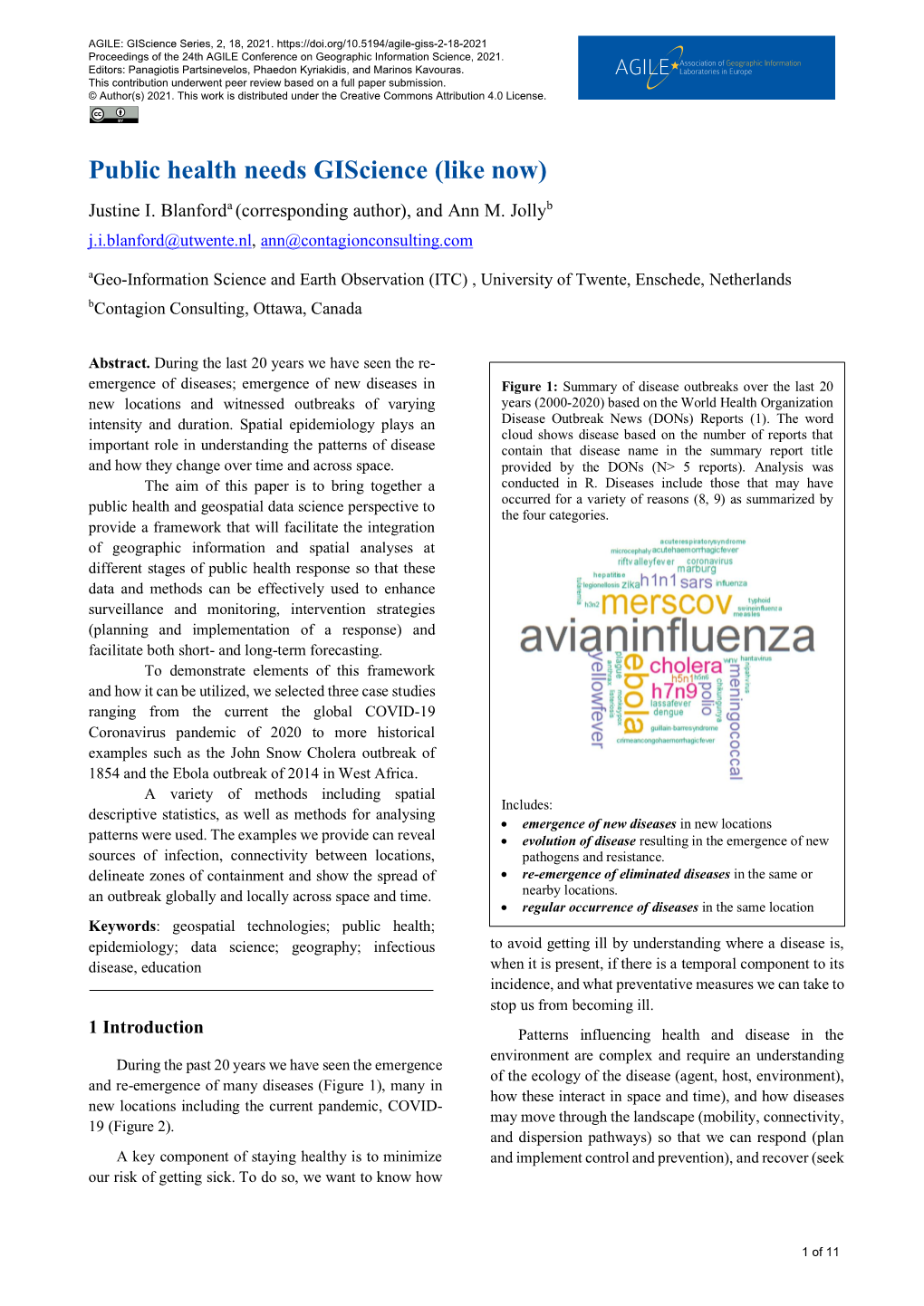
Public Health Needs Giscience (Like Now) Justine I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

On Epidemiology and Geographic Information Systems: a Review and Discussion of Future Directions Keith C
Perspectives On Epidemiology and Geographic Information Systems: A Review and Discussion of Future Directions Keith C. Clarke, Ph.D., Sara L. McLafferty, Ph.D,. and Barbara J. Tempalski Hunter College-CUNY, New York, New York, USA Geographic information systems are powerful automated systems for the capture, stor- age, retrieval, analysis, and display of spatial data. While the systems have been in development for more than 20 years, recent software has made them substantially easier to use for those outside the field. The systems offer new and expanding opportunities for epidemiology because they allow an informed user to choose between options when geographic distributions are part of the problem. Even when used minimally, these systems allow a spatial perspective on disease. Used to their optimum level, as tools for analysis and decision making, they are indeed a new information management vehicle with a rich potential for public health and epidemiology. Geographic information systems (GIS) are Computers were first applied to geography as “automated systems for the capture, storage, re- analytical and display tools during the 1960s (3). trieval, analysis, and display of spatial data” (1). GIS emerged as a multidisciplinary field during Common to all GIS is a realization that spatial the 1970s. The discipline’s heritage lies in cartog- data are unique because their records can be raphy’s mathematical roots: in urban planning’s linked to a geographic map. The component parts map overlay methods for selecting regions and of a GIS include not just a database, but also locations based on multiple factors (4); in the im- spatial or map information and some mechanism pact of the quantitative revolution on the disci- to link them together.GIS has also been described pline of geography; and in database management as the technology side of a new discipline, geo- developments in computer science. -

Public Health GIS News and Information, No. 44 (January 2002)
PUBLIC HEALTH GIS NEWS AND INFORMATION January 2002 (No. 44) Dedicated to CDC/ATSDR scientific excellence and advancement in disease control and prevention using GIS Selected Contents: Events Calendar (pp.1-2); News from GIS Users (pp.2-6); GIS Outreach (pp.6-7); Public Health and GIS Literature (pp.7-17); DHHS and Federal Update (pp.17- 21); Website(s) of Interest (pp.21-22); Final Thoughts (pp.22-24) I. Public Health GIS (and related)Events Austin, Texas [See site: http://www.tnris.state.tx.us/gis SPECIAL NCHS/CDC/ATSDR GIS LECTURES festival] FEBRUARY 12, 2002. “Mapping Community- � Level Housing and Related Data on the Web at the Fifth Annual International Conference: Map India Department of Housing and Urban Development 2002, February 6-8, 2002, New Delhi, India [See: (HUD)” by Jon Sperling and David Chase, U.S. http://www.mapindia.org] Department of Housing and Urban Development � th (HUD), from 2:00-3:30PM. This NCHS Cartography 8 Biennial Symposium on Minorities, the and GIS Guest Lecture Series programs will be held at Medically Underserved & Cancer, February 6-10, the NCHS Auditorium, RM1100, Hyattsville, MD; 2002, Washington, D.C. [See: http://www.iccnetwork. Envision is available to offsite CDC/ATSDR org] locations; Web access is available to all others at � http://video.cdc.gov/ramgen/envision/live.rm (link GIS and Crime Science Conference, February 14, becomes active approximately 30 minutes prior to the 2002, University of London, London, England [See: event and viewing requires RealPlayer http://www.ucl.ac.uk/spp/jdi/events_pubs.htm] installation).See abstract for presentations in this � edition. -

Public Health GIS News and Information, No. 43 (November 2001)
PUBLIC HEALTH GIS NEWS AND INFORMATION November 2001 (No. 43) Dedicated to CDC/ATSDR scientific excellence and advancement in disease control and prevention using GIS Selected Contents: Events Calendar (pp.1-2); News from GIS Users (pp.2-8); GIS Outreach (p.8); Public Health and GIS Literature (pp.8-15); DHHS and Federal Update (pp.16- 22); Website(s) of Interest (pp.22-24); Final Thoughts (pp.24-25) I. Public Health GIS (and related)Events [Note: Calendar events are posted as received; for a more complete SPECIAL NCHS/CDC/ATSDR GIS LECTURES: listing see prior two bimonthly reports at NCHS GIS website] K "GIS In Telecoms 2001," The Open GIS 14th Annual Geography Awareness Week Consortium, Inc. (OGC) (Wayland, MA) and IIR NOVEMBER 27, 2001 “GIS and Lyme Disease: Conferences-UK (UK), November 12-15, 2001, Exploring Space-Time Relationships with Geneva, Switzerland [See: http://www.iir-conferences. Geostatistics,” by Lee De Cola, Geographer and com] Mathematician, U.S. Geological Survey and Charles M. Croner, Geographer and Survey Statistician, L GIS Day 2001: “Discovering the World through Office of Research and Methodology, NCHS, CDC, GIS,” November 14, 2001 [See: http://www.gisday. from 2:00-3:30PM. com] NOVEMBER 29, 2001. “LandView V: A Federal Spatial Data Viewer,” by E. J. (Jerry) McFaul, K First Annual ESRI Health Conference, November Computer Scientist, U.S. Geological Survey, and and 12-14, 2001, Washington, DC [See: http://www.esri. Peter Gattuso, Information Management Specialist at com] the Environmental Protection Agency, from -

Model Geographic Information System Infrastructure for Local Health Departments in Connecticut
University of Connecticut OpenCommons@UConn UCHC Graduate School Masters Theses 2003 - University of Connecticut Health Center Graduate 2010 School June 2005 Model geographic Information System Infrastructure for Local Health Departments in Connecticut. Lemuel Skidmore Follow this and additional works at: https://opencommons.uconn.edu/uchcgs_masters Recommended Citation Skidmore, Lemuel, "Model geographic Information System Infrastructure for Local Health Departments in Connecticut." (2005). UCHC Graduate School Masters Theses 2003 - 2010. 103. https://opencommons.uconn.edu/uchcgs_masters/103 MODEL GEOGRAPHIC INFORMATION SYSTEM INFRASTRUCTURE FOR LOCAL HEALTH DEPARTMENTS IN CONNECTICUT Lemuel Skidmore B.A., Hawthorne College, 1972 M.S., Indiana State University, 1975 A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Public Health at the University of Connecticut 2005 APPROVAL PAGE Master of Public Health Thesis Model Geographic Information System Infrastructure for Local Health Departments in Connecticut Presented by Lemuel Skidmore, M.S. Major Advisor Timothy F. Morse Associate Advisor Paul M. Schur Associate Advisor Barbara Blechner Associate Advisor Ellen K. Cromley University of Connecticut 2005 ACKNOWLEDGEMENTS I need to thank many people for their support in developing this thesis. I apologize to those whom I missed. First are my advisors" Tim Morse for accepting me as an advisee and guiding me through the process, Paul Schur for helping me chase my idea balloons, Barbara B lechner for her -

Using Web GIS for Public Health Education
INTERNATIONAL JOURNAL OF ENVIRONMENTAL & SCIENCE EDUCATION 2016, VOL. 11, NO. 14, 6314-6333 OPEN ACCESS Using Web GIS for Public Health Education Rajika E. Reeda and Alec M. Bodzina aLehigh University, USA ABSTRACT An interdisciplinary curriculum unit that used Web GIS mapping to investigate malaria disease patterns and spread in relation to the environment for a high school Advanced Placement Environmental Science course was developed. A feasibility study was conducted to investigate the efficacy of the unit to promote geospatial thinking and reasoning skills and content understandings. Results revealed increased content understandings and significant effect sizes for all three geospatial thinking and reasoning subscales - inferences, relationships, and reasoning. The findings provide support that Web GIS, with appropriate curriculum design can improve both learning outcomes and geospatial thinking and reasoning skills. KEYWORDS ARTICLE HISTORY curriculum design, disease patterns, geospatial Received 10 March 2016 thinking, public health education, Web GIS Revised 10 May 2016 Accepted 22 May 2016 Introduction Maps allow for the synthesis of many abstract concepts, such as global disease patterns and their relationship to environmental and demographic factors for increased public health literacy through visualization (Riner, Cunningham, & Johnson, 2004). A Geographic Information System (GIS) provides a platform for this visualization through dynamic mapping. GIS differs from traditional paper maps in that it is a mapping system that allows data to be analyzed, manipulated, and interpreted through the use of layers. This leads to data map visualizations that facilitate understanding the relationships, patterns and trends among georeferenced data (Baker et al., 2015). Web-based GIS (referred to as Web GIS) is a form of GIS that is deployed using an Internet Web browser. -
GIS and Public Health Geographic Information Systems (Giss) Concentrate on Combining Computer Mapping Capabilities with Database Management and Analysis Tools
GIS and Public Health Geographic information systems (GISs) concentrate on combining computer mapping capabilities with database management and analysis tools. GIS systems include many applications , including the transportation of people and objects, environmental sciences, urban planning, agricultural applications, and so on. Public health is one of the most important topics that has seen an increased use of GIS. Geographical studies are playing an important role in public health and health services planning. In general, public health differs from personal health in the following regards: (1) it is focused on the health of populations rather than of individuals, (2) it is focused more on prevention than on treatment, (3) it operates in a mainly governmental (rather than private) context.[1] These efforts fall naturally within the domain of problems requiring the use of spatial analysis as part of the solution, and GIS and other spatial analysis tools are therefore recognized as providing potentially transformational capabilities for public health efforts. This ppt presents some history of the use of geographic information and geographic information systems in public health application areas, provides some examples showing the utilization of GIS techniques in solving specific public health problems, and finally addresses several potential issues arising from an increased use of these GIS techniques in the public health arena. History Public health efforts have been based on analysis and use of spatial data for many years. Dr. John Snow (physician), often credited as the father of epidemiology, is arguably the most famous of those examples.[2] Dr. Snow focused on a map which overlaid cholera deaths with the locations of public water supplies . -

GEP 610 Spatial Analysis of Urban Health
DRAFT SYLLABUS Lehman College, City University of New York Department of Earth, Environmental, and Geospatial Sciences GEP 610/EES 79903/PUBH 85100: Spatial Analysis of Urban Health Spring 2016 Course Description: This course focuses on urban health issues using a geographical framework and covers topics such as the historical perspective of health, place, and society; mapping and measuring health and health impacts; the social and spatial patterning of health; the geography of health inequalities and disparities; health and social/spatial mobility; and the effects of urban segregation, overcrowding, and poverty on disease. Current research, as well as the seminal early works on the geographies of health, will be reviewed. Geographic Information Science will be used in the laboratory exercises to illustrate the theoretical concepts and to produce worked examples of health geography. 3 credits, 4 hours Course Meets: Gillet Hall, Room 311 (classroom) Fridays, once per month, from 4:00 – 6:00 PM, dates as noted below. Instructors: Profs. Juliana Maantay and Andrew Maroko Emails: [email protected] [email protected] Phones: 718 960-8574 (JAM) 718 960-1830 (ARM) Office: GIllet Hall, Room 325 (JAM) Gillet Hall, Room 323 (ARM) Office Hours: Wednesdays, 2:00-4:00 PM and by appointment (JAM) Wednesdays, 3:00-5:00 PM and by appointment (ARM) Required Textbooks: . Shaw, Dorling, Mitchell, 2001. Health, Place, and Society (Open Access book - will be available in pdf on Blackboard) . Koch, T., 2005. Cartographies of Disease: Maps, Mapping, and Medicine, ESRI Press . Gatrell, A. and Elliott, S., 2009. Geographies of Health, 2nd Edition, Wiley-Blackwell . -

Gis in Epidemiology: Applications and Services
pISSN: 0976 3325 eISSN: 2229 6816 ORIGINAL ARTICLE GIS IN EPIDEMIOLOGY: APPLICATIONS AND SERVICES Bhatt Bindu M1, Joshi Janak P2 1Associate Professor, 2Senior Research Fellow, Department of Geography, Faculty of Science, The Maharaja Sayajirao University of Baroda, Vadodara, Gujarat ABSTRACT There is a growing understanding and appreciation regarding the power of health and health-related information in planning and implementing health programs. Given these points and the fact that most health information is tied in some way to geography, it is becoming increasingly important that health professionals, organizations, and communities create systems that empower them to really take advantage of the many different types of information that is available and that can be brought to bare on health issues and program management. There are countless layers or types of health and health-related data for a given population or place. GIS allow people to organize, visualize, and analyze these data layers more effectively. GIS and related spatial analysis methods provide a set of tools for describing and understanding the changing spatial organization of health care, for examining its relationship to health outcomes and access, and for exploring how the delivery of health care can be improved. Geographic information systems (GIS) provide ideal platforms for the convergence of disease-specific information and their analyses in relation to population settlements, surrounding social and health services and the natural environment. They are highly suitable for analysing epidemiological data, revealing trends and interrelationships that would be more difficult to discover in tabular format. Moreover GIS allows policy makers to easily visualize problems in relation to existing health and social services and the natural environment and so more effectively target resources. -

Public Health GIS News and Information, No. 70 (May 2006)
PUBLIC HEALTH GIS NEWS AND INFORMATION May 2006 (No. 70) Dedicated to CDC GIS Scientific Excellence and Advancement in Disease, Injury and Disability Control and Prevention, and Biologic, Chemical and Occupational Safety Selected Contents: Events Calendar (pp.1-2); News from GIS Users (pp.2-9); GIS Outreach (pp. 9-10); Public Health and GIS Literature (pp.10-15); DHHS and Federal Update (pp.15• 20); Website(s) of Interest (pp. 20-21); Final Thoughts (pp.21-22); MAP Appendix (23-25) I. Public Health GIS (and related) Events: SPECIAL NCHS/CDC GIS LECTURES Institutes in Public Policy, May 10-12, 2006, New Orleans, LA [See: http://www.nnphi.org/conf.htm] June 15, 2006: “The National Neighborhood Indicators Partnership (NNIP)- Advances in the * Cancer in African Americans-Opportunities and Development and Use of Neighborhood Level Data,” Challenges, Cancer Symposium, May 11-13, 2006, by researcher G. Thomas Kingsley, The Urban Institute, Cleveland OH [See symposium site and registration at: Washington, D.C., 2:00-3:00PM (EST), and live at [https://www.clevelandclinicmeded.com/summit/afcancer06/description.htm] NCHS. The NCHS GIS Guest Lecture Series has been presented continuously at NCHS since 1988. As with all * Overcoming Health Disparities: The Changing live lectures, Envision (live interactive) will be available Landscape, NY Academy of Medicine, May12-13, 2006, to offsite CDC locations as well as IPTV. Web access New York, NY [See: http://www.mecme.org] will be available to our national and worldwide public health audience. The cosponsors to the NCHS * American Society of Health Economists (ASHE) Cartography and GIS Guest Lecture Series include Conference: Economics of Population Health, June 4-7, CDC’s Behavioral and Social Science Working Group 2006, Madison, WI [See: http://healtheconomics.us] (BSSWG) and Statistical Advisory Group (SAG). -

Public Health Interventions: Applications for Public Health Nursing Practice SECOND EDITION
Public health interventions: Applications for public health nursing practice SECOND EDITION 2019 Public health interventions: Applications for public health nursing practice Second edition Marjorie Schaffer, PhD, RN, PHN Susan Strohschein, DNP, RN, PHN (retired) Suggested citation: Minnesota Department of Health. (2019). Public health interventions: Applications for public health nursing practice (2nd ed.). Minnesota Department of Health Community Health Division PO Box 64975 St. Paul, MN 55164-0975 651-201-3880 [email protected] www.health.state.mn.us To obtain this information in a different format, call: 651-201-3880. Contents Acknowledgements .............................................................................................................................................. 5 Foreword ............................................................................................................................................................... 7 Introduction .......................................................................................................................................................... 8 Overview of evidence-based practice and related topics .............................................................................. 17 Red wedge .......................................................................................................................................................... 25 Surveillance ................................................................................................................................................... -
Advanced Health Information Sharing with Web-Based Gis
ADVANCED HEALTH INFORMATION SHARING WITH WEB-BASED GIS SHENG GAO March 2010 TECHNICAL REPORT NO. 272 ADVANCED HEALTH INFORMATION SHARING WITH WEB-BASED GIS Sheng Gao Department of Geodesy and Geomatics Engineering University of New Brunswick P.O. Box 4400 Fredericton, N.B. Canada E3B 5A3 March 2010 © Sheng Gao, 2010 PREFACE This technical report is a reproduction of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Geodesy and Geomatics Engineering, March 2010. The research was supervised by Dr. David Coleman and Dr. Harold Boley, and funding was provided by the GeoConnections Secretariat of Natural Resources Canada. As with any copyrighted material, permission to reprint or quote extensively from this report must be received from the author. The citation to this work should appear as follows: Gao, S. (2010). Advanced Health Information Sharing with Web-Based GIS. Ph.D. dissertation, Department of Geodesy and Geomatics Engineering, Technical Report No. 272, University of New Brunswick, Fredericton, New Brunswick, Canada, 188 pp. ABSTRACT Web-based GIS is increasingly utilized in health organizations to share and visualize georeferenced health data through the Web. In the development of a public information and disease surveillance network, issues of data publishing and user access are important concerns. The handling of data heterogeneity, lack of available data and tools, and methods of health information representation constitute continuing challenges. The purpose of this research is to address these three problems and provide new solutions for health information sharing. Regarding data heterogeneity, a geospatial-enabled RuleML method has been designed for semantic disease information queries. -
Geographic Information Systems for Spatial Disease Cluster
GEOGRAPHIC INFORMATION SYSTEMS FOR SPATIAL DISEASE CLUSTER DETECTION, SPATIO-TEMPORAL DISEASE MAPPING, AND HEALTH SERVICE PLANNING by PING YIN (Under the Direction of Lan Mu and Marguerite Madden) ABSTRACT Geographic information systems (GIS) are increasingly recognized as an effective and efficient tool to deal with geographic questions in health studies. The overarching research question of this dissertation asks how GIS and spatial analysis can be used to facilitate public health studies. Three aspects of health studies are included: spatial disease cluster detection, spatio-temporal disease mapping, and health service planning. New methods or models are proposed and implemented with GIS in this dissertation to address an important problem in each of the three aspects. First, a redesigned spatial scan statistic (RSScan) is proposed to quickly detect disease clusters in arbitrary shapes. The experimental results indicate that the improved RSScan method generally has higher power and accuracy than three existing methods for detecting the clusters in irregular shapes. Second, to explore the spatio-temporal patterns of lung cancer incidence risks in Georgia between 2000 and 2007, a total of seven hierarchical Bayesian models are developed and compared at the census tract level using a two-year time period as the temporal unit. The study shows the northwest region of Georgia has stably elevated lung cancer incidence risks for all the population groups by race and sex. It also shows that there are strong inverse relationships between socioeconomic status and lung cancer incidence risk in males and weak inverse relationships in females in Georgia. Finally, two transportation models that address the modular capacitated maximal covering location problem (MCMCLP) are proposed and used to optimally site ambulances for Emergency Medical Services (EMS) Region 10 in Georgia.