LA, Tewari RP, Martin RJ, Eagleton L, Isaac MJ, et al. Bats in the belfry: an outbreak of histoplasmosis. Am J Public Health. 1982;72:1369–72. http://dx.doi.org/10.2105/AJPH.72.12.1369 Centers for Disease Control and Prevention. Histoplasmosis—Kentucky, 1995. MMWR Morb Mortal Wkly Rep. 1995;44:701–3. Centers for Disease Control and Prevention. Epidemiological reports—histoplasmosis. MMWR Morb Mortal Wkly Rep. 1956;5:1. Centers for Disease Control and Prevention. Epidemiological reports—histoplasmosis. MMWR Morb Mortal Wkly Rep. 1956;5:8. Chick EW, Bauman DS, Lapp NL, Morgan WK. A combined field and laboratory epidemic of histoplasmosis. Isolation from bat feces in West Virginia. Am Rev Respir Dis. 1972;105:968–71. Dean AG, Bates JH, Sorrels C, Sorrels T, Germany W, Ajello L, et al. An outbreak of histoplasmosis at an Arkansas courthouse, with five cases of probable reinfection. Am J Epidemiol. 1978;108:36– 46. Fournier M, Quinlisk P, Garvey A. Histoplasmosis infections associated with a demolition site—Iowa, 2008 [abstract]. Presented at: 58th Annual Epidemic Intelligence Service Conference; 2009 Apr 20–24; Atlanta, Georgia, USA. p. 56–57 [cited 2015 Mar 16]. http://www.cdc.gov/eis/downloads/2009.eis.conference.pdf Page 1 of 8 Gordon MA, Ziment I. Epidemic of acute Histoplasmosis in western New York State. N Y State J Med. -

Chapter 12: Fungi, Algae, Protozoa, and Parasites
I. FUNGI (Mycology) u Diverse group of heterotrophs. u Many are ecologically important saprophytes(consume dead and decaying matter) Chapter 12: u Others are parasites. Fungi, Algae, Protozoa, and u Most are multicellular, but yeasts are unicellular. u Most are aerobes or facultative anaerobes. Parasites u Cell walls are made up of chitin (polysaccharide). u Over 100,000 fungal species identified. Only about 100 are human or animal pathogens. u Most human fungal infections are nosocomial and/or occur in immunocompromised individuals (opportunistic infections). u Fungal diseases in plants cause over 1 billion dollars/year in losses. CHARACTERISTICS OFFUNGI (Continued) CHARACTERISTICS OFFUNGI 2. Molds and Fleshy Fungi 1. Yeasts u Multicellular, filamentous fungi. u Unicellular fungi, nonfilamentous, typically oval or u Identified by physical appearance, colony characteristics, spherical cells. Reproduce by mitosis: and reproductive spores. u Fission yeasts: Divide evenly to produce two new cells u Thallus: Body of a mold or fleshy fungus. Consists of many (Schizosaccharomyces). hyphae. u Budding yeasts: Divide unevenly by budding (Saccharomyces). u Hyphae (Sing: Hypha): Long filaments of cells joined together. Budding yeasts can form pseudohypha, a short chain of u Septate hyphae: Cells are divided by cross-walls (septa). undetached cells. u Coenocytic (Aseptate) hyphae: Long, continuous cells that are not divided by septa. Candida albicans invade tissues through pseudohyphae. Hyphae grow by elongating at the tips. u Yeasts are facultative anaerobes, which allows them to Each part of a hypha is capable of growth. grow in a variety of environments. u Vegetative Hypha: Portion that obtains nutrients. u Reproductive or Aerial Hypha: Portion connected with u When oxygen is available, they carry out aerobic respiration. -

Serious Fungal Infections in Ecuador
Eur J Clin Microbiol Infect Dis DOI 10.1007/s10096-017-2928-5 ORIGINAL ARTICLE Serious fungal infections in Ecuador J. Zurita1,2 & D. W. Denning3 & A. Paz-y-Miño 2 & M. B. Solís2 & L. M. Arias1 Received: 21 December 2016 /Accepted: 21 December 2016 # Springer-Verlag Berlin Heidelberg 2017 Abstract There is a dearth of data from Ecuador on the bur- Pneumocystis pneumonia. The burden of candidemia is den of life-threatening fungal disease entities; therefore, we 1037. Recurrent Candida vaginitis (≥4 episodes per year) af- estimated the burden of serious fungal infections in Ecuador fects 307,593 women aged 15–50 years. Chronic pulmonary based on the populations at risk and available epidemiological aspergillosis probably affects ∼476 patients following tuber- databases and publications. A full literature search was done culosis (TB). Invasive aspergillosis is estimated to affect 748 to identify all epidemiology papers reporting fungal infection patients (∼5.5/100,000). In addition, allergic rates. WHO, ONU-AIDS, Index Mundi, Global Asthma bronchopulmonary aspergillosis (ABPA) in asthma and se- Report, Globocan, and national data [Instituto Nacional de vere asthma with fungal sensitization (SAFS) were estimated Estadística y Censos (INEC), Ministerio de Salud Pública to affect 26,642 and 45,013 people, respectively. Our esti- (MSP), Sociedad de Lucha Contra el Cáncer (SOLCA), mates indicate that 433,856 (3%) of the population in Instituto Nacional de Donación y Trasplante de Órganos, Ecuador is affected by serious fungal infection. Tejidos y Células (INDOT)] were reviewed. When no data existed, risk populations were used to estimate frequencies of fungal infections, using previously described methodology Introduction by LIFE. -

Occurrence of Histoplasmosis in the Indian Sub-Continent: an Overview and Update
REVIEW ARTICLE Occurrence of Histoplasmosis in the Indian Sub-Continent: An Overview and Update https://doi.org/10.20936/jmrp/07/03/02 Harbans S Randhawa* and Harish C Gugnani** ISSN : 2162-6391 (Print) 2162-6375 (Online) ABSTRACT The occurrence of histoplasmosis and its environmental sources of infection are reviewed. It covers the regional distribution of 388 cases of histoplasmosis reported since 1995 to till date. The highest number of cases occurred in West Bengal, followed by Uttar Pradesh, Delhi Union territory (UT), Rajasthan, Maharashtra, Haryana, and Bihar. A sharp rising trend in reporting cases observed in recent years is particularly noteworthy. Also, discussed are the variable clinico-pathological manifestations of 388 cases from India, 20 from Bangladesh, five from Nepal, four from Pakistan, and three from Sri Lanka. Being a primary pathogen, the etiological agent Histoplasma capsulatum can infect immunocompetent as well as the immunocompromised patients. The disease is fatal unless diagnosed early and treated with specific antifungal drugs. It has a predilection for reticuloendothelial system, leading to hepatosplenomegaly, a prominent feature of disseminated histoplasmosis. It poses an ever-increasing threat to public health due to burgeoning population of immunocompromised patients resulting from the spread of AIDS and immunosuppressive therapy in patients undergoing organs transplantation. Non-recognition of the true burden of histoplasmosis in the Indian sub-continent is attributed to possible misdiagnosis as tuberculosis, malignancy or other diseases, and to lack of awareness and inadequate mycological diagnostic facilities. The need for exploring the natural foci of H. capsulatum infections, using molecular techniques, and delineating the endemic zones of histoplasmosis is strongly emphasized. -

Remodeling of the Histoplasma Capsulatum Membrane Induced by Monoclonal Antibodies
Article Remodeling of the Histoplasma Capsulatum Membrane Induced by Monoclonal Antibodies 1, 2, 1 1 Meagan C. Burnet y, Daniel Zamith-Miranda y, Heino M. Heyman , Karl K. Weitz , Erin L. Bredeweg 3, Joshua D. Nosanchuk 2,* and Ernesto S. Nakayasu 1,* 1 Biological Sciences Division, Pacific Northwest National Laboratory, Richland, WA 99352, USA; [email protected] (M.C.B.); [email protected] (H.M.H.); [email protected] (K.K.W.) 2 Department of Microbiology and Immunology and Division of Infectious Diseases, Department of Medicine, Albert Einstein College of Medicine, Bronx, NY 10461, USA; [email protected] 3 Environmental and Molecular Sciences Division, Pacific Northwest National Laboratory, Richland, WA 99352, USA; [email protected] * Correspondence: [email protected] (J.D.N.); [email protected] (E.S.N.) These authors contributed equally to the work. y Received: 24 April 2020; Accepted: 31 May 2020; Published: 2 June 2020 Abstract: Antibodies play a central role in host immunity by directly inactivating or recognizing an invading pathogen to enhance different immune responses to combat the invader. However, the cellular responses of pathogens to the presence of antibodies are not well-characterized. Here, we used different mass spectrometry techniques to study the cellular responses of the pathogenic fungus Histoplasma capsulatum to monoclonal antibodies (mAb) against HSP60, the surface protein involved in infection. A proteomic analysis of H. capsulatum yeast cells revealed that mAb binding regulates a variety of metabolic and signaling pathways, including fatty acid metabolism, sterol metabolism, MAPK signaling and ubiquitin-mediated proteolysis. The regulation of the fatty acid metabolism was accompanied by increases in the level of polyunsaturated fatty acids, which further augmented the degree of unsaturated lipids in H. -

Pathology of Fungal Infection
14/10/56 Pathology of Fungal Infection Julintorn Somran, MD. Growth form of fungi Filamentous or hyphae Yeasts 1 14/10/56 Dimorphic fungi • Presence of both filamentous forms and yeasts in their cycle – Histoplasma spp. • Hyphae at environmental temperatures and yeast form in the body – Candida spp. • Hyphae, pseudohyphae, and yeast form in the body Three types of fungal infection (Mycoses) 1. Superficial mycoses: – Skin, hair, and nails 2. Cutaneous and Subcutaneous mycoses: – deeper layer of skin 3. Systemic or deep mycoses: – internal organ involvement – Including opportunistic infection 2 14/10/56 Superficial mycoses Tinea (Ringworm) Ptyriasis versicolor Cutaneous and Subcutaneous mycoses Eumycotic mycetoma 3 14/10/56 Systemic or deep mycoses Mucormycosis or Zygomycosis Systemic or deep mycoses Pulmonary aspergilllosis 4 14/10/56 Host – Agent relationship Immunocompetent Nosocomial host infection Pathogenic agents Environment Organisms Host Infectious disease Impaired Defense mechanism Immunocompromise Opportunistic host infection Superficial mycoses Representative Causative Growth form disease organisms in Tissue Dermatophytosis Microsporum, Filamentous form Trichophyton, and Epidermophyton Pityriasis versicolor or Malassezia Yeast and filamentous skin infection via form malassezia Tinea nigra or Exophialia Filamentous form keratomycosis nigrican (Phaeoanellomyces) (pigmented) palmaris wernekii Onychomycosis Microsporum, Filamentous form Trichophyton, Epidermophyton etc. 5 14/10/56 DERMATOPHYTOSIS • Definition and Epidemiology: – Common superficial infection caused by fungi that able to invade keratinized tissue – stratum corneum, hair, and nails. – World wide in distribution – The source of infection – another person, animal or soil • Etiologic agents: – Microsporum, Trichophyton, and Epidermophyton – T rubrum – most common for tinea pedis and onychomycosis in temperate climate, and tinea cruris and tinea corporis in the tropics.